Abstract
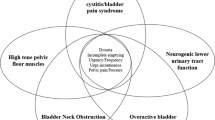
In this review, the current literature regarding pharmacotherapy treatment strategies available for the management of interstitial cystitis/bladder pain syndrome in older adults is addressed. The focus is on those treatments described by the American Urologic Association guidelines, organized according to clinical phenotype. Symptoms at presentation can vary with age, with older adults being more likely to experience nocturia, urinary incontinence, and Hunner’s lesions than their younger counterparts. As such, treatment of interstitial cystitis/bladder pain syndrome should follow an individualized multimodal plan based on the patient’s unique phenotype(s), starting with the most conservative options and escalating as needed. The side-effect profile and medication interactions should be reviewed, especially when treating older adults, requesting the aid of pharmacists or the primary care physician as needed to safely provide treatment.

Similar content being viewed by others
References
Hanno PM, Erickson D, Moldwin R, Faraday MM, American Urological Association. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53.
Hanno P, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourol Urodyn. 2009;28(4):274–86.
Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010;57(1):35–48.
Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186(2):540–4.
Clemens JQ, Meenan RT, O’Keeffe Rosetti MC, Brown SO, Gao SY, Calhoun EA. Prevalence of interstitial cystitis symptoms in a managed care population. J Urol. 2005;174(2):576–80.
Rais-Bahrami S, Friedlander JI, Herati AS, Sadek MA, Ruzimovsky M, Moldwin RM. Symptom profile variability of interstitial cystitis/painful bladder syndrome by age. BJU Int. 2012;109(9):1356–9.
Richter B, Hesse U, Hansen AB, Horn T, Mortensen SO, Nordling J. Bladder pain syndrome/interstitial cystitis in a Danish population: a study using the 2008 criteria of the European Society for the Study of Interstitial Cystitis. BJU Int. 2010;105(5):660–7.
Lee M-H, Chang K-M, Tsai W-C. Morbidity rate and medical utilization in interstitial cystitis/painful bladder syndrome. Int Urogynecol J. 2018;29(7):1045–50.
Clemens JQ, Mullins C, Ackerman AL, Bavendam T, van Bokhoven A, Ellingson BM, et al. Urologic chronic pelvic pain syndrome: insights from the MAPP Research Network. Nat Rev Urol. 2019;16(3):187–200.
Crane A, Lloyd J, Shoskes DA. Improving the utility of clinical phenotyping in interstitial cystitis/painful bladder syndrome: from UPOINT to INPUT. Can J Urol. 2018;25(2):9250–4.
Andersson K-E, Boedtkjer DB, Forman A. The link between vascular dysfunction, bladder ischemia, and aging bladder dysfunction. Ther Adv Urol. 2017;9(1):11–27.
Pinggera G-M, Mitterberger M, Pallwein L, Schuster A, Herwig R, Frauscher F, et al. Alpha-blockers improve chronic ischaemia of the lower urinary tract in patients with lower urinary tract symptoms. BJU Int. 2008;101(3):319–24.
Nomiya M, Yamaguchi O, Andersson K-E, Sagawa K, Aikawa K, Shishido K, et al. The effect of atherosclerosis-induced chronic bladder ischemia on bladder function in the rat. Neurourol Urodyn. 2012;31(1):195–200.
Cox A, Golda N, Nadeau G, Curtis Nickel J, Carr L, Corcos J, et al. CUA guideline: diagnosis and treatment of interstitial cystitis/bladder pain syndrome. Can Urol Assoc J. 2016;10(5–6):E136–55.
Abrams P, Andersson K-E, Apostolidis A, Birder L, Bliss D, Brubaker L, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2.
Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018;122(5):729–43.
Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. 2017;33(3):293–303.
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–7.
Theou O, Walston J, Rockwood K. Operationalizing frailty using the frailty phenotype and deficit accumulation approaches. Interdiscip Top Gerontol Geriatr. 2015;41:66–73.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–8.
Atchley MD, Shah NM, Whitmore KE. Complementary and alternative medical therapies for interstitial cystitis: an update from the United States. Transl Androl Urol. 2015;4(6):662–7.
Gordon B, Shorter B, Sarcona A, Moldwin RM. Nutritional considerations for patients with interstitial cystitis/bladder pain syndrome. J Acad Nutr Diet. 2015;115(9):1372–9.
Cho SY, Lee SL, Kim IS, Koo DH, Kim H, Oh S-J. Short-term effects of systematized behavioral modification program for nocturia: a prospective study. Neurourol Urodyn. 2012;31(1):64–8.
FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, et al. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. J Urol. 2012;187(6):2113–8.
Kim A, Keyong-Ok H, Shin JH, Choo M-S. Evaluation of the incidence and risk factors associated with persistent frequency in interstitial cystitis/bladder pain syndrome and the efficacy of antimuscarinic treatment. Investig Clin Urol. 2017;58(5):353–8.
Elliott C, Payne CK. Interstitial cystitis and the overlap with overactive bladder. Curr Urol Rep. 2012;13(5):319–26.
Anger J, Zabihi N, Clemens JQ, Payne CK, Saigal LVR. Treatment choice, duration, and cost in patients with interstitial cystitis and painful bladder syndrome. Int Urogynecol J. 2011;22(4):395–400.
Suskind AM, Quanstrom K, Zhao S, Bridge M, Walter LC, Neuhaus J, et al. Overactive bladder is strongly associated with frailty in older individuals. Urology. 2017;106:26–31.
American Geriatrics Society Beers Criteria Update Expert Panel 2019. American Geriatrics Society 2019 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
Coupland CAC, Hill T, Dening T, Morriss R, Moore M, Hippisley-Cox J. Anticholinergic drug exposure and the risk of dementia. JAMA Intern Med. 2019;179(8):1084.
Green AR, Reifler LM, Bayliss EA, Weffald LA, Boyd CM. Drugs contributing to anticholinergic burden and risk of fall or fall-related injury among older adults with mild cognitive impairment, dementia and multiple chronic conditions: a retrospective cohort study. Drugs Aging. 2019;36(3):289–97.
Orme S, Morris V, Gibson W, Wagg A. Managing urinary incontinence in patients with dementia: pharmacological treatment options and considerations. Drugs Aging. 2015;32(7):559–67.
Di Lena M, Tolls V, Kelly K-L, Nickel JC. Mirabegron as adjuvant treatment for patients with interstitial cystitis/bladder pain syndrome. Can Urol Assoc J. 2017;12(3):E100–4.
Gauthier C, Leblais V, Kobzik L, Trochu JN, Khandoudi N, Bril A, et al. The negative inotropic effect of beta3-adrenoceptor stimulation is mediated by activation of a nitric oxide synthase pathway in human ventricle. J Clin Investig. 1998;102(7):1377–84.
Kelleher C, Hakimi Z, Zur R, Siddiqui E, Maman K, Aballéa S, et al. Efficacy and tolerability of mirabegron compared with antimuscarinic monotherapy or combination therapies for overactive bladder: a systematic review and network meta-analysis. Eur Urol. 2018;74(3):324–33.
Tadrous M, Matta R, Greaves S, Herschorn S, Mamdani MM, Juurlink DN, et al. Association of mirabegron with the risk of arrhythmia in adult patients 66 years or older: a population-based cohort study. JAMA Intern Med. 2019;179(10):1436.
Anderson VR, Perry CM. Pentosan polysulfate: a review of its use in the relief of bladder pain or discomfort in interstitial cystitis. Drugs. 2006;66(6):821–35.
Sairanen J, Hotakainen K, Tammela TLJ, Stenman U-H, Ruutu M. Urinary epidermal growth factor and interleukin-6 levels in patients with painful bladder syndrome/interstitial cystitis treated with cyclosporine or pentosan polysulfate sodium. Urology. 2008;71(4):630–3.
Parsons CL. Bladder surface glycosaminoglycan: efficient mechanism of environmental adaptation. Urology. 1986;27(2 Suppl.):9–14.
Holm-Bentzen M, Jacobsen F, Nerstrøm B, Lose G, Kristensen JK, Pedersen RH, et al. A prospective double-blind clinically controlled multicenter trial of sodium pentosanpolysulfate in the treatment of interstitial cystitis and related painful bladder disease. J Urol. 1987;138(3):503–7.
Mulholland SG, Hanno P, Parsons CL, Sant GR, Staskin. Pentosan polysulfate sodium for therapy of interstitial cystitis. A double-blind placebo-controlled clinical study. Urology. 1990;35(6):552–8.
Parsons CL, Benson G, Childs SJ, Hanno P, Sant GR, Webster G. A quantitatively controlled method to study prospectively interstitial cystitis and demonstrate the efficacy of pentosanpolysulfate. J Urol. 1993;150(3):845–8.
Sant GR, Propert KJ, Hanno PM, Burks D, Culkin D, Diokno AC, et al. A pilot clinical trial of oral pentosan polysulfate and oral hydroxyzine in patients with interstitial cystitis. J Urol. 2003;170(3):810–5.
van Ophoven A, Vonde K, Koch W, Auerbach G, Maag KP. Efficacy of pentosan polysulfate for the treatment of interstitial cystitis/bladder pain syndrome: results of a systematic review of randomized controlled trials. Curr Med Res Opin. 2019;35(9):1495–503
Pearce WA, Chen R, Jain N. Pigmentary maculopathy associated with chronic exposure to pentosan polysulfate sodium. Ophthalmology. 2018;125(11):1793–802.
Hanif AM, Shah R, Yan J, Varghese JS, Patel SA, Cribbs BE, et al. Strength of association between pentosan polysulfate and a novel maculopathy. Ophthalmology. 2019;126(10):1464–6.
Jain N, Li AL, Yu Y, VanderBeek BL. Association of macular disease with long-term use of pentosan polysulfate sodium: findings from a US cohort. Br J Ophthalmol. 2019;104(8):1093–7
Ferguson TJ, Geraets RL, Barker MA. Chronic use of pentosan polysulfate sodium associated with risk of vision-threatening disease. Int Urogynecol J. 2019;30(3):337–8.
Rovner E, Propert KJ, Brensinger C, Wein AJ, Foy M, Kirkemo A, et al. Treatments used in women with interstitial cystitis: the interstitial cystitis data base (ICDB) study experience: the Interstitial Cystitis Data Base Study Group. Urology. 2000;56(6):940–5.
Aizawa N, Wyndaele J-J. Effects of phenazopyridine on rat bladder primary afferent activity, and comparison with lidocaine and acetaminophen. Neurourol Urodyn. 2010;29(8):1445–50.
Lusty A, Kavaler E, Zakariasen K, Tolls V, Nickel JC. Treatment effectiveness in interstitial cystitis/bladder pain syndrome: do patient perceptions align with efficacy-based guidelines? Can Urol Assoc J. 2018;12(1):E1–5.
Singh M, Shailesh F, Tiwari U, Sharma SG, Malik B. Phenazopyridine associated acute interstitial nephritis and review of literature. Ren Fail. 2014;36(5):804–7.
Sant GR, LaRock DR. Standard intravesical therapies for interstitial cystitis. Urol Clin N Am. 1994;21(1):73–83.
Perez-Marrero R, Emerson LE, Feltis JT. A controlled study of dimethyl sulfoxide in interstitial cystitis. J Urol. 1988;140(1):36–9.
Tutolo M, Ammirati E, Castagna G, Klockaerts K, Plancke H, Ost D, et al. A prospective randomized controlled multicentre trial comparing intravesical DMSO and chondroïtin sulphate 2% for painful bladder syndrome/interstitial cystitis. Int Braz J Urol. 2017;43(1):134–41.
Cervigni M, Sommariva M, Tenaglia R, Porru D, Ostardo E, Giammò A, et al. A randomized, open-label, multicenter study of the efficacy and safety of intravesical hyaluronic acid and chondroitin sulfate versus dimethyl sulfoxide in women with bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2017;36(4):1178–86.
Iyer S, Lotsof E, Zhou Y, Tran A, Botros C, Sand P, et al. Which bladder instillations are more effective? DMSO vs. bupivacaine/heparin/triamcinolone: a retrospective study. Int Urogynecol J. 2017;28(9):1335–40.
Rawls WF, Cox L, Rovner ES. Dimethyl sulfoxide (DMSO) as intravesical therapy for interstitial cystitis/bladder pain syndrome: a review. Neurourol Urodyn. 2017;36(7):1677–84.
Chintea CL, Belal M. Is there enough evidence for the use of intravesical instillations of glycosaminoglycan analogues in interstitial cystitis? BJU Int. 2013;111(2):192–3.
Barua JM, Arance I, Angulo JC, Riedl CR. A systematic review and meta-analysis on the efficacy of intravesical therapy for bladder pain syndrome/interstitial cystitis. Int Urogynecol J. 2016;27(8):1137–47.
Nickel JC, Egerdie RB, Steinhoff G, Palmer B, Hanno P. A multicenter, randomized, double-blind, parallel group pilot evaluation of the efficacy and safety of intravesical sodium chondroitin sulfate versus vehicle control in patients with interstitial cystitis/painful bladder syndrome. Urology. 2010;76(4):804–9.
Nickel JC, Hanno P, Kumar K, Thomas H. Second multicenter, randomized, double-blind, parallel-group evaluation of effectiveness and safety of intravesical sodium chondroitin sulfate compared with inactive vehicle control in subjects with interstitial cystitis/bladder pain syndrome. Urology. 2012;79(6):1220–4.
Thakkinstian A, Nickel JC. Efficacy of intravesical chondroitin sulphate in treatment of interstitial cystitis/bladder pain syndrome (IC/BPS): individual patient data (IPD) meta-analytical approach. Can Urol Assoc J. 2013;7(5–6):195–200.
Hanno PM, Parsons CL, Shrom SH, Fritz R, Mulholland SG. The protective effect of heparin in experimental bladder infection. J Surg Res. 1978;25(4):324–9.
Parsons CL, Zupkas P, Proctor J, Koziol J, Franklin A, Giesing D, et al. Alkalinized lidocaine and heparin provide immediate relief of pain and urgency in patients with interstitial cystitis. J Sex Med. 2012;9(1):207–12.
Perez-Marrero R, Emerson LE, Maharajh DO, Juma S. Prolongation of response to DMSO by heparin maintenance. Urology. 1993;41(1 Suppl.):64–6.
Meng E, Hsu Y-C, Chuang Y-C. Advances in intravesical therapy for bladder pain syndrome (BPS)/interstitial cystitis (IC). Low Urin Tract Symptoms. 2018;10(1):3–11.
Chuang Y-C, Yoshimura N, Huang C-C, Chiang P-H, Chancellor MB. Intravesical botulinum toxin A administration produces analgesia against acetic acid induced bladder pain responses in rats. J Urol. 2004;172(4 Part 1):1529–32.
Rapp DE, Turk KW, Bales GT, Cook SP. Botulinum toxin type A inhibits calcitonin gene-related peptide release from isolated rat bladder. J Urol. 2006;175(3):1138–42.
Lee B-J, Jeong J-H, Wang S-G, Lee J-C, Goh E-K, Kim H-W. Effect of botulinum toxin type A on a rat surgical wound model. Clin Exp Otorhinolaryngol. 2009;2(1):20.
Lucioni A, Bales GT, Lotan TL, McGehee DS, Cook SP, Rapp DE. Botulinum toxin type A inhibits sensory neuropeptide release in rat bladder models of acute injury and chronic inflammation. BJU Int. 2008;101(3):366–70.
Pang X, Marchand J, Sant GR, Kream RM, Theoharides TC. Increased number of substance P positive nerve fibres in interstitial cystitis. Br J Urol. 1995;75(6):744–50.
Smith CP, Radziszewski P, Borkowski A, Somogyi GT, Boone TB, Chancellor MB. Botulinum toxin a has antinociceptive effects in treating interstitial cystitis. Urology. 2004;64(5):871–5.
Kuo H-C, Chancellor MB. Comparison of intravesical botulinum toxin type A injections plus hydrodistention with hydrodistention alone for the treatment of refractory interstitial cystitis/painful bladder syndrome. BJU Int. 2009;104(5):657–61.
Kuo H-C. Repeated onabotulinumtoxin-A injections provide better results than single injection in treatment of painful bladder syndrome. Pain Physician. 2013;16(1):15–23.
Jhang J-F, Jiang Y-H, Kuo H-C. Potential therapeutic effect of intravesical botulinum toxin type A on bladder pain syndrome/interstitial cystitis. Int J Urol. 2014;21:49–55.
Przydacz M, Golabek T, Chlosta P. How to assess and predict success or failure of intra-detrusor injections with onabotulinumtoxinA. Adv Clin Exp Med. 2019;28(4):555–67.
Liao C-H, Wang C-C, Jiang Y-H. Intravesical onabotulinumtoxinA injection for overactive bladder patients with frailty, medical comorbidities or prior lower urinary tract surgery. Toxins (Basel). 2016;8(4):91.
Suskind AM, Kowalik C, Quanstrom K, Boscardin J, Zhao S, Reynolds WS, et al. The impact of frailty on treatment for overactive bladder in older adults. Neurourol Urodyn. 2019;38(7):1915–23.
Jiang Y-H, Liao C-H, Tang D-L, Kuo H-C. Efficacy and safety of intravesical onabotulinumtoxinA injection on elderly patients with chronic central nervous system lesions and overactive bladder. PLoS One. 2014;9(8):e105989.
Tanne JH. FDA adds “black box” warning label to fluoroquinolone antibiotics. BMJ. 2008;337:a816.
Gardella B, Iacobone AD, Porru D, Musacchi V, Dominoni M, Tinelli C, et al. Effect of local estrogen therapy (LET) on urinary and sexual symptoms in premenopausal women with interstitial cystitis/bladder pain syndrome (IC/BPS). Gynecol Endocrinol. 2015;31(10):828–32.
La Rosa VL, Ciebiera M, Lin L-T, Fan S, Butticè S, Sathyapalan T, et al. Treatment of genitourinary syndrome of menopause: the potential effects of intravaginal ultralow-concentration oestriol and intravaginal dehydroepiandrosterone on quality of life and sexual function. Menopause Rev. 2019;18(2):116–22.
Patnaik SS, Laganà AS, Vitale SG, Butticè S, Noventa M, Gizzo S, et al. Etiology, pathophysiology and biomarkers of interstitial cystitis/painful bladder syndrome. Arch Gynecol Obstet. 2017;295(6):1341–59.
Rahn DD, Carberry C, Sanses TV, Mamik MM, Ward RM, Meriwether KV, et al. Vaginal estrogen for genitourinary syndrome of menopause: a systematic review. Obstet Gynecol. 2014;124(6):1147–56.
Peeker R, Enerbäck L, Fall M, Aldenborg F. Recruitment, distribution and phenotypes of mast cells in interstitial cystitis. J Urol. 2000;163(3):1009–15.
Theoharides TC. Hydroxyzine for interstitial cystitis. J Allergy Clin Immunol. 1993;91(2):686–7.
Theoharides TC. Hydroxyzine in the treatment of interstitial cystitis. Urol Clin N Am. 1994;21(1):113–9.
Theoharides TC, Sant GR. Hydroxyzine therapy for interstitial cystitis. Urology. 1997;49(5A Suppl.):108–10.
Northstart RxLLC. Hydroxyzine [package insert]. DailyMed. 2020.http://dailymed.nlm.nih.gov/dailymed/druginfo.cfm?setid=8e5fce17-936e-46ea-a969-518c952c2091. Accessed 24 Sept 2020.
Simons KJ, Watson WTA, Chen XY, Simons FER. Pharmacokinetic and pharmacodynamic studies of the H1-receptor antagonist hydroxyzine in the elderly. Clin Pharmacol Ther. 1989;45(1):9–14.
Meares EM. Interstitial cystitis: 1987. Urology. 1987;29(4 Suppl.):46–8.
Thilagarajah R, Witherow RO, Walker MM. Oral cimetidine gives effective symptom relief in painful bladder disease: a prospective, randomized, double-blind placebo-controlled trial. BJU Int. 2001;87(3):207–12.
Dasgupta P, Sharma SD, Womack C, Blackford HN, Dennis P. Cimetidine in painful bladder syndrome: a histopathological study. BJU Int. 2001;88(3):183–6.
Lewi H. Cimetidine in treatment of interstitial cystitis. Urology. 1995;45(6):1088.
Seshadri P, Emerson L, Morales A. Cimetidine in the treatment of interstitial cystitis. Urology. 1994;44(4):614–6.
Mylan Pharmaceuticals Inc. Cimetidine [package insert]. DailyMed. 2020.https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=06c0a509-026f-44e0-9975-a94a8de51d43. Accessed 13 Oct 2020.
Fall M, Oberpenning F, Peeker R. Treatment of bladder pain syndrome/interstitial cystitis 2008: can we make evidence-based decisions? Eur Urol. 2008;54(1):65–75.
Vij M, Srikrishna S, Cardozo L. Interstitial cystitis: diagnosis and management. Eur J Obstet Gynecol Reprod Biol. 2012;161(1):1–7.
Foster HE, Hanno PM, Nickel JC, Payne CK, Mayer RD, Burks DA, et al. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J Urol. 2010;183(5):1853–8.
van Ophoven A, Pokupic S, Heinecke A, Hertle L. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. J Urol. 2004;172(2):533–6.
van Ophoven A, Hertle L. Long-term results of amitriptyline treatment for interstitial cystitis. J Urol. 2005;174(5):1837–40.
Cutler NR, Narang PK. Implications of dosing tricyclic antidepressants and benzodiazepines in geriatrics. Psychiatr Clin N Am. 1984;7(4):845–61.
Sasaki K, Smith CP, Chuang YC, Lee JY, Kim JC, Chancellor MB. Oral gabapentin (neurontin) treatment of refractory genitourinary tract pain. Tech Urol. 2001;7(1):47–9.
Kwon W-A, Ahn SH, Oh TH, Lee JW, Han DY, Jeong HJ. Effect of low-dose triple therapy using gabapentin, amitriptyline, and a nonsteroidal anti-inflammatory drug for overactive bladder symptoms in patients with bladder pain syndrome. Int Neurourol J. 2013;17(2):78–82.
Chua ME, See MC, Esmeňa EB, Balingit JC, Morales ML. Efficacy and safety of gabapentin in comparison to solifenacin succinate in adult overactive bladder treatment. Low Urin Tract Symptoms. 2018;10(2):135–42.
Moore RA, Wiffen PJ, Derry S, Rice AS. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. In: Moore RA, editor. Cochrane database of systematic reviews. Chichester: Wiley; 2014.
Akiyama Y, Hanno P. Phenotyping of interstitial cystitis/bladder pain syndrome. Int J Urol. 2019;26(S1):17–9.
Crescenze IM, Gupta P, Adams G, Oldendorf A, Stoffel JT, Romo PGB, et al. Advanced management of patients with ulcerative interstitial cystitis/bladder pain syndrome. Urology. 2019;133:78–83.
Cox M, John KJ, Carl KG. Assessment of patient outcomes following submucosal injection of triamcinolone for treatment of Hunner’s ulcer subtype interstitial cystitis. Can J Urol. 2009;16(2):4536–5440.
Forrest JB, Payne CK, Erickson DR. Cyclosporine A for refractory interstitial cystitis/bladder pain syndrome: experience of 3 tertiary centers. J Urol. 2012;188(4):1186–91.
Sairanen J, Tammela TLJ, Leppilahti M, Multanen M, Paananen I, Lehtoranta K, et al. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. J Urol. 2005;174(6):2235–8.
Ehrén I, Hallén Grufman K, Vrba M, Sundelin R, Lafolie P. Nitric oxide as a marker for evaluation of treatment effect of cyclosporine A in patients with bladder pain syndrome/interstitial cystitis type 3C. Scand J Urol. 2013;47(6):503–8.
Forsell T, Ruutu M, Isoniemi H, Ahonen J, Alfthan O. Cyclosporine in severe interstitial cystitis. J Urol. 1996;155(5):1591–3.
Sairanen J, Forsell T, Ruutu M. Long-term outcome of patients with interstitial cystitis treated with low dose cyclosporine A. J Urol. 2004;171(6 Pt 1):2138–41.
Larish AM, Dickson RR, Kudgus RA, McGovern RM, Reid JM, Hooten WM, et al. Vaginal diazepam for nonrelaxing pelvic floor dysfunction: the pharmacokinetic profile. J Sex Med. 2019;16(6):763–6.
Rogalski MJ, Kellogg-Spadt S, Hoffmann AR, Fariello JY, Whitmore KE. Retrospective chart review of vaginal diazepam suppository use in high-tone pelvic floor dysfunction. Int Urogynecol J. 2010;21(7):895–9.
Bartley J, Han E, Gupta P, Gaines N, Killinger KA, Boura JA, et al. Transvaginal trigger point injections improve pain scores in women with pelvic floor hypertonicity and pelvic pain conditions. Female Pelvic Med Reconstr Surg. 2019;25(5):392–6.
Steers WD, Tuttle JB. Mechanisms of disease: the role of nerve growth factor in the pathophysiology of bladder disorders. Nat Clin Pract Urol. 2006;3(2):101–10.
Evans RJ, Moldwin RM, Cossons N, Darekar A, Mills IW, Scholfield D. Proof of concept trial of tanezumab for the treatment of symptoms associated with interstitial cystitis. J Urol. 2011;185(5):1716–21.
Nickel JC, Mills IW, Crook TJ, Jorga A, Smith MD, Atkinson G, et al. Tanezumab reduces pain in women with interstitial cystitis/bladder pain syndrome and patients with nonurological associated somatic syndromes. J Urol. 2016;195(4 Pt 1):942–8.
Author information
Authors and Affiliations
Contributions
Drs Gracely and Cameron both participated in the literature search and in the writing and final review of this manuscript.
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflict of interest
Alyssa Gracely has no conflicts of interest that are directly relevant to the content of this article. Anne P. Cameron is a PI for Medtronic and a speaker for Wellspect.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability and material
Not applicable.
Code availability
Not applicable.
Rights and permissions
About this article
Cite this article
Gracely, A., Cameron, A.P. Managing Interstitial Cystitis/Bladder Pain Syndrome in Older Adults. Drugs Aging 38, 1–16 (2021). https://doi.org/10.1007/s40266-020-00810-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-020-00810-w