Abstract
Background
Temporal changes in the dispensing of glucose-lowering drugs (GLD) and their associated costs among elderly populations is unclear. This information is especially relevant to countries in which medications are partly or fully government subsidized.
Objective
Our objective was to estimate the trends in prevalence, incidence and costs associated with GLD dispensed to older Australians.
Methods
We analysed Pharmaceutical Benefits Scheme data for 76,906 people aged ≥ 65 years dispensed diabetes medications over the period 2013–2016.
Results
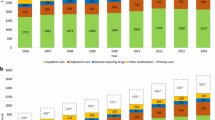
Older males were dispensed more GLD than were older females, with the marginal difference increasing from 3.2% in 2013 (age-sex adjusted incidence rate ratio [aIRR] 1.032; 95% confidence interval [CI] 1.024–1.041; p < 0.001) to 3.9% in 2016 (aIRR 1.039; 95% CI 1.030–1.047; p < 0.001). The number of GLD dispensed per person was consistently lower in those aged ≥ 75 years than in those aged 65–74 years, with the gap widening over the years. More patients were initiated with sodium-glucose cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors over the study period, at the expense of older GLD. The proportion of users and attributed costs associated with the use of metformin, sulfonylureas, α-glucosidase inhibitors and thiazolidinediones decreased over time. The total subsidized costs of GLD is forecast to increase to $A395 million by 2020.
Conclusions
The treatment landscape for diabetes in Australia is undergoing dynamic change. More patients were initiated with the newer but costlier GLD over the study period.

Similar content being viewed by others
References
American Diabetes Association (2018) Economic costs of diabetes in the U.S. in 2017. Diabetes Care 41 (5):917–928.
National Diabetes Services Scheme Older People. 2017. https://www.ndss.com.au/older-people. Accessed 3 Sep 2018.
Cefalu WT, Kaul S, Gerstein HC, Holman RR, Zinman B, Skyler JS, Green JB, Buse JB, Inzucchi SE, Leiter LA, Raz I, Rosenstock J, Riddle MC. Cardiovascular outcomes trials in type 2 diabetes: Where do we go from here? Reflections from a diabetes care editors’ expert forum. Diabetes Care. 2018;41(1):14–31.
Zheng SL, Roddick AJ, Aghar-Jaffar R, Shun-Shin MJ, Francis D, Oliver N, Meeran K. Association between use of sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 agonists, and dipeptidyl peptidase 4 inhibitors with all-cause mortality in patients with type 2 diabetes: a systematic review and meta-analysis. JAMA. 2018;319(15):1580–91.
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Sabatine MS (2018) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet:S0140-6736(0118)32590-X.
Pharmaceutical Benefits Scheme About the PBS. http://www.pbs.gov.au/info/about-the-pbs. Accessed 24 Jan 2020.
Davis WA, Peters KE, Makepeace A, Griffiths S, Bundell C, Grant SFA, Ellard S, Hattersley AT, Paul Chubb SA, Bruce DG, Davis TME. Prevalence of diabetes in Australia: insights from the Fremantle Diabetes Study Phase II. Intern Med J. 2018;48:803–9.
Mellish L, Karanges EA, Litchfield MJ, Schaffer AL, Blanch B, Daniels BJ, Segrave A, Pearson SA. The Australian Pharmaceutical Benefits Scheme data collection: a practical guide for researchers. BMC Res Notes. 2015;8:634.
Ofori-Asenso R, Ilomäki J, Tacey M, Zomer E, Curtis AJ, Bell JS, Zoungas S, Liew D (2018) Patterns of statin use and long-term adherence and persistence among older adults with diabetes. J Diabetes 10(9):699–707. https://doi.org/10.1111/1753-0407.12769(Epub ahead of print).
Pharmaceutical Benefits Scheme https://www.pbs.gov.au/pbs/home. Accessed 15 Aug 2018.
Australian Bureau of Statistics (2017) Diabetes mellitus. http://www.absgovau/ausstats/abs@nsf/Lookup/by%20Subject/4364055002~2014-15~Main%20Features~Diabetes%20mellitus~10005. Accessed 14 Dec 2018.
Chu W-M, Ho H-E, Huang K-H, Tsan Y-T, Liou Y-S, Wang Y-H, Lee M-C, Li Y-C. The prescribing trend of oral antidiabetic agents for type 2 diabetes in Taiwan: an 8-year population-based study. Medicine (Baltimore). 2017;96(43):e8257.
Orlando V, Guerriero F, Putignano D, Monetti VM, Tari DU, Farina G, Illario M, Iaccarino G, Menditto E (2015) Prescription patterns of antidiabetic treatment in the elderly. Results from Southern Italy. Curr Diabetes Rev 12(2):100–106.
Yamamoto-Honda R, Takahashi Y, Mori Y, Yamashita S, Yoshida Y, Kawazu S, Iwamoto Y, Kajio H, Yanai H, Mishima S, Handa N, Shimokawa K, Yoshida A, Watanabe H, Ohe K, Shimbo T, Noda M. Changes in antidiabetic drug prescription and glycemic control trends in elderly patients with type 2 diabetes mellitus from 2005–2013: an analysis of the National Center Diabetes Database (NCDD-03). Intern Med. 2018;57:1229–40.
Acknowledgements
The authors acknowledge the Australian Government Department of Human Services for provision of the data.
Author information
Authors and Affiliations
Contributions
KLC initially conceived the concept of this study. KLC and ROA were responsible for data collection. KLC and FMH performed the statistical analysis. KLC drafted the manuscript. All the authors made substantial contribution to the interpretation of data and revised the manuscript for important intellectual content. KLC and DL are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Conflicts of interest
DL has received research grants and honoraria from AstraZeneca and Boehringer Ingelheim. SZ has previously participated in educational events and advisory boards on behalf of Monash University for AstraZeneca, Merck Sharp & Dohme (Australia), Servier Australia and Novo Nordisk and holds NHMRC Senior Research Fellowships. KLC, FMH, ROA, JI and JSB have no conflicts of interest that are directly relevant to the content of this article.
Ethics statement
This study was approved by the Monash University Human Research Ethics Committee (MUHREC). The Australian Government Department of Human Services also approved the research plan and the final manuscript.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chin, K.L., Hidayat, F.M., Ofori-Asenso, R. et al. Trends in the Dispensing and Costs of Glucose-Lowering Medications Among Older Australians: Findings from National Claims Data. Drugs Aging 37, 393–398 (2020). https://doi.org/10.1007/s40266-020-00759-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-020-00759-w