Abstract
Introduction
Aspirin is widely used to prevent cardiovascular diseases (CVDs). However, the balance of its benefits and risks in the primary prevention of CVDs and cancer is unclear, especially in elderly Asians. The present study aimed to evaluate the efficacy of aspirin in the primary prevention of major adverse cardiac and cerebrovascular events (MACCE), bleeding risk, and cancer in elderly Koreans with cardiovascular (CV) risk factors.
Methods
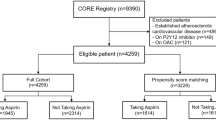
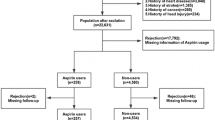
This retrospective cohort study used data from the Korean National Health Insurance Service–Senior cohort database (2002–2015). Patients aged 60–90 years with hypertension, type 2 diabetes mellitus (T2DM), or dyslipidemia were identified. Aspirin users were compared with non-users using propensity score matching at a 1:3 ratio. The primary outcome was MACCE, a composite of CV mortality, myocardial infarction, and ischemic stroke. The secondary outcomes were the components of MACCE, all-cause mortality, angina pectoris, heart failure, the incidence and mortality of cancer, and the risks of hemorrhagic stroke and gastrointestinal bleeding. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using a Cox proportional hazard model.
Results
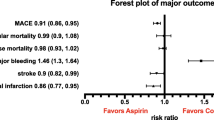
A total of 3366 aspirin users and 10,089 non-users were finally included in the study. During a mean follow-up of 7.8 years, the incidence of MACCE was 15.2% in aspirin users and 22.4% in non-users. The risk of MACCE was significantly lower in aspirin users than in non-users (HR 0.76; 95% CI 0.69–0.85), and this risk was significantly reduced in patients using aspirin over 5 years (HR 0.52; 95% CI 0.46–0.60). Aspirin use was associated with a 21% reduction in the risk of primary cancer (HR 0.79; 95% CI 0.70–0.88) and cancer-related mortality (HR 0.72; 95% CI 0.61–0.84). No significant differences in bleeding risks were observed between the two groups.
Conclusion
Aspirin reduced the risks of MACCE and cancer without increasing the bleeding risk in elderly Koreans with hypertension, T2DM, or dyslipidemia. Moreover, the benefits of the long-term use of aspirin in reducing the risks of MACCE were demonstrated. However, the decision of using aspirin for primary prevention must be carefully made on an individual basis, while estimating the benefit–risk balance of aspirin.


Similar content being viewed by others
References
Statistics Korea. Korean Statistical Information Service. 2018. http://kosis.kr/eng/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ETITLE&parmTabId=M_01_01#SelectStatsBoxDiv. Accessed 04 Jul 2019.
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25.
Rothwell PM, Algra A, Chen Z, Diener HC, Norrving B, Mehta Z. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. The Lancet. 2016;388(10042):365–75.
Trialists’ Collaboration A. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86.
Gorelick PB, Weisman SM. Risk of hemorrhagic stroke with aspirin use: an update. Stroke. 2005;36(8):1801–7.
Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. The Lancet. 2009;373:1849–60.
Mahmoud AN, Gad MM, Elgendy AY, Elgendy IY, Bavry AA. Efficacy and safety of aspirin for primary prevention of cardiovascular events: a meta-analysis and trial sequential analysis of randomized controlled trials. Eur Heart J. 2018;40(7):607–17.
Zheng SL, Roddick AJ. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. JAMA. 2019;321(3):277–87.
Lin MH, Lee CH, Lin C, Zou YF, Lu CH, Hsieh CH, et al. Low-dose aspirin for the primary prevention of cardiovascular disease in diabetic individuals: a meta-analysis of randomized control trials and trial sequential analysis. J Clin Med. 2019;8(5):609.
Algra AM, Rothwell PM. Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol. 2012;13(5):518–27.
Rothwell PM, Price JF, Fowkes FGR, Zanchetti A, Roncaglioni MC, Tognoni G, et al. Short-term effects of daily aspirin on cancer incidence, mortality, and non-vascular death: analysis of the time course of risks and benefits in 51 randomised controlled trials. The Lancet. 2012;379(9826):1602–12.
Chubak J, Whitlock EP, Williams SB, Kamineni A, Burda BU, Buist DS, et al. Aspirin for the prevention of cancer incidence and mortality: systematic evidence reviews for the US Preventive Services Task Force. Ann Intern Med. 2016;164(12):814–25.
McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519–28.
Bibbins-Domingo K, Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: US Preventive Services Task Force recommendation statement. A Intern Med. 2016;164(12):836–45.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81.
Arnett DK, Blumenthal RS, Albert MA, Michos ED, Buroker AB, Miedema MD, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol. 2019;140:e596–646.
Stuntz M, Bernstein B. Recent trends in the prevalence of low-dose aspirin use for primary and secondary prevention of cardiovascular disease in the United States, 2012–2015. Prev Med Rep. 2017;5:183–6.
Ikeda Y, Shimada K, Teramoto T, Uchiyama S, Yamazaki T, Oikawa S, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA. 2014;312(23):2510–20.
Sugawara M, Goto Y, Yamazaki T, Teramoto T, Oikawa S, Shimada K, et al. Low-dose aspirin for primary prevention of cardiovascular events in elderly Japanese patients with atherosclerotic risk factors: subanalysis of a randomized clinical trial (JPPP-70). Am J Cardiovasc Drugs. 2019;19(3):299–311.
Seong SC, Kim Y-Y, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7(9):e016640.
Lee J, Lee JS, Park S-H, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2016;46(2):e15.
Tang KL, Quan H, Rabi DM. Measuring medication adherence in patients with incident hypertension: a retrospective cohort study. BMC Health Serv Res. 2017;17(1):135.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson Comorbidity Index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–94.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285–350.
Linden A, Samuels SJ. Using balance statistics to determine the optimal number of controls in matching studies. J Eval in ClinPract. 2013;19:968–75.
Teramoto T, Shimada K, Uchiyama S, Sugawara M, Goto Y, Yamada N, et al. Rationale, design, and baseline data of the Japanese Primary Prevention Project (JPPP)—a randomized, open-label, controlled trial of aspirin versus no aspirin in patients with multiple risk factors for vascular events. Am Heart J. 2010;159(3):361–369.e4.
Ando K, Shimada K, Yamazaki T, Uchiyama S, Uemura Y, Ishizuka N, et al. Influence of blood pressure on the effects of low-dose asprin in elderly patients with multiple atherosclerotic risks. J Hypertens. 2019;37(6):1301–7.
Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293–304.
Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295(3):306–13.
Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. The Lancet. 1998;351(9118):1755–62.
Ogawa H, Nakayama M, Morimoto T, Uemura S, Kanauchi M, Doi N, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134–41.
Group* SCotPHSR. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989;321(3):129–35.
Group ASC. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529–39.
Gaziano JM, Brotons C, Coppolecchia R, Cricelli C, Darius H, Gorelick PB, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. The Lancet. 2018;392(10152):1036–46.
McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509–18.
American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S103–23.
Upadhaya S, Madala S, Baniya R, Saginala K, Khan J. Impact of acetylsalicylic acid on primary prevention of cardiovascular diseases: a meta-analysis of randomized trials. Eur J Prev Cardiol. 2019;26(7):746–9.
Tsoi KK, Ho JM, Chan FC, Sung JJ. Long-term use of low-dose aspirin for cancer prevention: a 10-year population cohort study in Hong Kong. Int J Cancer. 2019;145(1):267–73.
Kim YI, Kim SY, Kim JH, Lee JH, Kim YW, Ryu KW, et al. Long-term low-dose aspirin use reduces gastric cancer incidence: a nationwide cohort study. Cancer Res Treat. 2016;48(2):798.
Elwood PC, Pickering JE, Morgan G, Galante J, Weightman AL, Morris D, et al. Systematic review update of observational studies further supports aspirin role in cancer treatment: time to share evidence and decision-making with patients? PLoS One. 2018;13(9):e0203957.
Landolfi R, Marchioli R, Kutti J, Gisslinger H, Tognoni G, Patrono C, et al. Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med. 2004;350(2):114–24.
Belch J, MacCuish A, Campbell I, Cobbe S, Taylor R, Prescott R, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840.
Framework MRCsGPR. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. The Lancet. 1998;351(9098):233–41.
Elwood PC, Morgan G, Galante J, Chia JW, Dolwani S, Graziano JM, et al. Systematic review and meta-analysis of randomised trials to ascertain fatal gastrointestinal bleeding events attributable to preventive low-dose aspirin: no evidence of increased risk. PLoS One. 2016;11(11):e0166166.
Huang WY, Saver JL, Wu YL, Lin CJ, Lee M, Ovbiagele B. Frequency of intracranial hemorrhage with low-dose aspirin in individuals without symptomatic cardiovascular disease: a systematic review and meta-analysis. JAMA Neurol. 2019. https://doi.org/10.1001/jamaneurol.2019.1120.
Klatsky AL, Friedman GD, Sidney S, Kipp H, Kubo A, Armstrong MA. Risk of hemorrhagic stroke in Asian American ethnic groups. Neuroepidemiology. 2005;25(1):26–31.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. The Lancet Neurol. 2010;9(2):167–76.
An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. Journal of Stroke. 2017;19(1):3.
Soriano LC, Lanas A, Soriano-Gabarró M, Rodríguez LAG. Incidence of upper and lower gastrointestinal bleeding in new users of low-dose aspirin. Clin Gastroenterol Hepatol. 2019;17(5):887–889.e6.
Pignone M, DeWalt DA. More evidence to help guide decision making about aspirin for primary prevention. Ann Intern Med. 2018;169(11):804–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the conduct of this study.
Conflict of interest
Jung and Lee declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Jung, M., Lee, S. Efficacy of Aspirin in the Primary Prevention of Cardiovascular Diseases and Cancer in the Elderly: A Population-Based Cohort Study in Korea. Drugs Aging 37, 43–55 (2020). https://doi.org/10.1007/s40266-019-00723-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00723-3