Abstract
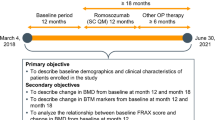
Rheumatoid arthritis (RA) is a chronic disabling disease that is associated with increased localized and generalized osteoporosis (OP). Previous studies estimated that approximately one-third of the RA population experience bone loss. Moreover, RA patients suffer from a doubled fracture incidence depending on several clinical factors, such as disease severity, age, glucocorticoid (GC) use, and immobility. As OP fractures are related to impaired quality of life and increased mortality rates, OP has an enormous impact on global health status. Therefore, there is an urgent need for a holistic approach in daily clinical practice. In other words, both OP- and RA-related factors should be taken into account in treatment guidelines for OP in RA. First, to determine the actual fracture risk, dual-energy X-ray absorptiometry (DXA), including vertebral fracture assessment (VFA) and calculation of the 10-year fracture risk with FRAX®, should be performed. In case of high fracture risk, calcium and vitamin D should be supplemented alongside anti-osteoporotic treatment. Importantly, RA treatment should be optimal, aiming at low disease activity or remission. Moreover, GC treatment should be at the lowest possible dose. In this way, good fracture risk management will lead to fracture risk reduction in RA patients. This review provides a practical guide for clinicians regarding pharmacological treatment options in RA patients with OP, taking into account both osteoporotic-related factors and factors related to RA.
Similar content being viewed by others
Osteoporosis (OP) is a common comorbidity in rheumatoid arthritis (RA) and should be considered an extra-articular manifestation. |
Treatment of OP in RA needs a holistic approach, taking into account both osteoporotic-related risk factors and rheumatoid-related factors. |
1 Introduction
Rheumatoid arthritis (RA) is a chronic systemic autoimmune disease characterized by symmetrical inflammation of the synovium, particularly in the smaller parts of the hands and feet. The prevalence of RA has been estimated to be approximately 1.0% in the general population and affects women more often than men. Due to the inflammatory burden of the disease, RA patients experience tenderness and articular damage of various joints, leading to functional disability, reduced quality of life, and reduced life expectancy [1,2,3,4]. The manifestations of RA are not limited to joint inflammation, as extra-articular manifestations (EAM) such as, for example, rheumatoid nodules, vasculitis, (epi)scleritis, pulmonary fibrosis, pericarditis, or Felty syndrome, are present in approximately 40% of RA patients [5].
A characteristic feature of (preclinical) RA is local bone loss, also called periarticular osteopenia, due to a decrease in bone trabeculae and the presence of bone marrow edema [6,7,8]. Periarticular bone loss is a consequence of the ongoing impact of inflammatory cytokines such as interleukin (IL)-6 or tumor necrosis factor (TNF) on the (peri)articular sites, and is more frequently present in RA patients with autoantibodies against citrullinated proteins (ACPAs) [7, 9, 10]. It has been demonstrated that ACPAs are already present years before the clinical onset of RA, therefore it is not surprising that, in some patients, local bone loss is already present in the preclinical phase of RA [11, 12]. Interestingly, recent studies suggest a direct association between low bone mass (i.e. bone mineral density [BMD]) and bone morphometric parameters (i.e. bone quality) and anti-CCP antibody (ACPA) titers in RA patients [13, 14]. Local bone loss at periarticular sites is a result of cortical bone thinning at the insertion sites of the inflamed synovium, which is the predominant localization of bone erosion development [8, 15]. Next to localized bone loss, generalized osteoporosis (OP) is a common EAM, especially in patients with longstanding and uncontrolled RA [16,17,18]. Since these patients have a higher risk for fragility fractures (i.e. hip and vertebral fractures) [19, 20], and these fragility fractures are related to a higher disease burden, impaired quality of life, increased health care costs, and an augmented mortality rate [21], more awareness for OP and the treatment of this comorbid condition in RA patients is needed. Therefore, this review aims to provide a practical guide for clinicians for pharmacological treatment options in RA patients suffering from OP.
2 Epidemiology
In RA patients, decreased mean BMD values of the spine and hips, compared with healthy individuals, has been known to be a very common EAM of RA for several years. In earlier studies, before the introduction of biologics, the prevalence of loss of BMD has been estimated to be doubled in both male and female RA patients compared with healthy controls at both the lumbar spine and the hip [16, 17]. In these studies, up to 32% of subjects experience loss of BMD, compared with only 16% in the ‘healthy’ reference group. Moreover, it was observed that RA patients have double the risk of both hip fractures and vertebral fractures, with prevalence estimates ranging from 13 to 36% depending on clinical parameters such as disease burden and duration, concomitant medication, history of (non)vertebral fractures, and age [19, 22,23,24].
In the Oslo RA register, postmenopausal female RA and non-RA patients were included, with a mean age of ≥ 63 years in both groups. In this study, substantially more vertebral deformities were observed in RA patients compared with non-RA patients, i.e. 147 and 51 vertebral deformities, respectively. Fifty-five (22.1%) patients with RA, compared with 38 (15.3%) controls, had at least one vertebral deformity measured morphometrically [odds ratio (OR) 1.74, 95% confidence interval (CI) 1.02–3.04], and 28 (11.2%) versus 12 (4.8%) had two or more deformities (OR 2.60, 95% CI 1.21–6.04) [22].
In the British General Practice Research Database (BGPRD), fracture rates were compared between RA and non-RA patients in different age groups. This registry observed that RA patients had comparable increases in fracture risk, with an adjusted relative risk (RR) for clinical osteoporotic fracture of 1.4 (95% CI 1.2–1.7) in male RA patients and 1.5 (95% CI 1.4–1.6) in female RA patients, in all age groups, when compared with non-RA patients. Interestingly, it was shown that there were an increasing number of fracture rates in patients of higher age groups, especially in patients aged 70 years and older [19].
The burden of OP (i.e. OP-related fractures) in RA patients can be explained by several reasons (Fig. 1). First, RA is a chronic disabling inflammatory disease that is associated with decreased mobility and physical activity, as well as lower muscle mass and sarcopenia, all factors known to have detrimental effects on bone mass [25,26,27,28]. Second, for several years now, the direct effects of inflammation on bone density have been known, especially in newly diagnosed RA patients [29]. Moreover, it has been observed that inflammation and bone loss share common pathways in pathogenesis [30,31,32].
Intriguingly, van Staa et al. observed that RA patients without prior GC use had an increased risk for both vertebral fractures (RR 1.5, 95% CI 1.2–1.9) and hip fractures (RR 1.7, 95% CI 1.5–2.0) compared with controls without a history of RA, at any time during follow-up. In addition, increased risk was also seen in early glucocorticoid (GC) users, not just in chronic users, suggesting that the underlying active disease with ongoing inflammation and muscle weakness should be considered a relevant risk factor for increased prevalence of OP and the incidence of fractures [19]. Third, it is known that GCs have direct and indirect negative effects on bone density [33, 34]. Indeed, previous studies have estimated that 30% of all patients treated with GCs for at least 6 months will develop OP [35]. Therefore, RA patients with (long-term) GC exposure have an accelerated risk for glucocorticoid-induced OP (GIOP) during their lifetime. For the abovementioned reasons, in relation to RA and the presence of classical risk factors for OP (e.g. familial OP or hip fracture and postmenopausal age), many RA patients suffer from both OP and an augmented fracture rate.
3 Fracture Risk Assessment
OP is defined as a musculoskeletal disorder characterized by compromised bone strength, predisposing individuals to an increased fracture risk [36]. Individuals can be divided into three groups according to the WHO criteria, dependent on the BMD value: T score ≧ − 1 = normal BMD; − 2.5 < T score < − 1 = osteopenia and T score ≦ − 2.5 = OP. However, most fractures occur paradoxically in patients not suffering from OP but suffering from osteopenia, and this can be partly explained by the fact that these patients also have impaired quality of bone, which is not measured with DXA [37, 38]. Moreover, in all patients, vertebral fracture assessment (VFA) is recommended. The gold standard for detecting vertebral fractures is a conventional radiograph of the thoracolumbar spine. In clinical practice, the Genant score is used, in which the degree of height loss is assessed and can be graded as mild (grade 1, 20–25% height loss), moderate (grade 2, 25–40% height loss), or severe (grade 3, > 40% height loss) [39]. However, VFA is an elegant alternative because this technique has been proven to be safe, with less radiation exposure, is less time-consuming, and has lower costs than conventional radiographs with comparable accuracy in detecting moderate-to-severe vertebral fractures [40]. Another way to assess fracture risk is to calculate the 10-year probability for a major fracture (i.e. vertebral, hip, humerus, or wrist fracture) using the computer-based algorithm FRAX® [41]. This algorithm includes several clinical risk factors, including, among others, previous fractures, parental history of hip fracture, age, smoking, GC use, and secondary causes for OP, including RA. Although FRAX® is very useful in daily clinical practice, this calculation tool has some disadvantages for RA patients as it does not take into account the cumulative disease burden and disease activity, which are notorious independent risk factors for bone loss in RA. Therefore, it has been suggested that FRAX® might underestimate the fracture risk in these patients [42, 43]. Other limitations of this fracture risk calculation tool include the fact that it does not take into account fall risk, vertebral fractures, and the dose of GC in the FRAX algorithm. Moreover, it was observed that the risk of a subsequent fracture after an initial fracture, is strongly upregulated in the first 2 years [44]. Although the FRAX® has some limitations, in daily clinical practice FRAX® is an adequate algorithm to identify high-risk RA patients and to determine which RA patients should be treated according to (inter)national guidelines [45].
4 Nonpharmacological Interventions
Although no randomized controlled studies have been performed on nonpharmacological interventions and fracture reduction, some general measures have been advocated in OP patients. First, a healthy lifestyle, including nonsmoking, little to no alcohol intake, and a nonsedentary and active lifestyle with exercises, should be advised in all patients in order to reduce bone loss [46,47,48]. Moreover, adequate calcium intake up to a daily dose of 1000–1200 mg is necessary; if daily intake is below this threshold, calcium supplementation is needed. Although calcium supplementation is needed in patients with a low calcium intake, high dietary calcium intake has been debated as supplementation has been associated with an elevated risk of cardiovascular disease (CVD) [49]. This is a concern, particularly in RA patients, as RA has been associated with an increased risk of CVD that equals the CVD risk of diabetes mellitus [50]. Moreover, a recent study showed an increased risk of CVD in RA patients with fragility fractures [51]. Another nonpharmacological modifiable factor is vitamin D deficiency, as a large meta-analysis has shown that vitamin D supplementation (800 IU/day) in patients who also received calcium supplementation is associated with a 20% reduction in falls and nonvertebral fractures [52, 53]. Therefore, supplementation of calcium and vitamin D is needed, along with general advice regarding low alcohol intake, cessation of smoking, and performing exercises to reduce fracture risk in RA patients.
5 Anti-osteoporotic Drugs in Rheumatoid Arthritis
5.1 Bisphosphonates
To date, no randomized controlled trials with bisphosphonates (BPs) have been conducted in osteoporotic RA patients with fractures as the primary outcome measure. Nevertheless, osteoporotic RA patients have been included in GIOP trials; therefore, from these RCTs, sparse data and indirect evidence on fracture reduction in osteoporotic RA patients treated with BPs are available [54]. Looking into these GIOP studies in more detail, a strong reduction in vertebral fractures was shown in BP-treated GIOP patients (RR 0.57, 95% CI 0.35–0.91) and a nonsignificant reduction in non-vertebral fractures has been observed (RR 0.79, 95% CI 0.47–1.33); however, most of the randomized controlled trials did not specify whether these were RA patients. Moreover, due to limited number of RA patients or the limited number of incident fractures due to the short follow-up duration, outcome data on fractures could not be specified.
The study performed by Lems et al. focused specifically on the effects of BPs in RA patients treated with low-dose prednisolone [55]. In that double-blind, placebo-controlled RCT, 163 RA patients who were treated with low-dose prednisone (≤ 10 mg/day) for at least 3 months were enrolled. Patients were randomized to receive daily doses of alendronate or placebo. Compared with placebo, a significant increase in BMD as the primary outcome at both the lumbar spine and the hip was shown after 1 year in the BP-treated group. As a secondary outcome, the fracture incidence was evaluated in both the BP- and placebo-treated groups. Overall, no significant differences were observed between fractures. Remarkably, there was a trend towards a higher incidence of vertebral deformities in the alendronate-treated patients, which seems to be in conflict with the favorable effects of alendronate on both BMD and markers of bone turnover. However, a probable explanation is that the alendronate-treated patients had more severe OP, as these patients had more prevalent vertebral fractures at baseline compared with patients in the placebo group.
Hence, to summarize the evidence of fracture risk reduction of BPs in RA patients, in general, BPs have been shown to reduce the risk of vertebral fractures in GIOP patients (including RA patients), but only one study focused on BPs and fracture risk in RA patients, showing significant BMD improvement, but no difference in fracture risk reduction compared with placebo, possibly due to the short follow-up duration.
5.2 Modern Treatment Options in Osteoporosis (OP): Teriparatide and Denosumab
5.2.1 Teriparatide
Teriparatide is a parathyroid hormone analog that is administered subcutaneously daily. It acts as an anabolic drug by increasing bone formation by decreasing osteoblast and osteocyte apoptosis and stimulating osteoblasts. Several studies showed fracture risk reduction in (postmenopausal) women and men [56].
In GIOP patients, including patients with rheumatic disorders such as RA, a landmark study showed that teriparatide, compared with the active comparator and antiresorptive drug alendronate, resulted in not only significantly more increases in BMD levels but also in significant vertebral fracture reduction, which was confirmed in the extension study and in daily clinical practice [57,58,59]. The efficacy of teriparatide has been studied in osteoporotic RA patients (n = 70) compared with postmenopausal osteoporotic patients without RA (n = 62) [60]. Interestingly, this study observed greater responses to teriparatide on bone formation markers bone alkaline phosphatase and P1NP at 1 month of treatment, and on femoral neck BMD after 18 months of treatment (4.7 vs. 0.7%, p = 0.038), but not on the lumbar spine and BMD levels in RA patients compared with osteoporotic patients. However, no differences in fracture rate could be detected in this small case-control study.
Another nonrandomized observational study by the same research group assessed the effects on BMD outcome after either continuing BP, switching from a BP to teriparatide, or switching from BP to denosumab in a group of 194 RA patients with, on average, over 3 years of BP use [61]. During the 18-month follow-up period, the group continuing BPs experienced an 8.8% incident fracture, compared with only 4.1% and 2.5% in denosumab-treated and teriparatide-treated patients, respectively.
In a recently published study by Langdahl et al., an integrated analysis of four prospective observational studies including approximately 8900 patients, and with approximately 900 RA patients included, found RA to be an important risk factor for fractures [62]. In that study, it was observed that RA patients treated with teriparatide showed significant reductions in vertebral and nonvertebral fractures. Therefore, it can be concluded that teriparatide is a pivotal bone formation drug that showed fracture reduction not only in OP patients but also in RA patients. Abaloparatide and romosozumab are new anabolic agents that have been approved in US for postmenopausal women, but not (yet) in Europe. Both abaloparatide and romosozumab have not been tested in GC users.
5.2.2 Denosumab
Denosumab is a fully human monoclonal antibody to an activator of osteoclastic differentiation and proliferation, soluble RANK-L. RANK-L is upregulated in postmenopausal women and in patients in an inflammatory state, such as RA [63, 64]. In postmenopausal women, denosumab has shown strong bone protective properties, as reported in the FREEDOM phase III trial. An RR reduction of vertebral, nonvertebral, and hip fractures compared with placebo was found in 68%, 20%, and 40% of patients, respectively [65]. In RA patients, there are some data on denosumab and OP.
Recently, it was found that compared with risedronate, denosumab had superior effects on spine and hip BMD after 1 year, which continued after 2 years in patients with GIOP [66, 67]. In this large, randomized controlled trial in more than 700 patients, approximately 40% of patients had RA. Despite the superior effects on BMD, no differences were observed in vertebral, hip, and nonvertebral fractures. At first sight, this could be disappointing, but the study was smaller (295 denosumab-treated patients vs. 295 alendronate-treated patients), the observation time was shorter (1 vs. 3 years), and denosumab was tested against placebo in the phase III FREEDOM study, and also against the active comparator risedronate in the GIOP study.
In a phase II, randomized controlled trial in 350 RA patients taking methotrexate, denosumab every 6, 3, or 2 months, or placebo, was added to methotrexate treatment to study the effects of denosumab on radiographic progression in RA patients. Not surprisingly, BMD significantly increased at both lumbar spine and total hip level in the denosumab groups compared with placebo at 6 and 12 months [68]. Intriguingly, this study also showed that denosumab significantly inhibits radiographic progression at the joints, as the modified Sharp erosion score showed less increase in the denosumab-treated groups compared with the placebo groups (0.27, 0.14, and 0.09 for denosumab every 6, 3, or 2 months, respectively, versus 0.99 in the placebo group), while no difference was found in joint space narrowing. Moreover, a higher percentage of RA patients taking methotrexate had no deterioration in disease progression in the modified Sharp erosion score in the denosumab group (78.8, 80.5, and 83.5 in the denosumab groups, versus 62.5% in the placebo group). In the recently published DESIRABLE study, which included 650 RA patients taking conventional disease-modifying antirheumatic drugs (cDMARDs), these observations were replicated in a well-conducted, randomized, placebo-controlled trial, as this study clearly showed that compared with placebo, denosumab significantly inhibited the progression of joint destruction and increased lumbar spine BMD in patients receiving concomitant csDMARD treatment [69]. However, no changes in the disease activity of RA were observed in the denosumab-treated groups compared with the placebo group, indicating that denosumab acts directly on the bone metabolism and has no clinically relevant effects on cartilage and the immune system. Importantly, no differences in adverse events were observed between the denosumab-treated groups and placebo, which is in line with previous observations in RA patients that denosumab use, compared with non-denosumab use, was not associated with an elevated infection risk, even in patients with concomitant biological DMARD (bDMARD) use [67]. Moreover, it was observed that concomitant denosumab use with bDMARDs had a protective effect on bone erosion development compared with RA patients treated with bDMARDs only [70, 71]. These studies emphasize the disease-modifying role of denosumab in RA patients in reducing radiologic joint damage progression, which was previously stated in the 2017 systematic review by Boleto and colleagues [72].
In another study, it was shown that the combination of calcium and vitamin D supplementation with denosumab enhances BMD more than denosumab monotherapy in RA patients with OP. However, no fractures were observed in both denosumab groups, suggesting a bone protective role in denosumab-treated RA patients [73]. This is in line with the observed fracture risk reduction when patients switched from BPs to a bone protective agent with another mode of action, such as denosumab (4.1% vs. 8.8%) [61]. Therefore, it can be concluded that denosumab significantly increases BMD levels and seems to decrease fracture risk in RA patients, especially when denosumab is combined with calcium D supplementation. Moreover, bone erosion development seems to be arrested in denosumab-treated RA patients, with concomitant methotrexate or bDMARD use.
6 Disease-Modifying Antirheumatic Drugs (DMARDs)
6.1 Conventional DMARDs
Methotrexate and other cDMARDs, such as leflunomide, hydroxychloroquine, and sulfasalazine, are standard drugs in the RA treatment arsenal of rheumatologists. These drugs reduce the disease activity in RA, which may slow down joint damage progression. Since BMD loss in RA is related to disease activity, the use of DMARDs may improve BMD levels. Previously, it was shown that RA patients in clinical remission more often have gain in bone density, while patients with persisting disease activity have rarely any gain in bone density [74]. However, only little evidence is available on cDMARDs and OP and fracture risk in RA.
Looking at the link between the anchor drug for RA, methotrexate, and OP, only a few studies exist. In an observational study of approximately 100 RA patients, no deterioration in BMD was observed in the methotrexate-treated patients (n = 68) compared with the patients treated with other cDMARDs [75]. However, the combination of corticosteroids and methotrexate showed larger decreases in BMD compared with corticosteroids in patients not treated with methotrexate. Other studies on BMD levels and methotrexate in RA patients have been performed, but in these studies no impairment of BMD in approximately 450 methotrexate-treated RA patients compared with other DMARD treatment was observed [76,77,78,79,80]. Surprisingly, some negative effects have been postulated for the anchor drug methotrexate, as methotrexate might jeopardize bone density by direct negative effects on the osteoblast activity [81]. This can potentially lead to spontaneous stress fractures, a condition that has been called ‘methotrexate osteopathy’. Methotrexate osteopathy has been predominately described in patients with hematologic conditions, with much higher doses used than in rheumatology conditions such as RA [82].
Data on the relation between cDMARDs, other than methotrexate, and BMD levels, OP, and fracture risk are scarce. To the best of our knowledge, only one study has been conducted on other cDMARDs and BMD levels. In that study, 153 RA patients with newly diagnosed OP were followed for 1 year, and BMD levels were assessed in these patients [83]. The study showed that the only cDMARD (including methotrexate, sulfasalazine, leflunomide and hydroxychloroquine) associated with BMD improvement at the lumbar spine in multivariate analysis was leflunomide. However, these results should be interpreted with caution as the study was not a randomized, placebo-controlled trial. Therefore, in general, no impairment in BMD has been observed for cDMARDs, although the most critical conclusion is that the data are based on a limited number of patients with a variety of disease activities and other confounders.
6.2 Biological and Targeted Synthetic DMARDs
6.2.1 Tumor Necrosis Factor Inhibitors
Tumor necrosis factor (TNF) inhibitors were the first biologics used in RA treatment, and are pivotal agents in the inhibition of inflammation. Inflammatory cytokines such as TNF induce osteoclast maturation and suppress osteoblast activation by the Dickkopf-1 and disturb bone homeostasis in this manner [84, 85]. Therefore, anti-TNF treatment may improve bone homeostasis in RA patients. Indeed, several studies showed positive effects on bone density and bone turnover in RA patients. Vis et al. were one of the first to report the beneficial effects on bone metabolism in RA patients treated with infliximab [86]. Most studies on the effects of TNF blocking and bone loss have been performed with infliximab in RA. These studies observed preservation or improvement of BMD at the lumbar spine and hip, as well as a decrease in bone resorption markers [e.g. Carboxy terminal crosslinked telopeptides (CTX)] and an increase in bone formation markers (e.g. P1NP) [87]. Similar effects on BMD have been described for other TNF inhibitors such as etanercept and adalimumab [88, 89]. Although favorable effects on BMD levels have been reported, some degree of caution is needed as most of these studies have a short follow-up period and the favorable effects on BMD in relatively small studies are not accompanied by data on fracture risk. Only a few studies investigated whether TNF-blocking agents decrease the fracture incidence rate in RA patients. In a large, population-based study in more than 16,000 RA patients, fracture risk incidence was compared between three different treatment modalities, i.e. RA patients treated with TNF inhibitors, RA patients treated with the cDMARD methotrexate, and RA patients treated with cDMARDs other than MTX [90]. Remarkably, this study observed no differences in the non-vertebral fracture risk incidence rates. The results might be explained by confounding by indication, since anti-TNF is probably prescribed in the most severe RA patients. As a consequence, an increased fracture risk should be expected. The fact that no increased fracture risk was found could be seen as a favorable result.
In another cohort study with approximately 22,000 RA patients treated with TNF inhibitors, no increased incidence fracture rates were observed [91]. However, looking carefully at the data, patients treated with anti-TNF had more EAMs and used more corticosteroids, suggesting that RA patients treated with TNF inhibitors suffered a more severe disease, with more risk factors for osteoporotic fractures. Finally, the North American CORRONA registry with approximately 8500 female RA patients, observed a reduced risk for incident fractures in the anti-TNF group compared with the methotrexate-only group [92]. This is in line with the recent longitudinal prospective observational FORWARD study, a national databank for rheumatic diseases in the US, which observed lower incidence rates for vertebral fractures in RA patients treated with TNF inhibitors [93]. These studies suggest an osteoprotective role for anti-TNF in RA patients.
6.2.2 Other Biological and Targeted Synthetic DMARDs
Data on bDMARDS (such as abatacept, rituximab, tocilizumab, and sarilimumab) and targeted synthetic (ts)DMARDs in relation to BMD and fracture rate in RA are scarce. Treatment with IL-6 inhibition (i.e. sarilumab and tocilizumab) showed some evidence for osteoprotective effects. In tocilizumab-treated RA patients, Garnero et al. described a decline in bone resorption markers, Carboxy terminal crosslinked telopeptides of type I collagen (CTX-1), and increases in the bone formation markers osteocalcin (OC) and N-terminal propeptide of type I collagen (PINP) [94]. This is in line with the observations made in the MOBILITY trial in sarilumab-treated RA patients. In that study, an improvement in both bone formation and bone resorption markers was shown [95]. More recently a nationwide study in Israel showed stabilization of BMD levels in RA patients during tocilizumab treatment [96]. Interestingly, these observations were replicated in a study performed in Taiwan, where Chen et al. showed both improvement of bone turnover markers and BMD at femoral neck and lumbar spine (the latter was not significant) in ACPA-positive RA patients [97].
Another retrospective observational Japanese study observed larger improvements at hip BMD in RA patients treated with both denosumab and tocilizumab, compared with treatment of RA patients with denosumab and another bDMARD during 18 months of follow-up [71].
Together, these data at least suggest positive effects of IL-6 inhibition on bone metabolism. For the B lymphocyte-depleting therapy rituximab, data in RA patients is even more limited.
This monoclonal antibody targeting CD20-positive B cells has shown some decline in bone resorption markers during rituximab therapy in RA patients [98, 99]. More recently, some exciting data have been reported that rituximab may improve BMD, but these results are preliminary due to the low number of patients and the short duration of follow-up in these rituximab-treated RA patients; therefore, the (long-term) effects of B lymphocyte depletion on OP and fractures remains to be established [100,101,102].
Abatacept is a soluble fusion protein (CTLA4) that blocks CD28 to bind to antigen-presenting cells (APC) with CD80/CD86 on its surface; however, due to this co-stimulation blockade, T lymphocytes are not activated. For several years, abatacept has been known as a good bDMARD in moderate to severe RA. Co-stimulation blockade has been found to have some inhibiting effects on osteoclastogenesis, and, hypothetically, may have some osteoprotective effects [103, 104]. In a prospective, nonrandomized cohort study of 165 RA patients, the effects of abatacept (n = 50) on BMD were compared with other biologics (n = 115) [105]. This study showed a incline in the femoral neck BMD in the group of RA patients treated with abatacept, confirming the hypothesized inhibiting effects on osteoclasts.
The most modern and very promising antirheumatic drugs include the JAK inhibitors. Despite no studies having been published on BMD and JAK inhibition, baricitinib has been shown to suppress osteoclast development by inhibiting expression of RANKL on osteoblasts in vitro, while tofacitinib preserved cortical trabecular hardness in rats [106, 107]. The coming era will reveal whether these drugs will serve as potent osteoprotective agents.
7 Treatment of OP in RA: A Practical Guide
Despite the effective treatment options available nowadays compared with 2–3 decades ago, RA patients still suffer from an increased risk for fractures [108]. One of the most threatening reasons for the high incidence of fractures, next to aging, and the low adherence of osteoporotic drugs, is the ongoing use of corticosteroids, resulting in GIOP. Although the observation that GC use in early and active RA may not diminish BMD levels [109], ongoing GC use, even at low doses, is associated with an elevated fracture risk [110].
To prevent new fractures in RA patients, the following steps may help to identify high-risk OP patients, and may serve as a practical guide for OP treatment in RA.
In our opinion, three measures should be taken into account in the management of OP, as summarized in Table 1: general measures, RA disease-related factors, and OP-related factors.
First, some general lifestyle advice should be given; a normal body mass index (BMI), smoking cessation, and avoiding excessive alcohol intake should be advocated. Moreover, a non-sedentary and active lifestyle should be advised in all patients in order to reduce bone loss. For this reason, every RA patient should be encouraged to perform physical activities, along with daily, weight-bearing exercises if possible.
Second, some RA-related factors should be taken into account. Most important is to aim at remission or the lowest disease activity as possible, as ongoing inflammation jeopardizes bone quality and should be considered a relevant risk factor for osteoporotic-related fractures [19]. Although no superiority for a specific treatment regimen has been demonstrated, some (indirect) evidence exists that bDMARDs may be more pivotal for preventing bone loss when looking carefully at fracture data of cDMARDs compared with bDMARDs. The question remains whether this is only explained by the fact that bDMARDs are excellent and better immunosuppressives in reducing inflammation. Unfortunately, bDMARDs are less often prescribed in the elderly; this is critical since the elderly, in particular, are at high fracture risk. Next, in order to aim at the lowest possible disease activity, efforts should be made to prescribe GCs at the lowest possible dose. Again, GCs are often used in the elderly, which may have devastating effects. If possible, doses higher than 7.5 mg should be avoided and prednisolone sparing-agents (e.g. cDMARDs, bDMARDs, or tsDMARDs) should be added if long-term treatment for higher doses is expected. Moreover, GCs should preferably only be used as an induction therapy and for a short period of time when possible.
Third, it is important to manage all OP-related factors. All RA patients with known OP, VF, or RA who are treated with prednisolone for more than 3 months at doses higher than 7.5 mg every day (or GC equivalent), should be treated with anti-osteoporotic medication, along with calcium and vitamin D supplementation. In daily clinical practice, fracture risk should be ascertained using DXA. Along with DXA performance, VFA is recommended in all postmenopausal and male patients aged 50 years and over or RA patients aged 40 years and over who are treated with prednisolone 5 mg (or a GC equivalent) every day for more than 3 months. In case of a VF or T score ≤ − 2.5, anti-osteoporotic medication, along with calcium and vitamin D supplementation, should be initiated.
As mentioned above, ongoing inflammation in RA patients due to disease activity threatens bone quality and accelerates bone loss. For this reason, it can be advocated that certain RA patients with high disease burden should be treated with osteoporotic medication to decrease fracture risk. Therefore, in (certain) RA patients, lower treatment thresholds (e.g. a T score < − 2.0) can be recommended to decide whether RA patients should be treated with osteoporotic medication [111]. Another validated tool to assess (future) fracture risk in RA patients is the FRAX® calculation tool, which should be recommended in all RA patients with a T score > − 2.5, to assess future fracture risk. In RA patients, adequate calcium intake, up to a daily intake of 1000–1200 mg, is needed. Below this threshold, calcium supplementation is needed. Particularly in GC-treated patients, it has been suggested that the daily calcium intake should be above 1000–1200 mg/day [112, 113]. This recommended dose is slightly higher than the dose recommended for postmenopausal women not using GCs, and is related to the lower intestinal calcium absorption and increased urinary calcium excretion in GC-treated patients. An adequate 25-hydroxyvitamin D3 serum level > 50 nmol/L is advised throughout the whole year, and also at the end of winter [114]. If an osteopenic RA patient suffers from a high risk of fracture, or an RA patient has OP, in general the oral BP alendronic acid (or another oral BP such as risedronate) is the first choice as this agent has been shown to improve BMD levels in RA patients. However, sparse data indicate that the modern treatment agents denosumab and teriparatide might be superior, in RA patients, for increases in BMD and fracture rate reduction, compared with the active comparators alendronate or risedronate. Although these pivotal osteoporotic drugs are attractive as first-line therapy, the evidence is too little to include them as first-line drugs for OP in RA. Moreover, these drugs are too costly to be used in all patients. However, in certain patients with a very high fracture risk, i.e. elderly patients with RA, a (very) low BMD, or a recent nonvertebral osteoporotic fracture or known VF, second-line anti-osteoporotic agents are a very attractive option to reduce fracture risk.
We are hopeful that good implementation of the above measures will serve as an ideal form of fracture risk management and will ultimately lead to a reduction in fracture risk in vulnerable RA patients.
References
Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–99.
Symmons DP. Epidemiology of rheumatoid arthritis: determinants of onset, persistence and outcome. Best Pract Res Clin Rheumatol. 2002;16(5):707–22.
Alamanos Y, Drosos AA. Epidemiology of adult rheumatoid arthritis. Autoimmun Rev. 2005;4(3):130–6.
Raterman HG, Hoving JL, Nurmohamed MT, Herenius MM, Sluiter JK, Lems WF, et al. Work ability: a new outcome measure in rheumatoid arthritis? Scand J Rheumatol. 2010;39(2):127–31.
Turesson C, O’Fallon WM, Crowson CS, Gabriel SE, Matteson EL. Extra-articular disease manifestations in rheumatoid arthritis: incidence trends and risk factors over 46 years. Ann Rheum Dis. 2003;62(8):722–7.
Adami G, Saag KG. Osteoporosis pathophysiology, epidemiology, and screening in rheumatoid arthritis. Curr Rheumatol Rep. 2019;21(7):34.
Stach CM, Bauerle M, Englbrecht M, Kronke G, Engelke K, Manger B, et al. Periarticular bone structure in rheumatoid arthritis patients and healthy individuals assessed by high-resolution computed tomography. Arthritis Rheum. 2010;62(2):330–9.
McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365(23):2205–19.
Hecht C, Englbrecht M, Rech J, Schmidt S, Araujo E, Engelke K, et al. Additive effect of anti-citrullinated protein antibodies and rheumatoid factor on bone erosions in patients with RA. Ann Rheum Dis. 2015;74(12):2151–6.
Engdahl C, Bang H, Dietel K, Lang SC, Harre U, Schett G. Periarticular bone loss in arthritis is induced by autoantibodies against citrullinated vimentin. J Bone Miner Res. 2017;32(8):1681–91.
Nielen MM, van Schaardenburg D, Reesink HW, van de Stadt RJ, van der Horst-Bruinsma IE, de Koning MH, et al. Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum. 2004;50(2):380–6.
Kleyer A, Finzel S, Rech J, Manger B, Krieter M, Faustini F, et al. Bone loss before the clinical onset of rheumatoid arthritis in subjects with anticitrullinated protein antibodies. Ann Rheum Dis. 2014;73(5):854–60.
Orsolini G, Caimmi C, Viapiana O, Idolazzi L, Fracassi E, Gatti D, et al. Titer-dependent effect of anti-citrullinated protein antibodies on systemic bone mass in rheumatoid arthritis patients. Calcif Tissue Int. 2017;101(1):17–23.
Stemmler F, Simon D, Liphardt AM, Englbrecht M, Rech J, Hueber AJ, et al. Biomechanical properties of bone are impaired in patients with ACPA-positive rheumatoid arthritis and associated with the occurrence of fractures. Ann Rheum Dis. 2018;77(7):973–80.
Black RJ, Spargo L, Schultz C, Chatterton B, Cleland L, Lester S, et al. Decline in hand bone mineral density indicates increased risk of erosive change in early rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(4):515–22.
Haugeberg G, Uhlig T, Falch JA, Halse JI, Kvien TK. Bone mineral density and frequency of osteoporosis in female patients with rheumatoid arthritis: results from 394 patients in the Oslo County Rheumatoid Arthritis register. Arthritis Rheum. 2000;43(3):522–30.
Haugeberg G, Uhlig T, Falch JA, Halse JI, Kvien TK. Reduced bone mineral density in male rheumatoid arthritis patients: frequencies and associations with demographic and disease variables in ninety-four patients in the Oslo County Rheumatoid Arthritis Register. Arthritis Rheum. 2000;43(12):2776–84.
Lodder MC, de Jong Z, Kostense PJ, Molenaar ET, Staal K, Voskuyl AE, et al. Bone mineral density in patients with rheumatoid arthritis: relation between disease severity and low bone mineral density. Ann Rheum Dis. 2004;63(12):1576–80.
van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C. Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum. 2006;54(10):3104–12.
Cheng TT, Yu SF, Su FM, Chen YC, Su BY, Chiu WC, et al. Anti-CCP-positive patients with RA have a higher 10-year probability of fracture evaluated by FRAX(R): a registry study of RA with osteoporosis/fracture. Arthritis Res Ther. 2018;20(1):16.
Brooks PM. The burden of musculoskeletal disease—a global perspective. Clin Rheumatol. 2006;25(6):778–81.
Orstavik RE, Haugeberg G, Mowinckel P, Hoiseth A, Uhlig T, Falch JA, et al. Vertebral deformities in rheumatoid arthritis: a comparison with population-based controls. Arch Intern Med. 2004;164(4):420–5.
Bultink IE, Lems WF. Performance of vertebral fracture assessment in addition to dual energy X-ray absorptiometry in patients with rheumatoid arthritis. Rheumatology (Oxford). 2014;53(5):775–6.
Mohammad A, Lohan D, Bergin D, Mooney S, Newell J, O’Donnell M, et al. The prevalence of vertebral fracture on vertebral fracture assessment imaging in a large cohort of patients with rheumatoid arthritis. Rheumatology (Oxford). 2014;53(5):821–7.
Book C, Karlsson M, Akesson K, Jacobsson L. Disease activity and disability but probably not glucocorticoid treatment predicts loss in bone mineral density in women with early rheumatoid arthritis. Scand J Rheumatol. 2008;37(4):248–54.
van der Goes MC, Jacobs JW, Jurgens MS, Bakker MF, van der Veen MJ, van der Werf JH, et al. Are changes in bone mineral density different between groups of early rheumatoid arthritis patients treated according to a tight control strategy with or without prednisone if osteoporosis prophylaxis is applied? Osteoporos Int. 2013;24(4):1429–36.
Forslind K, Keller C, Svensson B, Hafstrom I, Group BS. Reduced bone mineral density in early rheumatoid arthritis is associated with radiological joint damage at baseline and after 2 years in women. J Rheumatol. 2003;30(12):2590–6.
Sinigaglia L, Nervetti A, Mela Q, Bianchi G, Del Puente A, Di Munno O, et al. A multicenter cross sectional study on bone mineral density in rheumatoid arthritis. Italian Study Group on Bone Mass in Rheumatoid Arthritis. J Rheumatol. 2000;27(11):2582–9.
Guler-Yuksel M, Bijsterbosch J, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Hulsmans HM, de Beus WM, et al. Changes in bone mineral density in patients with recent onset, active rheumatoid arthritis. Ann Rheum Dis. 2008;67(6):823–8.
Schett G, Stach C, Zwerina J, Voll R, Manger B. How antirheumatic drugs protect joints from damage in rheumatoid arthritis. Arthritis Rheum. 2008;58(10):2936–48.
Schett G, Saag KG, Bijlsma JW. From bone biology to clinical outcome: state of the art and future perspectives. Ann Rheum Dis. 2010;69(8):1415–9.
Vis M, Guler-Yuksel M, Lems WF. Can bone loss in rheumatoid arthritis be prevented? Osteoporos Int. 2013;24(10):2541–53.
Buttgereit F, Straub RH, Wehling M, Burmester GR. Glucocorticoids in the treatment of rheumatic diseases: an update on the mechanisms of action. Arthritis Rheum. 2004;50(11):3408–17.
Weinstein RS. Clinical practice. Glucocorticoid-induced bone disease. N Engl J Med. 2011;365(1):62–70.
Gudbjornsson B, Juliusson UI, Gudjonsson FV. Prevalence of long term steroid treatment and the frequency of decision making to prevent steroid induced osteoporosis in daily clinical practice. Ann Rheum Dis. 2002;61(1):32–6.
NIH Consensus Development Panel on Osteoporosis Prevention Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285(6):785–95.
Pasco JA, Seeman E, Henry MJ, Merriman EN, Nicholson GC, Kotowicz MA. The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporos Int. 2006;17(9):1404–9.
Felsenberg D, Boonen S. The bone quality framework: determinants of bone strength and their interrelationships, and implications for osteoporosis management. Clin Ther. 2005;27(1):1–11.
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, et al. Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1996;11(7):984–96.
Schousboe JT, Debold CR. Reliability and accuracy of vertebral fracture assessment with densitometry compared to radiography in clinical practice. Osteoporos Int. 2006;17(2):281–9.
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22(9):2395–411.
Roux S, Cabana F, Carrier N, Beaulieu M, April PM, Beaulieu MC, et al. The World Health Organization Fracture Risk Assessment Tool (FRAX) underestimates incident and recurrent fractures in consecutive patients with fragility fractures. J Clin Endocrinol Metab. 2014;99(7):2400–8.
Phuan-Udom R, Lektrakul N, Katchamart W. The association between 10-year fracture risk by FRAX and osteoporotic fractures with disease activity in patients with rheumatoid arthritis. Clin Rheumatol. 2018;37(10):2603–10.
Kanis JA, Johansson H, Oden A, Harvey NC, Gudnason V, Sanders KM, et al. Characteristics of recurrent fractures. Osteoporos Int. 2018;29(8):1747–57.
Elde KD, Madsen OR. FRAX 10-yr fracture risk in rheumatoid arthritis-assessments with and without bone mineral density may lead to very different results in the individual patient. J Clin Densitom. 2019;22(1):31–8.
Kanis JA, Johnell O, Oden A, Johansson H, De LC, Eisman JA, et al. Smoking and fracture risk: a meta-analysis. Osteoporos Int. 2005;16(2):155–62.
Kanis JA, Johansson H, Johnell O, Oden A, De LC, Eisman JA, et al. Alcohol intake as a risk factor for fracture. Osteoporos Int. 2005;16(7):737–42.
Sioen I, Michels N, Polfliet C, De SS, D’Haese S, Roggen I, et al. The influence of dairy consumption, sedentary behaviour and physical activity on bone mass in Flemish children: a cross-sectional study. BMC Public Health. 2015;15:717.
Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS, Gamble GD, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.
van Halm VP, Peters MJ, Voskuyl AE, Boers M, Lems WF, Visser M, et al. Rheumatoid arthritis versus diabetes as a risk factor for cardiovascular disease: a cross-sectional study, the CARRE Investigation. Ann Rheum Dis. 2009;68(9):1395–400.
Ni Mhuircheartaigh O, Crowson CS, Gabriel SE, Roger VL, Melton LJ 3rd, Amin S. Fragility fractures are associated with an increased risk for cardiovascular events in women and men with rheumatoid arthritis: a population-based study. J Rheumatol. 2017;44(5):558–64.
Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ, Lyons RA, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367(1):40–9.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Allen CS, Yeung JH, Vandermeer B, Homik J. Bisphosphonates for steroid-induced osteoporosis. Cochrane Database Syst Rev. 2016;10:CD001347.
Lems WF, Lodder MC, Lips P, Bijlsma JW, Geusens P, Schrameijer N, et al. Positive effect of alendronate on bone mineral density and markers of bone turnover in patients with rheumatoid arthritis on chronic treatment with low-dose prednisone: a randomized, double-blind, placebo-controlled trial. Osteoporos Int. 2006;17(5):716–23.
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344(19):1434–41.
Saag KG, Shane E, Boonen S, Marin F, Donley DW, Taylor KA, et al. Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med. 2007;357(20):2028–39.
Saag KG, Zanchetta JR, Devogelaer JP, Adler RA, Eastell R, See K, et al. Effects of teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: thirty-six-month results of a randomized, double-blind, controlled trial. Arthritis Rheum. 2009;60(11):3346–55.
Karras D, Stoykov I, Lems WF, Langdahl BL, Ljunggren O, Barrett A, et al. Effectiveness of teriparatide in postmenopausal women with osteoporosis and glucocorticoid use: 3-year results from the EFOS study. J Rheumatol. 2012;39(3):600–9.
Ebina K, Hashimoto J, Shi K, Kashii M, Hirao M, Yoshikawa H. Comparison of the effect of 18-month daily teriparatide administration on patients with rheumatoid arthritis and postmenopausal osteoporosis patients. Osteoporos Int. 2014;25(12):2755–65.
Ebina K, Hirao M, Hashimoto J, Hagihara K, Kashii M, Kitaguchi K, et al. Assessment of the effects of switching oral bisphosphonates to denosumab or daily teriparatide in patients with rheumatoid arthritis. J Bone Miner Metab. 2018;36(4):478–87.
Langdahl BL, Silverman S, Fujiwara S, Saag K, Napoli N, Soen S, et al. Real-world effectiveness of teriparatide on fracture reduction in patients with osteoporosis and comorbidities or risk factors for fractures: integrated analysis of 4 prospective observational studies. Bone. 2018;116:58–66.
Miller PD. A review of the efficacy and safety of denosumab in postmenopausal women with osteoporosis. Ther Adv Musculoskelet Dis. 2011;3(6):271–82.
Lewiecki EM. New and emerging concepts in the use of denosumab for the treatment of osteoporosis. Ther Adv Musculoskelet Dis. 2018;10(11):209–23.
Cummings SR, San MJ, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–65.
Saag KG, Wagman RB, Geusens P, Adachi JD, Messina OD, Emkey R, et al. Denosumab versus risedronate in glucocorticoid-induced osteoporosis: a multicentre, randomised, double-blind, active-controlled, double-dummy, non-inferiority study. Lancet Diabetes Endocrinol. 2018;6(6):445–54.
Saag KG, Pannacciulli N, Geusens P, Adachi JD, Messina OD, Morales-Torres J, et al. Denosumab vs risedronate in glucocorticoid-induced osteoporosis: final results of a 24-month randomized, double-blind, double-dummy trial. Arthritis Rheumatol. 2019;71(7):1174–84.
Takeuchi T, Tanaka Y, Ishiguro N, Yamanaka H, Yoneda T, Ohira T, et al. Effect of denosumab on Japanese patients with rheumatoid arthritis: a dose–response study of AMG 162 (Denosumab) in patients with RheumatoId arthritis on methotrexate to Validate inhibitory effect on bone Erosion (DRIVE)-a 12-month, multicentre, randomised, double-blind, placebo-controlled, phase II clinical trial. Ann Rheum Dis. 2016;75(6):983–90.
Takeuchi T, Tanaka Y, Soen S, Yamanaka H, Yoneda T, Tanaka S, et al. Effects of the anti-RANKL antibody denosumab on joint structural damage in patients with rheumatoid arthritis treated with conventional synthetic disease-modifying antirheumatic drugs (DESIRABLE study): a randomised, double-blind, placebo-controlled phase 3 trial. Ann Rheum Dis. 2019;78(7):899–907.
Hasegawa T, Kaneko Y, Izumi K, Takeuchi T. Efficacy of denosumab combined with bDMARDs on radiographic progression in rheumatoid arthritis. Joint Bone Spine. 2017;84(3):379–80.
Suzuki T, Nakamura Y, Kato H. Effects of denosumab on bone metabolism and bone mineral density with anti-TNF inhibitors, tocilizumab, or abatacept in osteoporosis with rheumatoid arthritis. Ther Clin Risk Manag. 2018;14:453–9.
Boleto G, Drame M, Lambrecht I, Eschard JP, Salmon JH. Disease-modifying anti-rheumatic drug effect of denosumab on radiographic progression in rheumatoid arthritis: a systematic review of the literature. Clin Rheumatol. 2017;36(8):1699–706.
Suzuki T, Nakamura Y, Kato H. Calcium and vitamin D supplementation with 3-year denosumab treatment is beneficial to enhance bone mineral density in postmenopausal patients with osteoporosis and rheumatoid arthritis. Ther Clin Risk Manag. 2019;15:15–22.
Dirven L, Guler-Yuksel M, de Beus WM, Ronday HK, Speyer I, Huizinga TW, et al. Changes in hand bone mineral density and the association with the level of disease activity in patients with rheumatoid arthritis: bone mineral density measurements in a multicenter randomized clinical trial. Arthritis Care Res (Hoboken). 2011;63(12):1691–9.
Buckley LM, Leib ES, Cartularo KS, Vacek PM, Cooper SM. Effects of low dose methotrexate on the bone mineral density of patients with rheumatoid arthritis. J Rheumatol. 1997;24(8):1489–94.
Minaur NJ, Kounali D, Vedi S, Compston JE, Beresford JN, Bhalla AK. Methotrexate in the treatment of rheumatoid arthritis. II: In vivo effects on bone mineral density. Rheumatology (Oxford). 2002;41(7):741–9.
di Munno O, Mazzantini M, Sinigaglia L, Bianchi G, Minisola G, Muratore M, et al. Effect of low dose methotrexate on bone density in women with rheumatoid arthritis: results from a multicenter cross-sectional study. J Rheumatol. 2004;31(7):1305–9.
Carbone LD, Kaeley G, McKown KM, Cremer M, Palmieri G, Kaplan S. Effects of long-term administration of methotrexate on bone mineral density in rheumatoid arthritis. Calcif Tissue Int. 1999;64(2):100–1.
Mazzantini M, Di Munno O, Incerti-Vecchi L, Pasero G. Vertebral bone mineral density changes in female rheumatoid arthritis patients treated with low-dose methotrexate. Clin Exp Rheumatol. 2000;18(3):327–31.
Cranney AB, McKendry RJ, Wells GA, Ooi DS, Kanigsberg ND, Kraag GR, et al. The effect of low dose methotrexate on bone density. J Rheumatol. 2001;28(11):2395–9.
May KP, West SG, McDermott MT, Huffer WE. The effect of low-dose methotrexate on bone metabolism and histomorphometry in rats. Arthritis Rheum. 1994;37(2):201–6.
Ragab AH, Frech RS, Vietti TJ. Osteoporotic fractures secondary to methotrexate therapy of acute leukemia in remission. Cancer. 1970;25(3):580–5.
Kwon OC, Oh JS, Hong S, Lee CK, Yoo B, Kim YG. Conventional synthetic disease-modifying antirheumatic drugs and bone mineral density in rheumatoid arthritis patients with osteoporosis: possible beneficial effect of leflunomide. Clin Exp Rheumatol. 2019;37(5):813–9.
Walsh NC, Gravallese EM. Bone remodeling in rheumatic disease: a question of balance. Immunol Rev. 2010;233(1):301–12.
Daoussis D, Andonopoulos AP. The emerging role of Dickkopf-1 in bone biology: is it the main switch controlling bone and joint remodeling? Semin Arthritis Rheum. 2011;41(2):170–7.
Vis M, Wolbink GJ, Lodder MC, Kostense PJ, van de Stadt RJ, de Koning MH, et al. Early changes in bone metabolism in rheumatoid arthritis patients treated with infliximab. Arthritis Rheum. 2003;48(10):2996–7.
Zerbini CAF, Clark P, Mendez-Sanchez L, Pereira RMR, Messina OD, Una CR, et al. Biologic therapies and bone loss in rheumatoid arthritis. Osteoporos Int. 2017;28(2):429–46.
Seriolo B, Paolino S, Sulli A, Ferretti V, Cutolo M. Bone metabolism changes during anti-TNF-alpha therapy in patients with active rheumatoid arthritis. Ann N Y Acad Sci. 2006;1069:420–7.
Krieckaert CL, Nurmohamed MT, Wolbink G, Lems WF. Changes in bone mineral density during long-term treatment with adalimumab in patients with rheumatoid arthritis: a cohort study. Rheumatology (Oxford). 2013;52(3):547–53.
Kim SY, Schneeweiss S, Liu J, Solomon DH. Effects of disease-modifying antirheumatic drugs on nonvertebral fracture risk in rheumatoid arthritis: a population-based cohort study. J Bone Miner Res. 2012;27(4):789–96.
Kawai VK, Grijalva CG, Arbogast PG, Curtis JR, Solomon DH, Delzell E, et al. Initiation of tumor necrosis factor alpha antagonists and risk of fractures in patients with selected rheumatic and autoimmune diseases. Arthritis Care Res (Hoboken). 2013;65(7):1085–94.
Coulson KA, Reed G, Gilliam BE, Kremer JM, Pepmueller PH. Factors influencing fracture risk, T score, and management of osteoporosis in patients with rheumatoid arthritis in the Consortium of Rheumatology Researchers of North America (CORRONA) registry. J Clin Rheumatol. 2009;15(4):155–60.
Ozen G, Pedro S, Wolfe F, Michaud K. Medications associated with fracture risk in patients with rheumatoid arthritis. Ann Rheum Dis. 2019;78(8):1041–7.
Garnero P, Thompson E, Woodworth T, Smolen JS. Rapid and sustained improvement in bone and cartilage turnover markers with the anti-interleukin-6 receptor inhibitor tocilizumab plus methotrexate in rheumatoid arthritis patients with an inadequate response to methotrexate: results from a substudy of the multicenter double-blind, placebo-controlled trial of tocilizumab in inadequate responders to methotrexate alone. Arthritis Rheum. 2010;62(1):33–43.
Boyapati A, Msihid J, Fiore S, van Adelsberg J, Graham NM, Hamilton JD. Sarilumab plus methotrexate suppresses circulating biomarkers of bone resorption and synovial damage in patients with rheumatoid arthritis and inadequate response to methotrexate: a biomarker study of MOBILITY. Arthritis Res Ther. 2016;18(1):225.
Abu-Shakra M, Zisman D, Balbir-Gurman A, Amital H, Levy Y, Langevitz P, et al. Effect of tocilizumab on fatigue and bone mineral density in patients with rheumatoid arthritis. Isr Med Assoc J. 2018;20(4):239–44.
Chen YM, Chen HH, Huang WN, Liao TL, Chen JP, Chao WC, et al. Tocilizumab potentially prevents bone loss in patients with anticitrullinated protein antibody-positive rheumatoid arthritis. PLoS One. 2017;12(11):e0188454.
Boumans MJ, Thurlings RM, Yeo L, Scheel-Toellner D, Vos K, Gerlag DM, et al. Rituximab abrogates joint destruction in rheumatoid arthritis by inhibiting osteoclastogenesis. Ann Rheum Dis. 2012;71(1):108–13.
Hein G, Eidner T, Oelzner P, Rose M, Wilke A, Wolf G, et al. Influence of Rituximab on markers of bone remodeling in patients with rheumatoid arthritis: a prospective open-label pilot study. Rheumatol Int. 2011;31(2):269–72.
Salvin SQL, Maset M, Corazza L, DeMarchi G, Lombardi S, et al. Variations in lumbar spine and femoral BMD after rituximab therapy in active rheumatoid arthritis. Ann Rheum Dis. 2010;69:704.
Keywani K, Raterman H, ter Wee MM, Nurmohamed MT, Voskuyl AE, Bultink Bultink IE, Lems WF. The arrest of bone mineral density loss at the lumbar spine and hip in patients with active rheumatoid arthritis during rituximab therapy. Ann Rheum Dis. 2018;77:A933.
Wheater G, Elshahaly M, Naraghi K, Tuck SP, Datta HK, van Laar JM. Changes in bone density and bone turnover in patients with rheumatoid arthritis treated with rituximab, results from an exploratory, prospective study. PLoS One. 2018;13(8):e0201527.
Axmann R, Herman S, Zaiss M, Franz S, Polzer K, Zwerina J, et al. CTLA-4 directly inhibits osteoclast formation. Ann Rheum Dis. 2008;67(11):1603–9.
Bozec A, Zaiss MM, Kagwiria R, Voll R, Rauh M, Chen Z, et al. T cell costimulation molecules CD80/86 inhibit osteoclast differentiation by inducing the IDO/tryptophan pathway. Sci Transl Med. 2014;6(235):235ra60.
Tada M, Inui K, Sugioka Y, Mamoto K, Okano T, Koike T. Abatacept might increase bone mineral density at femoral neck for patients with rheumatoid arthritis in clinical practice: AIRTIGHT study. Rheumatol Int. 2018;38(5):777–84.
Murakami K, Kobayashi Y, Uehara S, Suzuki T, Koide M, Yamashita T, et al. A Jak1/2 inhibitor, baricitinib, inhibits osteoclastogenesis by suppressing RANKL expression in osteoblasts in vitro. PLoS One. 2017;12(7):e0181126.
Vidal B, Cascao R, Finnila MAJ, Lopes IP, da Gloria VG, Saarakkala S, et al. Effects of tofacitinib in early arthritis-induced bone loss in an adjuvant-induced arthritis rat model. Rheumatology (Oxford). 2018;57(8):1461–71.
Mazzucchelli R, Perez Fernandez E, Crespi-Villarias N, Quiros-Donate J, Garcia Vadillo A, Espinosa M, et al. Trends in hip fracture in patients with rheumatoid arthritis: results from the Spanish National Inpatient Registry over a 17-year period (1999–2015). TREND-AR study. RMD Open. 2018;4(1):e000671.
Blavnsfeldt AG, de Thurah A, Thomsen MD, Tarp S, Langdahl B, Hauge EM. The effect of glucocorticoids on bone mineral density in patients with rheumatoid arthritis: a systematic review and meta-analysis of randomized, controlled trials. Bone. 2018;114:172–80.
Cheng TT, Lai HM, Yu SF, Chiu WC, Hsu CY, Chen JF, et al. The impact of low-dose glucocorticoids on disease activity, bone mineral density, fragility fractures, and 10-year probability of fractures in patients with rheumatoid arthritis. J Investig Med. 2018;66(6):1004–7.
Lems WF, Raterman HG, van den Bergh JP, Bijlsma HW, Valk NK, Zillikens MC, et al. Osteopenia: a diagnostic and therapeutic challenge. Curr Osteoporos Rep. 2011;9(3):167–72.
Buckley L, Guyatt G, Fink HA, Cannon M, Grossman J, Hansen KE, et al. 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheumatol. 2017;69(8):1521–37.
Briot K, Roux C. Glucocorticoid-induced osteoporosis. RMD Open. 2015;1(1):e000014.
Lips P. Relative value of 25(OH)D and 1,25(OH)2D measurements. J Bone Miner Res. 2007;22(11):1668–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hennie G. Raterman has received an unrestricted educational grant from UCB, and consulting fees from Amgen, Cellgene and Sanof Genzyme. Willem F. Lems has received a grant from Pfizer, and consulting fees from MSD, Amgen, Lilly, Pfizer and UCB.
Funding
No funding was received for the preparation of this manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Raterman, H.G., Lems, W.F. Pharmacological Management of Osteoporosis in Rheumatoid Arthritis Patients: A Review of the Literature and Practical Guide. Drugs Aging 36, 1061–1072 (2019). https://doi.org/10.1007/s40266-019-00714-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00714-4