Abstract
Background and Objective
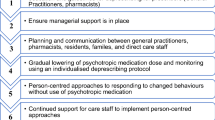
Psychotropic drug use is high in nursing homes in Belgium. A practice improvement initiative (including education, professional support and the transition towards person-centred care) achieved significant reductions in psychotropic drug use. The initiative outline was transcribed into a general intervention template, and consequently implemented in five nursing homes (in mixed locations and with a mixed character) in preparation for a future broader roll-out in Belgium. The impact of the intervention on the use of psychotropic drugs in these five nursing homes is reported in this paper.
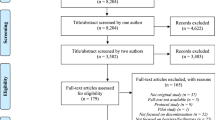
Methods
The general intervention template was fitted into the individual nursing home setting. Education for the nursing home personnel on psychotropic drugs and non-pharmacological alternatives, as well as details for a transition to person-centred care was provided. Psychotropic drug use was recorded using a dynamic cohort study design with cross-sectional observations (November 2016–November 2017).
Results
At baseline, participants’ (n = 677) mean age was 85.6 years (range 54–109 years), with 72.6% female. Mean medication intake was 8.5 (range 1–22), predominantly central nervous system drugs (Anatomic Therapeutic Chemical classification N, 88.8%). Long-term (> 3 months) psychotropic drug use (62.0%) and concomitant psychotropic drug use (31.5% taking two or more medications) were high. After 12 months, the prevalence of long-term psychotropic drug use decreased significantly (from 62.0 to 52.9%, p < 0.001), likewise the combined use of psychotropic drugs (from 31.5 to 24.0%, p = 0.001). The decrease in the prevalence of antidepressant and hypnosedative use was significant (respectively, from 32.2 to 23.4%, p < 0.001, and from 35.3 to 28.7%, p = 0.006) in contrast to antipsychotic use (from 17.1 to 15.9%, p = 0.522).
Conclusions
The stand-alone adaptation of the previously reported initiative using a general template was possible. This intervention resulted in a significant decrease in psychotropic drug use (predominantly hypnosedatives and antidepressants) among nursing home residents after 12 months.




Similar content being viewed by others
References
Schüssler S, Dassen T, Lohrmann C. Care dependency and nursing care problems in nursing home residents with and without dementia: a cross-sectional study. Aging Clin Exp Res. 2016;28:973–82.
Ivanova I, Wauters M, Stichele RV, Christiaens T, De Wolf J, Dilles T, et al. Medication use in a cohort of newly admitted nursing home residents (Ageing@NH) in relation to evolving physical and mental health. Arch Gerontol Geriatr. 2018;75:202–8.
Mann E, Köpke S, Haastert B, Pitkälä K, Meyer G, Alanen H, et al. Psychotropic medication use among nursing home residents in Austria: a cross-sectional study. BMC Geriatr. 2009;9:18.
Hollingworth SA, Siskind DJ, Nissen LM, Robinson M, Hall WD. Patterns of antipsychotic medication use in Australia 2002–2007. Aust N Z J Psychiatry. 2010;44:372–7.
Sterke CS, van Beeck EF, van der Velde N, Ziere G, Petrovic M, Looman CWN, et al. New insights: dose-response relationship between psychotropic drugs and falls: a study in nursing home residents with dementia. J Clin Pharmacol. 2012;52:947–55.
National Institute for Health and Care Excellence (UK). Dementia: assessment, management and support for people living with dementia and their carers. London: National Institute for Health and Care Excellence (UK); 2018.
Barnes TRE, Banerjee S, Collins N, Treloar A, McIntyre SM, Paton C. Antipsychotics in dementia: prevalence and quality of antipsychotic drug prescribing in UK mental health services. Br J Psychiatry. 2012;201:221–6.
Selbæk G, Kirkevold Ø, Engedal K. The course of psychiatric and behavioral symptoms and the use of psychotropic medication in patients with dementia in Norwegian nursing homes: a 12-month follow-up study. Am J Geriatr Psychiatry. 2008;16:528–36.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–43.
Azermai M, Elseviers M, Petrovic M, Van Bortel L, Vander Stichele R. Geriatric drug utilisation of psychotropics in Belgian nursing homes. Hum Psychopharmacol. 2011;26:12–20.
Elseviers MM, Vander Stichele RR, Van Bortel L. Quality of prescribing in Belgian nursing homes: an electronic assessment of the medication chart. Int J Qual Health Care. 2014;26:93–9.
Anrys PMS, Strauven GC, Foulon V, Degryse J-M, Henrard S, Spinewine A. Potentially inappropriate prescribing in Belgian nursing homes: prevalence and associated factors. J Am Med Dir Assoc. 2018;19:884–90.
Azermai M, Wauters M, De Meester D, Renson L, Pauwels D, Peeters L, et al. A quality improvement initiative on the use of psychotropic drugs in nursing homes in Flanders. Acta Clin Belg. 2017;72:163–71.
De Vriendt P, Cornelis E, Vanbosseghem R, Desmet V, Van de Velde D. Enabling meaningful activities and quality of life in long-term care facilities: the stepwise development of a participatory client-centred approach in Flanders. Br J Occup Ther. 2019;82(1):15–26. https://doi.org/10.1177/0308022618775880.
Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivelä S-L, Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002;55:809–17.
Stevenson DG, Decker SL, Dwyer LL, Huskamp HA, Grabowski DC, Metzger ED, et al. Antipsychotic and benzodiazepine use among nursing home residents: findings from the 2004 National Nursing Home Survey. Am J Geriatr Psychiatry. 2010;18:1078–92.
Stock KJ, Amuah JE, Lapane KL, Hogan DB, Maxwell CJ. Prevalence of, and resident and facility characteristics associated with antipsychotic use in assisted living vs. long-term care facilities: a cross-sectional analysis from Alberta, Canada. Drugs Aging. 2017;34:39–53.
van der Spek K, Gerritsen DL, Smalbrugge M, Nelissen-Vrancken MHJMG, Wetzels RB, Smeets CHW, et al. Only 10% of the psychotropic drug use for neuropsychiatric symptoms in patients with dementia is fully appropriate: the PROPER I-study. Int Psychogeriatrics. 2016;28:1589–95.
Allers K, Dörks M, Schmiemann G, Hoffmann F. Antipsychotic drug use in nursing home residents with and without dementia. Int Clin Psychopharmacol. 2017;32:213–8.
MacPherson S, Davison TE, Hallford D, Mellor D, Seedy M, Bird M, et al. Behavioral symptoms of dementia that present management difficulties in nursing homes: staff perceptions and their concordance with informant scales. J Gerontol Nurs. 2016;43:34–43.
Tjia J, Lemay CA, Bonner A, Compher C, Paice K, Field T, et al. Informed family member involvement to improve the quality of dementia care in nursing homes. J Am Geriatr Soc. 2017;65:59–65.
Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, et al. Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2013;(3):CD007726.
Van Leeuwen E, Petrovic M, van Driel ML, De Sutter AI, Vander Stichele R, Declercq T, et al. Withdrawal versus continuation of long-term antipsychotic drug use for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2018;3:CD007726.
Van Leeuwen E, Petrovic M, van Driel ML, De Sutter AI, Stichele R Vander, Declercq T, et al. Discontinuation of long-term antipsychotic drug use for behavioral and psychological symptoms in older adults aged 65 years and older with dementia. J Am Med Dir Assoc. 2018;19:1009–14.
Gould RL, Coulson MC, Patel N, Highton-Williamson E, Howard RJ. Interventions for reducing benzodiazepine use in older people: meta-analysis of randomised controlled trials. Br J Psychiatry. 2014;204:98–107.
de Souto Barreto P, Lapeyre-Mestre M, Cestac P, Vellas B, Rolland Y. Effects of a geriatric intervention aiming to improve quality care in nursing homes on benzodiazepine use and discontinuation. Br J Clin Pharmacol. 2016;81:759–67.
Westbury J, Jackson S, Gee P, Peterson G. An effective approach to decrease antipsychotic and benzodiazepine use in nursing homes: the RedUSe project. Int Psychogeriatr. 2010;22:26–36.
Westbury J, Tichelaar L, Peterson G, Gee P, Jackson S. A 12-month follow-up study of “RedUSe”: a trial aimed at reducing antipsychotic and benzodiazepine use in nursing homes. Int Psychogeriatr. 2011;23:1260–9.
Westbury JL, Gee P, Ling T, Brown DT, Franks KH, Bindoff I, et al. RedUSe: reducing antipsychotic and benzodiazepine prescribing in residential aged care facilities. Med J Aust. 2018;208:398–403.
Richter T, Mann E, Meyer G, Haastert B, Köpke S. Prevalence of psychotropic medication use among German and Austrian nursing home residents: a comparison of 3 cohorts. J Am Med. Dir Assoc. 2012;13(187):e7–13.
Hughes CM, Lapane K, Watson MC, Davies HTO. Does organisational culture influence prescribing in care homes for older people? A new direction for research. Drugs Aging. 2007;24:81–93.
Leten L, Azermai M, Wauters M, De Lepeleire J. Een kwalitatieve exploratie van het chronisch gebruik van psychofarmaca in woonzorgcentraA qualitative exploration of the chronic use of psychotropic drugs in nursing homes. Tijdschr Gerontol Geriatr. 2017;48:177–86.
Cabrera E, Sutcliffe C, Verbeek H, Saks K, Soto-Martin M, Meyer G, et al. Non-pharmacological interventions as a best practice strategy in people with dementia living in nursing homes: a systematic review. Eur Geriatr Med. 2015;6:134–50.
Chen R-C, Liu C-L, Lin M-H, Peng L-N, Chen L-Y, Liu L-K, et al. Non-pharmacological treatment reducing not only behavioral symptoms, but also psychotic symptoms of older adults with dementia: a prospective cohort study in Taiwan. Geriatr Gerontol Int. 2014;14:440–6.
Martin P, Tannenbaum C, Ahmed S, Tamblyn R, Benedetti A. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education. JAMA Intern Med. 2014;174:890–8.
Lawrence V, Fossey J, Ballard C, Moniz-Cook E, Murray J. Improving quality of life for people with dementia in care homes: making psychosocial interventions work. Br J Psychiatry. 2012;201:344–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for the conduct of this study was received from the Flemish Agency for Care and Health (Vlaams Agentschap voor Zorg en Gezondheid).
Conflict of interest
Maarten Wauters, Monique Elseviers, Laurine Peeters, Dirk De Meester, Thierry Christiaens and Mirko Petrovic have no conflicts of interest that are directly relevant to the content of this article. The authors received no support from any organisation for the submitted work, have no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years, and no other relationships or activities that could appear to have influenced the submitted work.
Rights and permissions
About this article
Cite this article
Wauters, M., Elseviers, M., Peeters, L. et al. Reducing Psychotropic Drug Use in Nursing Homes in Belgium: An Implementation Study for the Roll-Out of a Practice Improvement Initiative. Drugs Aging 36, 769–780 (2019). https://doi.org/10.1007/s40266-019-00686-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00686-5