Abstract
Background
Older adults living with dementia may have a higher risk of medication toxicity than those without dementia. Optimising prescribing in this group of people is a critically important yet challenging process.
Objective
Our aim was to systematically review the evidence for the effectiveness of interventions for optimising prescribing in older people with dementia.
Methods
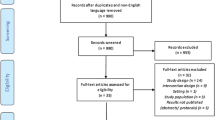
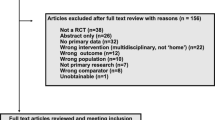
This systematic review searched the Pubmed, Embase, CINAHL, PsycINFO and Cochrane Library electronic databases for studies that evaluated relevant interventions. Experimental, quasi-experimental and observational studies published in English prior to August 2018 were included. Data were synthesised at a narrative level.
Results
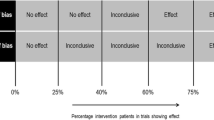
The 18 studies accepted for review included seven randomised, two nonrandomised controlled, five quasi-experimental and four observational studies. Half the studies were conducted in nursing homes and the other half in hospital and community settings. There was great variability in the interventions and outcomes reported and a meta-analysis was not feasible. The three randomised and four nonrandomised studies examining medication appropriateness all reported improvements on at least one measure of the outcome. Six studies reported on interventions that identified and resolved drug-related problems. The results for other outcomes, including the number of medications (10 studies), healthcare utilisation (7 studies), mortality (7 studies), quality of life (3 studies) and falls (3 studies), were mixed and difficult to synthesise because of variability in the study design and measures used.
Conclusion
Emerging evidence suggests that interventions in older people with dementia may have positive effects on medication appropriateness and resolution of drug-related problems; however, whether optimisation of medication results in clinically meaningful outcomes remains uncertain.


Similar content being viewed by others
References
Guideline Adaptation Committee. Clinical practice guidelines and principles of care for people with dementia. Sydney: Guideline Adaptation Committee; 2016.
Reeve E, Bell SJ, Hilmer SN. Barriers to optimising prescribing and deprescribing in older adults with dementia: a narrative review. Curr Clin Pharmacol. 2015;10(3):168–77.
Page A, Etherton-Beer C, Seubert LJ, Clark V, King S, Clifford RM. Medication use to manage comorbidities for people with dementia: a systematic review. J Pharm Pract Res. 2018;48:356–67.
World Health Organization. Dementia. http://www.who.int/mediacentre/factsheets/fs362/en/. Accessed 3 Jan 2018.
Andersen F, Viitanen M, Halvorsen DS, Straume B, Engstad TA. Co-morbidity and drug treatment in Alzheimer’s disease. A cross sectional study of participants in the Dementia Study in Northern Norway. BMC Geriatr. 2011;11(1):58.
Bunn F, Burn A-M, Goodman C, Rait G, Norton S, Robinson L, et al. Comorbidity and dementia: a scoping review of the literature. BMC Med. 2014;12:192–206.
Clague F, Mercer SW, McLean G, Reynish E, Guthrie B. Comorbidity and polypharmacy in people with dementia: insights from a large, population-based cross-sectional analysis of primary care data. Age Ageing. 2017;46(1):33–9.
Kristensen RU, Norgaard A, Jensen-Dahm C, Gasse C, Wimberley T, Waldemar G. Polypharmacy and potentially inappropriate medication in people with dementia: a nationwide study. J Alzheimers Dis. 2018;63(1):383–94.
Somers M, Rose E, Simmonds D, Whitelaw C, Calver J, Beer C. Quality use of medicines in residential aged care. Aust Fam Phys. 2010;39(6):413.
Kuijpers MA, Van Marum RJ, Egberts AC, Jansen PA. Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol. 2008;65(1):130–3.
Tan ECK, Jokanovic N, Koponen MPH, Thomas D, Hilmer SN, Bell SJ. Prevalence of analgesic use and pain in people with and without dementia or cognitive impairment in aged care facilities: a systematic review and meta-analysis. Curr Clin Pharmacol. 2015;10(3):194–203.
Parsons C. Polypharmacy and inappropriate medication use in patients with dementia: an underresearched problem. Ther Adv Drug Saf. 2017;8(1):31–46.
Lau DT, Mercaldo ND, Harris AT, Trittschuh E, Shega J, Weintraub S. Polypharmacy and potentially inappropriate medication use among community-dwelling elders with dementia. Alzheimer Dis Assoc Disord. 2010;24(1):56.
Johnell K. Inappropriate drug use in people with cognitive impairment and dementia: a systematic review. Curr Clin Pharmacol. 2015;10(3):178–84.
Redston MR, Hilmer SN, McLachlan AJ, Clough AJ, Gnjidic D. Prevalence of potentially inappropriate medication use in older inpatients with and without cognitive impairment: a systematic review. J Alzheimers Dis. 2018;61(4):1639–52.
Ramsey CM, Gnjidic D, Agogo GO, Allore H, Moga D. Longitudinal patterns of potentially inappropriate medication use following incident dementia diagnosis. Alzheimers Dement Transl Res Clin Interv. 2018;4:1–10.
Bosboom PR, Alfonso H, Almeida OP, Beer C. Use of potentially harmful medications and health-related quality of life among people with dementia living in residential aged care facilities. Dement Geriatr Cogn Disord Extra. 2012;2(1):361–71.
Renom-Guiteras A, Thurmann PA, Miralles R, Klaassen-Mielke R, Thiem U, Stephan A, et al. Potentially inappropriate medication among people with dementia in eight European countries. Age Ageing. 2018;47(1):68–74.
Walsh KA, O’Riordan D, Kearney PM, Timmons S, Byrne S. Improving the appropriateness of prescribing in older patients: a systematic review and meta-analysis of pharmacists’ interventions in secondary care. Age Ageing. 2016;45(2):201–9.
Page A, Potter K, Clifford R, McLachlan AJ, Etherton-Beer C. Medication appropriateness tool for co-morbid health conditions in dementia: consensus recommendations from a multidisciplinary expert panel. Intern Med J. 2016;46(10):1189–97.
Reeve E, Trenaman SC, Rockwood K, Hilmer SN. Pharmacokinetic and pharmacodynamic alterations in older people with dementia. Expert Opin Drug Metab Toxicol. 2017;13(6):651–68.
Van Spall HG, Toren A, Kiss A, Fowler RA. Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. JAMA. 2007;297(11):1233–40.
Alldred DP, Raynor DK, Hughes C, Barber N, Chen T, Spoor P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD009095.pub2.
McGrattan M, Ryan C, Barry HE, Hughes CM. Interventions to improve medicines management for people with dementia: a systematic review. Drugs Aging. 2017;34(12):907–16.
Alldred DP, Kennedy MC, Hughes C, Chen TF, Miller P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD009095.pub3.
Cooper JA, Cadogan CA, Patterson SM, Kerse N, Bradley MC, Ryan C, et al. Interventions to improve the appropriate use of polypharmacy in older people: a Cochrane systematic review. BMJ Open. 2015;5(12):e009235.
Clyne B, Fitzgerald C, Quinlan A, Hardy C, Galvin R, Fahey T, et al. Interventions to address potentially inappropriate prescribing in community-dwelling older adults: a systematic review of randomized controlled trials. J Am Geriatr Soc. 2016;64(6):1210–22.
Patterson SM, Cadogan CA, Kerse N, Cardwell CR, Bradley MC, Ryan C, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD008165.pub3.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Shafiee Hanjani L, Long D, Peel N, Peeters G, Freeman C, Hubbard R. Interventions to optimise prescribing in older people with dementia. PROSPERO 2017 (CRD42017073358). http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017073358. Accessed 1 Nov 2018.
Hartmaier SL, Sloane PD, Guess HA, Koch GG, Mitchell CM, Phillips CD. Validation of the minimum data set cognitive performance scale: agreement with the mini-mental state examination. J Gerontol A Biol Sci Med Sci. 1995;50(2):M128–33.
Coon JT, Abbott R, Rogers M, Whear R, Pearson S, Lang I, et al. Interventions to reduce inappropriate prescribing of antipsychotic medications in people with dementia resident in care homes: a systematic review. J Am Med Dir Assoc. 2014;15(10):706–18.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
National Institutes of Health. Quality assessment tool for before-after (pre-post) studies with no control group. Systematic evidence reviews and clinical practice guidelines. Washington, DC: National Institutes of Health; 2014.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: University of Ottawa; 2001. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 17 Jan 2018.
Gustafsson M, Sjölander M, Pfister B, Jonsson J, Schneede J, Lövheim H. Pharmacist participation in hospital ward teams and hospital readmission rates among people with dementia: a randomized controlled trial. Eur J Clin Pharmacol. 2017;73:827–35.
Potter K, Flicker L, Page A, Etherton-Beer C. Deprescribing in frail older people: a randomised controlled trial. PLoS One. 2016;11(3):e0149984.
Jordan S, Gabe-Walters ME, Watkins A, Humphreys I, Newson L, Snelgrove S, et al. Nurse-led medicines’ monitoring for patients with dementia in care homes: a pragmatic cohort stepped wedge cluster randomised trial. PLoS ONE. 2015;10(10):e0140203.
Pitkälä KH, Juola A-L, Kautiainen H, Soini H, Finne-Soveri UH, Bell JS, et al. Education to reduce potentially harmful medication use among residents of assisted living facilities: a randomized controlled trial. J Am Med Dir Assoc. 2014;15(12):892–8.
Zermansky AG, Alldred DP, Petty DR, Raynor DK, Freemantle N, Eastaugh J, et al. Clinical medication review by a pharmacist of elderly people living in care homes—randomised controlled trial. Age Ageing. 2006;35(6):586–91.
Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing. 2004;33(6):612–7.
Furniss L, Burns A, Craig SKL, Scobie S, Cooke J, Faragher B. Effects of a pharmacist’s medication review in nursing homes. Randomised controlled trial. Br J Psychiatry. 2000;176:563–7.
Sakakibara M, Igarashi A, Takase Y, Kamei H, Nabeshima T. Effects of prescription drug reduction on quality of life in community-dwelling patients with dementia. J Pharm Pharm Sci. 2015;18(5):705–12.
Garfinkel D, Zur-Gil S, Ben-Israel J. The war against polypharmacy: a new cost-effective geriatric-positive approach for improving drug therapy in disabled elderly people. Isr Med Assoc J. 2007;9(6):430–4.
Jordan S, Gabe M, Newson L, Snelgrove S, Panes G, Picek A, et al. Medication monitoring for people with dementia in care homes: the feasibility and clinical impact of nurse-led monitoring. Sci World J. 2014;2014:843621.
Ghibelli S, Marengoni A, Djade CD, Nobili A, Tettamanti M, Franchi C, et al. Prevention of inappropriate prescribing in hospitalized older patients using a computerized prescription support system (INTERcheck®). Drugs Aging. 2013;30(10):821–8.
Lang PO, Vogt-Ferrier N, Hasso Y, Le Saint L, Dramé M, Zekry D, et al. Interdisciplinary geriatric and psychiatric care reduces potentially inappropriate prescribing in the hospital: interventional study in 150 acutely ill elderly patients with mental and somatic comorbid conditions. J Am Med Dir Assoc. 2012;13(4):406.e1–7.
Garfinkel D, Mangin D. Feasibility study of a systematic approach for discontinuation of multiple medications in older adults: addressing polypharmacy. Arch Intern Med. 2010;170(18):1648–54.
Halvorsen KH, Ruths S, Granas AG, Viktil KK. Multidisciplinary intervention to identify and resolve drug-related problems in Norwegian nursing homes. Scand J Prim Health Care. 2010;28(2):82–8.
Poudel A, Peel NM, Mitchell CA, Gray LC, Nissen LM, Hubbard RE. Geriatrician interventions on medication prescribing for frail older people in residential aged care facilities. Clin Interv Aging. 2015;10:1043.
Brunet NM, Sevilla-Sánchez D, Novellas JA, Jané CC, Gómez-Batiste X, McIntosh J, et al. Optimizing drug therapy in patients with advanced dementia: a patient-centered approach. Eur Geriatr Med. 2014;5(1):66–71.
Saad M, Harisingani R, Katinas L. Impact of geriatric consultation on the number of medications in hospitalized older patients. Consult Pharm. 2012;27(1):42–8.
Chan VT, Woo BK, Sewell DD, Allen EC, Golshan S, Rice V, et al. Reduction of suboptimal prescribing and clinical outcome for dementia patients in a senior behavioral health inpatient unit. Int Psychogeriatr. 2009;21(1):195–9.
Gustafsson M, Sjolander M, Pfister B, Schneede J, Lovheim H. Effects of pharmacists’ interventions on inappropriate drug use and drug-related readmissions in people with dementia: a secondary analysis of a randomized controlled trial. Pharmacy (Basel). 2018;6(1):E7.
Pfister B, Jonsson J, Gustafsson M. Drug-related problems and medication reviews among old people with dementia. BMC Pharmacol Toxicol. 2017;18(1):52–62.
Grimes DA, Schulz KF. An overview of clinical research: the lay of the land. Lancet. 2002;359(9300):57–61.
Reeve E, Farrell B, Thompson W, Herrmann N, Sketris I, Magin P, et al. Evidence-based clinical practice guideline for deprescribing cholinesterase inhibitors and memantine. Sydney: The University of Sydney; 2018.
Millar AN, Daffu-O’Reilly A, Hughes CM, Alldred DP, Barton G, Bond CM, et al. Development of a core outcome set for effectiveness trials aimed at optimising prescribing in older adults in care homes. Trials. 2017;18(1):175.
Acknowledgements
The authors would like to thank Ms. Christine Dalais (The University of Queensland Library) for her help with the development of the search strategy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Leila Shafiee Hanjani, Duncan Long, Nancye M. Peel, Geeske Peeters, Christopher R. Freeman and Ruth E. Hubbard declare that they have no conflicts of interest.
Funding
Leila Shafiee Hanjani is supported by an Australian Government Research Training Program (RTP), and Geeske Peeters is supported by a fellowship from the Global Brain Health Institute. This work was supported by the National Health and Medical Research Council (NHMRC) Partnership Centre for Dealing with Cognitive and Related Functional Decline in Older People (Grant no. GNT9100000). No other sources of funding were used to assist in the preparation of this article.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shafiee Hanjani, L., Long, D., Peel, N.M. et al. Interventions to Optimise Prescribing in Older People with Dementia: A Systematic Review. Drugs Aging 36, 247–267 (2019). https://doi.org/10.1007/s40266-018-0620-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0620-9