Abstract
Background
Residents of long-term care facilities (LTCFs) are at high risk of hospitalization. Medications are a potentially modifiable risk factor for hospitalizations.
Objective
Our objective was to systematically review the association between medications or prescribing patterns and hospitalizations from LTCFs.
Methods
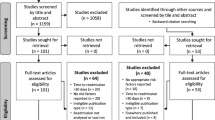
We searched MEDLINE, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and International Pharmaceutical Abstracts (IPA) from inception to August 2017 for longitudinal studies reporting associations between medications or prescribing patterns and hospitalizations. Two independent investigators completed the study selection, data extraction and quality assessment using the Joanna Briggs Institute Critical Appraisal Tools.
Results
Three randomized controlled trials (RCTs), 22 cohort studies, five case–control studies, one case-time-control study and one case-crossover study, investigating 13 different medication classes and two prescribing patterns were included. An RCT demonstrated that high-dose influenza vaccination reduced all-cause hospitalization compared with standard-dose vaccination (risk ratio [RR] 0.93; 95% confidence interval [CI] 0.88–0.98). Another RCT found no difference in hospitalization rates between oseltamivir as influenza treatment and oseltamivir as treatment plus prophylaxis (treatment = 4.7%, treatment and prophylaxis = 3.5%; p = 0.7). The third RCT found no difference between multivitamin/mineral supplementation and hospitalization (odds ratio [OR] 0.94; 95% CI 0.74–1.20) or emergency department visits (OR 1.05; 95% CI 0.76–1.47). Two cohort studies demonstrated influenza vaccination reduced hospitalization. Four studies suggested polypharmacy and potentially inappropriate medications (PIMs) increased all-cause hospitalization. However, associations between polypharmacy (two studies), PIMs (one study) and fall-related hospitalizations were inconsistent. Inconsistent associations were found between psychotropic medications with all-cause and cause-specific hospitalizations (11 studies). Warfarin, nonsteroidal anti-inflammatory drugs, pantoprazole and vinpocetine but not long-term acetylsalicylic acid (aspirin), statins, trimetazidine, digoxin or β-blockers were associated with all-cause or cause-specific hospitalizations in single studies of specific resident populations. Most cohort studies assessed prevalent rather than incident medication exposure, and no studies considered time-varying medication use.
Conclusion
High-quality evidence suggests influenza vaccination reduces hospitalization. Polypharmacy and PIMs are consistently associated with increased all-cause hospitalization.

Similar content being viewed by others
References
Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev. 2007;65(1):3–39.
Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc. 2010;58(4):627–35.
Saliba D, Kington R, Buchanan J, Bell R, Wang M, Lee M, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48(2):154–63.
Hirsch CH, Sommers L, Olsen A, Mullen L, Winograd CH. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc. 1990;38(12):1296–303.
Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451–8.
Torio CM, Moore BJ. National inpatient hospital costs: the most expensive conditions by payer 2013. In: Statistical brief 204. Agency for Healthcare Research and Quality, Rockville. 2016. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp. Accessed 16 Sept 2017.
Castle NG, Mor V. Hospitalization of nursing home residents: a review of the literature, 1980–1995. Med Care Res Rev. 1996;53(2):123–48.
Graverholt B, Forsetlund L, Jamtvedt G. Reducing hospital admissions from nursing homes: a systematic review. BMC Health Serv Res. 2014;14:36.
Konetzka RT, Spector W, Limcangco MR. Reducing hospitalizations from long-term care settings. Med Care Res Rev. 2008;65(1):40–66.
Murray LM, Laditka SB. Care transitions by older adults from nursing homes to hospitals: implications for long-term care practice, geriatrics education, and research. J Am Med Dir Assoc. 2010;11(4):231–8.
Roughead EE, Semple SJ. Medication safety in acute care in Australia: where are we now? Part 1: a review of the extent and causes of medication problems 2002–2008. Aust N Z Health Policy. 2009;6(18). https://doi.org/10.1186/1743-8462-6-18.
Jokanovic N, Tan ECK, Dooley MJ, Kirkpatrick CM, Bell JS. Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc. 2015;16(6):535.
Nguyen JK, Fouts MM, Kotabe SE, Lo E. Polypharmacy as a risk factor for adverse drug reactions in geriatric nursing home residents. Am J Geriatr Pharmacother. 2006;4(1):36–41. https://doi.org/10.1016/j.amjopharm.2006.03.002.
Fleg JL, Aronow WS, Frishman WH. Cardiovascular drug therapy in the elderly: benefits and challenges. Nat Rev Cardiol. 2011;8(1):13–28.
Sanford AM, Orrell M, Tolson D, Abbatecola AM, Arai H, Bauer JM, et al. An international definition for nursing home. J Am Med Dir Assoc. 2015;16(3):181–4. https://doi.org/10.1016/j.jamda.2014.12.013.
Critical appraisal tools. Joanna Briggs Institute. 2016. http://joannabriggs.org/research/critical-appraisal-tools.html. Accessed 26 Sept 2017.
Chan TC, Luk JK, Shea YF, Lau KH, Chan FH, Yu GK, et al. Continuous use of antipsychotics and its association with mortality and hospitalization in institutionalized Chinese older adults: an 18-month prospective cohort study. Int Psychogeriatr. 2011;23(10):1640–8.
Cherubini A, Eusebi P, Dell’Aquila G, Landi F, Gasperini B, Bacuccoli R, et al. Predictors of hospitalization in Italian nursing home residents: the U.L.I.S.S.E. project. J Am Med Dir Assoc. 2012;13(1):84. https://doi.org/10.1016/j.jamda.2011.04.001.
Cooper JW, Freeman MH, Cook CL, Burfield AH. Psychotropic and psychoactive drugs and hospitalization rates in nursing facility residents. Pharm Pract (Granada). 2007;5(3):140–4.
Dedhiya SD, Hancock E, Craig BA, Doebbeling CC, Thomas J 3rd. Incident use and outcomes associated with potentially inappropriate medication use in older adults. Am J Geriatr Pharmacother. 2010;8(6):562–70.
Eaton CB, Lapane KL, Murphy JB, Hume AL. Effect of statin (HMG-Co-A-Reductase Inhibitor) use on 1-year mortality and hospitalization rates in older patients with cardiovascular disease living in nursing homes. J Am Geriatr Soc. 2002;50(8):1389–95.
Gorisek Miksic N, Ursic T, Simonovic Z, Lusa L, Lobnik Rojko P, Petrovec M, et al. Oseltamivir prophylaxis in controlling influenza outbreak in nursing homes: a comparison between three different approaches. Infection. 2015;43(1):73–81.
Jung HY, Meucci M, Unruh MA, Mor V, Dosa D. Antipsychotic use in nursing home residents admitted with hip fracture. J Am Geriatr Soc. 2013;61(1):101–6.
Lalic S, Sluggett JK, Ilomaki J, Wimmer B, Tan ECK, Robson L, et al. Polypharmacy and medication regimen complexity as risk factors for hospitalization among residents of long-term care facilities: a prospective cohort study. J Am Med Dir Assoc. 2016;17(11):1067.e1–6.
Lapane KL, Hume AL, Barbour MM, Lipsitz LA. Does aspirin attenuate the effect of angiotensin-converting enzyme inhibitors on health outcomes of very old patients with heart failure? J Am Geriatr Soc. 2002;50(7):1198–204.
Lapane KL, Spooner JJ, Mucha L, Straus WL. Effect of nonsteroidal anti-inflammatory drug use on the rate of gastrointestinal hospitalizations among people living in long-term care. J Am Geriatr Soc. 2001;49(5):577–84. https://doi.org/10.1046/j.1532-5415.2001.49117.x.
Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med. 2005;17(11):68–74. https://doi.org/10.1016/j.jamda.2016.08.019.
Leung AY, Kwan CW, Chi I. Residents with Alzheimer’s disease in long-term care facilities in Hong Kong: patterns of hospitalization and emergency room use. Aging Ment Health. 2013;17(8):959–65.
Patriarca PA, Weber JA, Parker RA. Efficacy of influenza vaccine in nursing homes. Reduction in illness and complications during an influenza A (H3N2) epidemic. J Am Med Assoc. 1985;253(8):1136–9.
Rochon PA, Normand SL, Gomes T, Gill SS, Anderson GM, Melo M, et al. Antipsychotic therapy and short-term serious events in older adults with dementia. Arch Intern Med. 2008;168(10):1090–6.
Ruggiero C, Dell’Aquila G, Gasperini B, Onder G, Grp US. Potentially inappropriate drug prescriptions and risk of hospitalization among older, Italian, nursing home residents: the ULISSE project. Drugs Aging. 2010;27(9):747–58.
Simoni-Wastila L, Ryder PT, Qian J, Zuckerman IH, Shaffer T, Zhao L. Association of antipsychotic use with hospital events and mortality among medicare beneficiaries residing in long-term care facilities. Am J Geriatr Psychiatry. 2009;17(5):417–27. https://doi.org/10.1097/JGP.0b013e31819b8936.
Deguchi Y, Nishimura K. Efficacy of influenza vaccine in elderly persons in welfare nursing homes: reduction in risks of mortality and morbidity during an influenza A (H3N2) epidemic. J Gerontol A Biol Sci Med Sci. 2001;56(6):391–4.
Steinman MA, Zullo AR, Lee Y, et al. Association of β-blockers with functional outcomes, death, and rehospitalization in older nursing home residents after acute myocardial infarction. JAMA Intern Med. 2017;177(2):254–62.
Liperoti R, Pedone C, Lapane KL, Mor V, Bernabei R, Gambassi G. Venous thromboembolism among elderly patients treated with atypical and conventional antipsychotic agents. Arch Intern Med. 2005;165(22):2677–82.
Lackner TE, Heard T, Glunz S, Gann N, Babington M, Malone DC. Gastrointestinal disease control after histamine-2-receptor antagonist dose modification for renal impairment in frail chronically Ill elderly patients. J Am Geriatr Soc. 2003;51(5):650–6.
Bor A, Matuz M, Csatordai M, Szalai G, Balint A, Benko R, et al. Medication use and risk of falls among nursing home residents: a retrospective cohort study. Int J Clin Pharm. 2017;39(2):408–15.
Sheriff HM, Thogaripally MR, Panjrath G, Arundel C, Zeng Q, Fonarow GC, et al. Digoxin and 30-day all-cause readmission in long-term care residents hospitalized for heart failure. J Am Med Dir Assoc. 2017;18(9):761–5. https://doi.org/10.1016/j.jamda.2017.03.016.
Quilliam BJ, Lapane KL, Eaton CB, Mor V. Effect of antiplatelet and anticoagulant agents on risk of hospitalization for bleeding among a population of elderly nursing home stroke survivors. Stroke. 2001;32(10):2299–304.
Liperoti R, Gambassi G, Lapane KL, Chiang C, Pedone C, Mor V, et al. Cerebrovascular events among elderly nursing home patients treated with conventional or atypical antipsychotics. J Clin Psychiatry. 2005;66(9):1090–6.
Liperoti R, Gambassi G, Lapane KL, Chiang C, Pedone C, Mor V, et al. Conventional and atypical antipsychotics and the risk of hospitalization for ventricular arrhythmias or cardiac arrest. Arch Intern Med. 2005;165(6):696–701.
Liperoti R, Onder G, Lapane KL, Mor V, Friedman JH, Bernabei R, et al. Conventional or atypical antipsychotics and the risk of femur fracture among elderly patients: results of a case-control study. J Clin Psychiatry. 2007;68(6):929–34.
Ryan-Atwood TE, Hutchinson-Kern M, Ilomaki J, Dooley MJ, Poole SG, Kirkpatrick CM, et al. Medication use and fall-related hospital admissions from long-term care facilities: a hospital-based case-control study. Drugs Aging. 2017;34(8):625–33.
Booy R, Lindley RI, Dwyer DE, Yin JK, Heron LG, Moffatt CR, et al. Treating and preventing influenza in aged care facilities: a cluster randomised controlled trial. PLoS One. 2012;7(10):e46509. https://doi.org/10.1371/journal.pone.0046509.
Liu BA, McGeer A, McArthur MA, Simor AE, Aghdassi E, Davis L, et al. Effect of multivitamin and mineral supplementation on episodes of infection in nursing home residents: a randomized, placebo-controlled study. J Am Geriatr Soc. 2007;55(1):35–42.
Gravenstein S, Davidson HE, Taljaard M, Ogarek J, Gozalo P, Han L, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccination on numbers of US nursing home residents admitted to hospital: a cluster-randomised trial. Lancet Respir Med. 2017;5(9):738–46.
Price SD, Holman CD, Sanfilippo FM, Emery JD. Are high-care nursing home residents at greater risk of unplanned hospital admission than other elderly patients when exposed to Beers potentially inappropriate medications? Geriatr Gerontol Int. 2014;14(4):934–41.
Berry SD, Lee Y, Cai S, Dore DD. Nonbenzodiazepine sleep medication use and hip fractures in nursing home residents. JAMA Intern Med. 2013;173(9):754–61. https://doi.org/10.1001/jamainternmed.2013.3795.
Lattanzio F, Mussi C, Scafato E, Ruggiero C, Dell’Aquila G, Pedone C, et al. Health care for older people in Italy: The U.L.I.S.S.E. project (Un Link Informatico sui Servizi Sanitari Esistenti per l’anziano—a computerized network on health care services for older people). J Nutr Health Aging. 2010;14(3):238–42.
Bernabei R, Gambassi G, Lapane K, Sgadari A, Landi F, Gatsonis C, et al. Characteristics of the SAGE database: a new resource for research on outcomes in long-term care. SAGE (Systematic Assessment of Geriatric drug use via Epidemiology) Study Group. J Gerontol A Biol Sci Med Sci. 1999;54(1):25–33.
Lund JL, Richardson DB, Sturmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep. 2015;2(4):221–8. https://doi.org/10.1007/s40471-015-0053-5.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20. https://doi.org/10.1093/aje/kwg231.
Divac N, Prostran M, Jakovcevski I, Cerovac N. Second-generation antipsychotics and extrapyramidal adverse effects. BioMed Res Int. 2014;2014:6. https://doi.org/10.1155/2014/656370.
Kleijer BC, van Marum RJ, Egberts AC, Jansen PA, Knol W, Heerdink ER. Risk of cerebrovascular events in elderly users of antipsychotics. J Psychopharmacol. 2009;23(8):909–14. https://doi.org/10.1177/0269881108093583.
Dose-response relationship. In: Pettygrove S, editor. Encyclopædia Britannica: Encyclopædia Britannica, inc.; 2016.
Dettori JR. Loss to follow-up. Evid Based Spine Care J. 2011;2(1):7–10. https://doi.org/10.1055/s-0030-1267080.
American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–31. https://doi.org/10.1111/j.1532-5415.2012.03923.x.
Levy HB, Marcus E-L, Christen C. Adverse reactions/medication safety: beyond the Beers criteria: a comparative overview of explicit criteria. Ann Pharmacother. 2010;44(12):1968–75. https://doi.org/10.1345/aph.1P426.
Steinman MA, Beizer JL, DuBeau CE, Laird RD, Lundebjerg NE, Mulhausen P. How to use the AGS 2015 Beers criteria—a guide for patients, clinicians, health systems, and payors. J Am Geriatr Soc. 2015;63(12):e1–7. https://doi.org/10.1111/jgs.13701.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening tool of older person’s prescriptions) and START (Screening tool to alert doctors to right treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83.
Grace AR, Briggs R, Kieran RE, Corcoran RM, Romero-Ortuno R, Coughlan TL, et al. A comparison of Beers and STOPP criteria in assessing potentially inappropriate medications in nursing home residents attending the emergency department. J Am Med Dir Assoc. 2014;15(11):830–4. https://doi.org/10.1016/j.jamda.2014.08.008.
van der Stelt CA, Windsant-van Vermeulen, den Tweel AM, Egberts AC, van den Bemt PM, Leendertse AJ, Hermens WA, et al. The association between potentially inappropriate prescribing and medication-related hospital admissions in older patients: a nested case control study. Drug Saf. 2016;39(1):79–87. https://doi.org/10.1007/s40264-015-0361-1.
Lee WJ, Chen LK, Tang GJ, Lan TY. The impact of influenza vaccination on hospitalizations and mortality among frail older people. J Am Med Dir Assoc. 2014;15(4):256–60. https://doi.org/10.1016/j.jamda.2013.12.003.
Nichol KL, Margolis KL, Wouremna J, von Sternberg T. Effectiveness of influenza vaccine in the elderly. Gerontology. 1996;42(5):274–9.
Chan TC, Hung IF, Luk JK, Shea YF, Chan FH, Woo PC, et al. Prevention of mortality and pneumonia among nursing home older adults by dual pneumococcal and seasonal influenza vaccination during a pandemic caused by novel pandemic influenza A (H1N1). J Am Med Dir Assoc. 2012;13(8):698–703. https://doi.org/10.1016/j.jamda.2012.05.009.
Chan TC, Fan-Ngai Hung I, Ka-Hay Luk J, Chu LW, Hon-Wai Chan F. Effectiveness of influenza vaccination in institutionalized older adults: a systematic review. J Am Med Dir Assoc. 2014;15(3):226.e1-6. https://doi.org/10.1016/j.jamda.2013.10.008.
Welliver R, Monto AS, Carewicz O, Schatteman E, Hassman M, Hedrick J, et al. Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. JAMA. 2001;285(6):748–54.
van der Sande MA, Meijer A, Şen-Kerpiclik F, Enserink R, Cools HJ, Overduin P, et al. Effectiveness of post-exposition prophylaxis with oseltamivir in nursing homes: a randomised controlled trial over four seasons. Emerg Themes Epidemiol. 2014;11(1):13. https://doi.org/10.1186/1742-7622-11-13.
Jefferson T, Jones M, Doshi P, Spencer EA, Onakpoya I, Heneghan CJ. Oseltamivir for influenza in adults and children: systematic review of clinical study reports and summary of regulatory comments. BMJ. 2014;348(g2545). https://doi.org/10.1136/bmj.g2545.
Pengo V, Legnani C, Noventa F, Palareti G. Oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and risk of bleeding. A multicenter inception cohort study. Thromb Haemost. 2001;85(3):418–22.
Bleeding during antithrombotic therapy in patients with atrial fibrillation. The stroke prevention in atrial fibrillation investigators. Arch Intern Med. 1996;156(4):409–16.
Jhund P, McMurray JJV. Does aspirin reduce the benefit of an angiotensin-converting enzyme inhibitor? Circulation. 2006;113(22):2566.
Leor J, Reicher-Reiss H, Goldbourt U, Boyko V, Gottlieb S, Battler A, et al. Aspirin and mortality in patients treated with angiotensin-converting enzyme inhibitors: a cohort study of 11,575 patients with coronary artery disease. J Am Coll Cardiol. 1999;33(7):1920–5. https://doi.org/10.1016/S0735-1097(99)00129-1.
Ittaman SV, VanWormer JJ, Rezkalla SH. The role of aspirin in the prevention of cardiovascular disease. Clin Med Res. 2014;12(3–4):147–54. https://doi.org/10.3121/cmr.2013.1197.
Ahmed A. Digoxin and reduction in mortality and hospitalization in geriatric heart failure: importance of low doses and low serum concentrations. J Gerontol A Biol Sci Med Sci. 2007;62(3):323–9.
Scott D, Blizzard L, Fell J, Jones G. Statin therapy, muscle function and falls risk in community-dwelling older adults. QJM. 2009;102(9):625–33. https://doi.org/10.1093/qjmed/hcp093.
Pedro-Botet J, Climent E, Chillarón JJ, Toro R, Benaiges D, Flores-Le Roux JA. Statins for primary cardiovascular prevention in the elderly. J Geriatr Cardiol. 2015;12(4):431–8. https://doi.org/10.11909/j.issn.1671-5411.2015.04.016.
Zhou X, Chen J. Is treatment with trimetazidine beneficial in patients with chronic heart failure? PLoS One. 2014;9(5):e94660. https://doi.org/10.1371/journal.pone.0094660.
Di Napoli P, Di Giovanni P, Gaeta MA, Taccardi AA, Barsotti A. Trimetazidine and reduction in mortality and hospitalization in patients with ischemic dilated cardiomyopathy: a post hoc analysis of the Villa Pini d’Abruzzo Trimetazidine Trial. J Cardiovasc Pharmacol. 2007;50(5):585–9. https://doi.org/10.1097/FJC.0b013e31814fa9cb.
Chen Y, Liu B, Glass K, Du W, Banks E, Kirk M. Use of proton pump inhibitors and the risk of hospitalization for infectious gastroenteritis. PLoS One. 2016;11(12):e0168618. https://doi.org/10.1371/journal.pone.0168618.
Lewis JR, Barre D, Zhu K, Ivey KL, Lim EM, Hughes J, et al. Long-term proton pump inhibitor therapy and falls and fractures in elderly women: a prospective cohort study. J Bone Miner Res. 2014;29(11):2489–97. https://doi.org/10.1002/jbmr.2279.
Pello Lázaro AM, Cristóbal C, Franco-Peláez JA, Tarín N, Aceña Á, Carda R, et al. Use of proton-pump inhibitors predicts heart failure and death in patients with coronary artery disease. PLoS One. 2017;12(1):e0169826. https://doi.org/10.1371/journal.pone.0169826.
Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs: a meta-analysis. Ann Intern Med. 1991;115(10):787–96. https://doi.org/10.7326/0003-4819-115-10-787.
Peng S, Duggan A. Gastrointestinal adverse effects of non-steroidal anti-inflammatory drugs. Expert Opin Drug Saf. 2005;4(2):157–69. https://doi.org/10.1517/14740338.4.2.157.
Yachimski PS, Friedman LS. Gastrointestinal bleeding in the elderly. Nat Clin Pract Gastroenterol Hepatol. 2008;5(2):80–93.
Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2010;(1):CD005465. https://doi.org/10.1002/14651858.cd005465.pub2.
Marcum ZA, Perera S, Thorpe JM, Switzer GE, Gray SL, Castle NG, et al. Anticholinergic use and recurrent falls in community-dwelling older adults: findings from the health ABC study. Ann Pharmacother. 2015;49(11):1214–21. https://doi.org/10.1177/1060028015596998.
Toot S, Devine M, Akporobaro A, Orrell M. Causes of hospital admission for people with dementia: a systematic review and meta-analysis. J Am Med Dir Assoc. 2013;14(7):463–70. https://doi.org/10.1016/j.jamda.2013.01.011.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Kate Wang is supported by an Australian Government Research Training Program Scholarship. Esa Chen is supported by the National Health and Medical Research Council (NHMRC) Cognitive Decline Partnership Centre and the Faculty of Pharmacy and Pharmaceutical Sciences, Monash University. Julia Gilmartin-Thomas is an NHMRC-ARC Dementia Research Development Fellow. Jenni Ilomäki is funded through the NHMRC Early Career Fellowship. No other sources of funding were used to assist in the preparation of this review.
Conflict of interest
Kate Wang, J. Simon Bell, Esa Chen, Julia Gilmartin-Thomas and Jenni Ilomäki have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, K.N., Bell, J.S., Chen, E.Y.H. et al. Medications and Prescribing Patterns as Factors Associated with Hospitalizations from Long-Term Care Facilities: A Systematic Review. Drugs Aging 35, 423–457 (2018). https://doi.org/10.1007/s40266-018-0537-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0537-3