Abstract
Background
Medicines are potentially modifiable risk factors for postoperative delirium. However, the extent to which preoperative medicines are included in risk prediction models (RPMs) is unknown.
Objective
This systematic review aimed to assess the extent of inclusion of preoperative medications in RPMs for postoperative delirium.
Methods
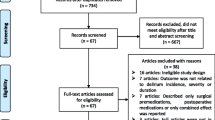
Articles were systematically searched from MEDLINE, EMBASE and CINAHL using Medical Subject Headings (MeSH) where possible and keywords for postoperative delirium and prediction model. Studies published until May 2017 with a primary outcome of postoperative delirium that developed an RPM containing preoperative patient information were considered. Where a study had two cohorts, a derivation and a validation cohort, findings from the derivation cohort were extracted and reported.
Results
Eighteen prospective and one retrospective cohort studies were included for review. Of the 19 studies, only nine considered preoperative medication data, with medications appearing as predictor variables in five models. There was wide variability in the factors included in the final models, with the most frequent predictors being age and cognitive impairment, appearing in 13 (68%) and 11 (58%) RPMs, respectively.
Conclusion
While medications are commonly cited risk factors for delirium, they are not adequately considered when developing RPMs. Future studies aiming to develop an RPM for postoperative delirium should include preoperative medication data as a potential predictor variable because of the modifiable nature of medication use and its impact on other factors commonly in models, such as cognition.

Similar content being viewed by others
References
Jackson MB, Mookherjee S, Hamlin NP. The perioperative medicine consult handbook. New York: Springer; 2015.
Mu JL, Lee A, Joynt GM. Pharmacologic agents for the prevention and treatment of delirium in patients undergoing cardiac surgery: systematic review and metaanalysis. Crit Care Med. 2015;43(1):194–204. https://doi.org/10.1097/ccm.0000000000000673.
Rudolph JL, Jones RN, Levkoff SE, Rockett C, Inouye SK, Sellke FW, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119(2):229–36. https://doi.org/10.1161/circulationaha.108.795260.
Katznelson R, Djaiani GN, Borger MA, Friedman Z, Abbey SE, Fedorko L, et al. Preoperative use of statins is associated with reduced early delirium rates after cardiac surgery. Anesthesiology. 2009;110(1):67–73.
Marcantonio E, Ta T, Duthie E, Resnick NM. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. J Am Geriatr Soc. 2002;50(5):850–7.
Tropea J, Slee J, Holmes A, Gorelik A, Brand C. Use of antipsychotic medications for the management of delirium: an audit of current practice in the acute care setting. Int Psychogeriatr. 2009;21(01):172–9.
Mangusan RF, Hooper V, Denslow SA, Travis L. Outcomes associated with postoperative delirium after cardiac surgery. Am J Crit Care. 2015;24(2):156–63. https://doi.org/10.4037/ajcc2015137.
Pauley E, Lishmanov A, Schumann S, Gala GJ, van Diepen S, Katz JN. Delirium is a robust predictor of morbidity and mortality among critically ill patients treated in the cardiac intensive care unit. Am Heart J. 2015;170(1):79.e1–86.e1. https://doi.org/10.1016/j.ahj.2015.04.013.
Hshieh TT, Yue J, Oh E, Puelle M, Dowal S, Travison T, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512–20. https://doi.org/10.1001/jamainternmed.2014.7779.
Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–22.
Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, Cooney LM Jr. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–76.
Benoit AG, Campbell BI, Tanner JR, Staley JD, Wallbridge HR, Biehl DR, et al. Risk factors and prevalence of perioperative cognitive dysfunction in abdominal aneurysm patients. J Vasc Surg. 2005;42(5):884–90. https://doi.org/10.1016/j.jvs.2005.07.032.
Tully PJ, Baker RA, Winefield HR, Turnbull DA. Depression, anxiety disorders and type D personality as risk factors for delirium after cardiac surgery. Aust N Z J Psychiatry. 2010;44(11):1005–11. https://doi.org/10.3109/00048674.2010.495053.
Chen YL, Lin HC, Lin KH, Lin LS, Hsieh CE, Ko CJ, et al. Low hemoglobin level is associated with the development of delirium after hepatectomy for hepatocellular carcinoma patients. PLoS One. 2015;10(3):e0119199. https://doi.org/10.1371/journal.pone.0119199.
Katznelson R, Djaiani G, Mitsakakis N, Lindsay TF, Tait G, Friedman Z, et al. Delirium following vascular surgery: increased incidence with preoperative β-blocker administration. Can J Anaesth. 2009;56(11):793–801.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Association; 2013.
Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 7 July 2017.
Choi NY, Kim EH, Baek CH, Sohn I, Yeon S, Chung MK. Development of a nomogram for predicting the probability of postoperative delirium in patients undergoing free flap reconstruction for head and neck cancer. Eur J Surg Oncol. 2017;43(4):683–8. https://doi.org/10.1016/j.ejso.2016.09.018.
Jeong YM, Lee E, Kim KI, Chung JE, In Park H, Lee BK, et al. Association of pre-operative medication use with post-operative delirium in surgical oncology patients receiving comprehensive geriatric assessment. BMC Geriatr. 2016;16:134. https://doi.org/10.1186/s12877-016-0311-5.
Visser L, Prent A, Van Der Laan MJ, Van Leeuwen BL, Izaks GJ, Zeebregts CJ, et al. Predicting postoperative delirium after vascular surgical procedures. J Vasc Surg. 2015;62(1):185–9. https://doi.org/10.1016/j.jvs.2015.01.041.
Bohner H, Hummel TC, Habel U, Miller C, Reinbott S, Yang Q, et al. Predicting delirium after vascular surgery: a model based on pre- and intraoperative data. Ann Surg. 2003;238(1):149–56. https://doi.org/10.1097/00000658-200307000-00019.
Bakker RC, Osse RJ, Tulen JH, Kappetein AP, Bogers AJ. Preoperative and operative predictors of delirium after cardiac surgery in elderly patients. Eur J Cardiothorac Surg. 2012;41(3):544–9. https://doi.org/10.1093/ejcts/ezr031.
Van Der Mast RC, Van Den Broek WW, Fekkes D, Pepplinkhuizen L, Habbema JDF. Incidence of and preoperative predictors for delirium after cardiac surgery. J Psychosom Res. 1999;46(5):479–83. https://doi.org/10.1016/S0022-3999%2899%2900002-1.
Guenther U, Theuerkauf N, Frommann I, Brimmers K, Malik R, Stori S, et al. Predisposing and precipitating factors of delirium after cardiac surgery: a prospective observational cohort study. Ann Surg. 2013;257(6):1160–7. https://doi.org/10.1097/SLA.0b013e318281b01c.
Krzych LJ, Wybraniec MT, Krupka-Matuszczyk I, Skrzypek M, Bochenek AA. Delirium Screening in Cardiac Surgery (DESCARD): a useful tool for nonpsychiatrists. Can J Cardiol. 2014;30(8):932–9. https://doi.org/10.1016/j.cjca.2014.04.020.
Koster S, Hensens AG, Schuurmans MJ, van der Palen J. Prediction of delirium after cardiac surgery and the use of a risk checklist. Eur J Cardiovasc Nurs. 2013;12(3):284–92. https://doi.org/10.1177/1474515112450244.
Koster S, Oosterveld FG, Hensens AG, Wijma A, van der Palen J. Delirium after cardiac surgery and predictive validity of a risk checklist. Ann Thorac Surg. 2008;86(6):1883–7. https://doi.org/10.1016/j.athoracsur.2008.08.020.
Harasawa N, Mizuno T. A novel scale predicting postoperative delirium (POD) in patients undergoing cerebrovascular surgery. Arch Gerontol Geriatr. 2014;59(2):264–71. https://doi.org/10.1016/j.archger.2014.05.007.
Goldenberg G, Kiselev P, Bharathan T, Baccash E, Gill L, Madhav V, et al. Predicting post-operative delirium in elderly patients undergoing surgery for hip fracture. Psychogeriatrics. 2006;6(2):43–8. https://doi.org/10.1111/j.1479-8301.2006.00146.x.
Liang CK, Chu CL, Chou MY, Lin YT, Lu T, Hsu CJ, et al. Developing a prediction model for post-operative delirium and long-term outcomes among older patients receiving elective orthopedic surgery: a prospective cohort study in taiwan. Rejuvenation Res. 2015;18(4):347–55. https://doi.org/10.1089/rej.2014.1645.
Litaker D, Locala J, Franco K, Bronson DL, Tannous Z. Preoperative risk factors for postoperative delirium. Gen Hosp Psychiatry. 2001;23(2):84–9. https://doi.org/10.1016/S0163-8343%2801%2900117-7.
Dworkin A, Lee DSH, An AR, Goodlin SJ. A simple tool to predict development of delirium after elective surgery. J Am Geriatr Soc. 2016;64(11):e149–53. https://doi.org/10.1111/jgs.14428.
Kim MY, Park UJ, Kim HT, Cho WH. DELirium prediction based on hospital information (Delphi) in general surgery patients. Medicine (Baltimore). 2016;95(12):e3072. https://doi.org/10.1097/MD.0000000000003072.
Marcantonio ER, Goldman L, Mangione CM, Ludwig LE, Muraca B, Haslauer CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271(2):134–9.
Clinical Epidemiology and Health Service Evaluation Unit. Clinical practice guidelines for the management of delirium in older people. Melbourne: Clinical Epidemiology and Health Service Evaluation Unit; 2006. p. 42.
Duppils GS, Wikblad K. Acute confusional states in patients undergoing hip surgery. Gerontology. 2000;46(1):36–43.
Dai YT, Lou MF, Yip PK, Huang GS. Risk factors and incidence of postoperative delirium in elderly Chinese patients. Gerontology. 2000;46(1):28–35.
Ali S, Patel M, Jabeen S, Bailey RK, Patel T, Shahid M, et al. Insight into delirium. Innov Clin Neurosci. 2011;8(10):25.
Alagiakrishnan K, Wiens CA. An approach to drug induced delirium in the elderly. Postgrad Med J. 2004;80(945):388–93.
Dimsdale JE, Newton RP. Neuropsychological side effects of β-blockers. Arch Intern Med. 1989;149(3):514–25.
O’Neal JB, Liu X, Shotwell MS, Liang Y, Shaw A, Shah A, et al. Impact of preoperative statin or beta blocker use and delirium following cardiac surgery. Anesth Analg. 2016;122:S57. https://doi.org/10.1213/01.ane.0000499505.96779.a0.
Kassie GM, Nguyen TA, Ellett LMK, Pratt NL, Roughead EE. Preoperative medication use and postoperative delirium: a systematic review. BMC Geriatr. 2017;17(1):298.
Kassie GM, Ellett LMK, Nguyen TA, Roughead EE. Current practice and opinions of hospital pharmacists regarding their role in the screening, prevention and treatment of delirium. Int J Clin Pharm. 2017;39(6):1194–200.
Acknowledgements
We thank the health librarians of the University of South Australia who assisted us in searching the literature.
Funding
GMK is supported by an Australian Government Research Training Program Scholarship. LMKE and TAN are both supported by National Health and Medical Research Council (NHMRC)–Australian Research Council (ARC) Dementia Research Development Fellowships (LMKE grant identification number APP1101788, TAN grant identification number APP1103860). EER is supported by an NHMRC Senior Principal Research Fellowship (grant identification number APP1110139). The contents of the published material are solely the responsibility of the individual authors and do not reflect the views of NHMRC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gizat M. Kassie, Tuan A. Nguyen, Lisa M. Kalisch Ellett, Nicole L. Pratt and Elizabeth E. Roughead declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kassie, G.M., Nguyen, T.A., Kalisch Ellett, L.M. et al. Do Risk Prediction Models for Postoperative Delirium Consider Patients’ Preoperative Medication Use?. Drugs Aging 35, 213–222 (2018). https://doi.org/10.1007/s40266-018-0526-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0526-6