Abstract
Purpose
The aim of this study was to analyse the prevalence and predictors of drug combinations increasing bleeding risk among warfarin users with and without Alzheimer’s disease (AD).
Methods
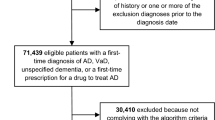
This retrospective observational study utilised data from the Finnish MEDALZ-2005 cohort. The MEDALZ-2005 study included all community-dwelling persons with a clinically verified diagnosis of AD at the end of 2005, and one comparison person without AD for each case. Data on drug use was collected from the Prescription Register. We included persons who were warfarin users during the study period 2006–2009. Drug combinations increasing bleeding risk with warfarin included selective serotonin reuptake inhibitors (SSRIs), non-steroidal anti-inflammatory agents (NSAIDs), other antithrombotic drugs and tramadol. Factors associated with combination use were investigated with logistic regression.
Results
During the follow-up, 3385 persons with AD and 4830 persons without AD used warfarin. Drug combinations increasing bleeding risk were more common in warfarin users with AD than without AD [35.9 and 30.5 %, respectively (p < 0.0001)]. The most common combination was SSRIs and warfarin, which was more common among persons with AD (23.8 %) than among persons without AD (10.9 %). NSAIDs and warfarin combination was more common among persons without AD. Combination use was associated with AD, female gender, younger age, diabetes mellitus, rheumatoid arthritis and asthma/chronic obstructive pulmonary disease (COPD).
Conclusions
Use of drug combinations increasing bleeding risk was more common among warfarin users with AD. Special attention should be paid to minimise the duration of concomitant use and to find safer alternatives without increased bleeding risk.

Similar content being viewed by others
References
Horton JD, Bushwick BM. Warfarin therapy: evolving strategies in anticoagulation. Am Fam Physician. 1999;59:635–46.
Bauersachs RM. Use of anticoagulants in elderly patients. Thromb Res. 2012;129:107–15.
Sinauridze EI, Panteleev MA, Ataullakhanov FI. Anticoagulant therapy: basic principles, classic approaches and recent developments. Blood Coagul Fibrinolysis. 2012;23:482–93.
Finnish Medical Society Duodecim. Current care: atrial fibrillation. 2014. http://www.kaypahoito.fi/. Accessed 1 Oct 2015.
Wadelius M, Pirmohamed M. Pharmacogenetics of warfarin: current status and future challenges. Pharmacogenomics J. 2007;7:99–111.
Sellers MB, Newby LK. Atrial fibrillation, anticoagulation, fall risk, and outcomes in elderly patients. Am Heart J. 2011;161:241–6.
Gasse C, Hollowell J, Meier CR, Haefeli WE. Drug interactions and risk of acute bleeding leading to hospitalisation or death in patients with chronic atrial fibrillation treated with warfarin. Thromb Haemost. 2005;94:537–43.
Donzé J, Clair C, Hug B, Rodondi N, Waeber G, Cornuz J, et al. Risk of falls and major bleeds in patients on oral anticoagulation therapy. Am J Med. 2012;125:773–8.
Van Doorn C, Gruber-Baldini AL, Zimmerman S, Hebel RJ, Port CL, Baumgarten M, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. J Am Geriatr Soc. 2003;51:1213–8.
Douglas A, Letts L, Richardson J. A systematic review of accidental injury from fire, wandering and medication self-administration errors for older adults with and without dementia. Arch Gerontol Geriatr. 2011;52:e1–10.
Tolppanen A-M, Taipale H, Koponen M, Lavikainen P, Tanskanen A, Tiihonen J, et al. Use of existing data sources in clinical epidemiology: Finnish health care registers in Alzheimer’s disease research—the Medication use among persons with Alzheimer’s disease (MEDALZ-2005) study. Clin Epidemiol. 2013;5:277–85.
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS–ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–44.
WHO Collaborating Centre for Drug Statistics Methodology. The anatomical therapeutic chemical classification system. 2014. http://www.whocc.no/atc_ddd_index/. Accessed 1 Oct 2015.
Taipale H, Tanskanen A, Koponen M, Tolppanen A-M, Tiihonen J, Hartikainen S. Antidementia drug use among community-dwelling individuals with Alzheimer’s disease in Finland: a nationwide register-based study. Int Clin Psychopharmacol. 2014;29:216–23.
Taipale H, Koponen M, Tanskanen A, Tolppanen A-M, Tiihonen J, Hartikainen S. Antipsychotic doses among community-dwelling persons with Alzheimer disease in Finland. J Clin Psychopharmacol. 2014;34:435–40.
Taipale H, Koponen M, Tanskanen A, Tolppanen A-M, Tiihonen J, Hartikainen S. Antipsychotic polypharmacy among a nationwide sample of community-dwelling persons with Alzheimer’s disease. J Alzheimers Dis. 2014;41:1223–8.
Torvinen-Kiiskinen S, Taipale H, Tanskanen A, Tiihonen J, Hartikainen S. Concomitant use of acetylcholine esterase inhibitors and urinary antispasmodics among Finnish community-dwelling persons with Alzheimer disease. J Clin Psychopharmacol. 2014;34:1–6.
Böttiger Y, Laine K, Andersson ML, Korhonen T, Molin B, Ovesjö M-L, et al. SFINX-a drug–drug interaction database designed for clinical decision support systems. Eur J Clin Pharmacol. 2009;65:627–33.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Howard PA, Ellerbeck EF, Engelman KK, Patternson KL. The nature and frequency of potential warfarin drug interactions that increase the risk of bleeding in patients with atrial fibrillation. Pharmacoepidemiol Drug Saf. 2002;11:569–76.
Hauta-Aho M, Tirkkonen T, Vahlberg T, Laine K. The effect of drug interactions on bleeding risk associated with warfarin therapy in hospitalized patients. Ann Med. 2009;41:619–28.
Kotirum S, Chaiyakunapruk N, Jampachaisri K, Wattanasombat S, Rojnuckarin P. Utilization review of concomitant use of potentially interacting drugs in Thai patients using warfarin therapy. Pharmacoepidemiol Drug Saf. 2007;16:216–22.
Wittkowsky AK, Boccuzzi SJ, Wogen J, Wygant G, Patel P, Hauch O. Frequency of concurrent use of warfarin with potentially interacting drugs. Pharmacotherapy. 2004;24:1668–74.
Martinez C, Jones RW, Rietbrock S. Trends in the prevalence of antipsychotic drug use among patients with Alzheimer’s disease and other dementias including those treated with antidementia drugs in the community in the UK: a cohort study. BMJ Open. 2013. doi:10.1136/bmjopen-2012-002080.
Kessing LV, Harhoff M, Andersen PK. Treatment with antidepressants in patients with dementia-a nationwide register-based study. Int Psychogeriatr. 2007;19:902–13.
Guthrie B, Clark SA, McCowan C. The burden of psychotropic drug prescribingin people with dementia: a populationdatabase study. Age Ageing. 2010;39:637–42.
Finnish Medical Society Duodecim, 2010. Current care: memory disorders. http://www.kaypahoito.fi/. Accessed 1 Oct 2015.
Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293:596–608.
Hallas J, Dall M, Andries A, Andersen BS, Aalykke C, Hansen JM, et al. Use of single and combined antithrombotic therapy and risk of serious upper gastrointestinal bleeding: population based case-control study. BMJ. 2006;333:726.
Lip G, Windecker S, Huber K, Kirchhof P, Marin F, Ten Berg J, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the European Society of Cardiology Working Group. Eur Heart J. 2014;35:3155–79.
Roughead EE, Kalisch LM, Barratt JD, Gilbert AL. Prevalence of potentially hazardous drug interactions amongst Australian veterans. Br J Clin Pharmacol. 2010;70:252–7.
Vitry AI, Roughead EE, Ramsay EN, Preiss AK, Ryan P, Gilbert AL, et al. Major bleeding risk associated with warfarin and co-medications in the elderly population. Pharmacoepidemiol Drug Saf. 2011;20:1057–63.
Schalekamp T, Klungel OH, Souverein PC, de Boer A. Effect of oral antiplatelet agents on major bleeding in users of coumarins. Thromb Haemost. 2008;100:1076–83.
Sørensen R, Hansen ML, Abildstrom SZ, Hvelplund A, Andersson C, Jørgensen C, et al. Risk of bleeding in patients with acute myocardial infarction treated with different combinations of aspirin, clopidogrel, and vitamin K antagonists in Denmark: a retrospective analysis of nationwide registry data. Lancet. 2009;374:1967–74.
Battistella M, Mamdami MM, Juurlink DN, Rabeneck L, Laupacis A. Risk of upper gastrointestinal hemorrhage in warfarin users treated with nonselective NSAIDs or COX-2 inhibitors. Arch Intern Med. 2005;165:189–92.
Penning-van Beest F, Erkens J, Petersen K-U, Koelz HR, Herings R. Main comedications associated with major bleeding during anticoagulant therapy with coumarins. Eur J Clin Pharmacol. 2005;61:439–44.
Pottegård A, Meegaard PM, Holck LHV, dePont Christensen Rd, Madsen H, Hallas J. Concurrent use of tramadol and oral vitamin K antagonists and the risk of excessive anticoagulation: a register-based nested case-control study. Eur J Clin Pharmacol 2013;69:641–6.
Brouquet A, Cudennec T, Benoist S, Moulias S, Beauchet A, Penna C, et al. Impaired mobility, ASA status and administration of tramadol are risk factors for postoperative delirium in patients aged 75 years or more after major abdominal surgery. Ann Surg. 2010;251:759–65.
Hughes GJ, Patel PN, Saxena N. Effect of acetaminophen on international normalized ratio in patients receiving warfarin therapy. Pharmacotherapy. 2011;31:591–7.
Agarwal S, Bennett D, Smith DJ. Predictors of warfarin use in atrial fibrillation patients in the inpatient setting. Am J Cardiovasc Drugs. 2010;10:37–48.
Gurwitz JH, Monette J, Rochon PA, Eckler MA, Avorn J. Atrial fibrillation and stroke prevention with warfarin in the long-term care setting. Arch Intern Med. 1997;157:978–84. doi:10.1001/archinte.1997.00440300080006.
Quilliam BJ, Lapane KL, Leibson C. Clinical correlates and drug treatment of residents with stroke in long-term care editorial comment. Stroke. 2001;32:1385–93.
Wilke T, Groth A, Pfannkuche M, Harks O, Fuchs A, Maywald U, et al. Real life anticoagulation treatment of patients with atrial fibrillation in Germany: extent and causes of anticoagulant under-use. J Thromb Thrombolysis. 2015;40(1):97–107.
Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. BMJ Br Med J. 1993;307:846–8.
Haukka J, Suvisaari J, Tuulio-Henriksson A, Lönnqvist J. High concordance between self-reported medication and official prescription database information. Eur J Clin Pharmacol. 2007;63:1069–74.
Rikala M, Hartikainen S, Sulkava R, Korhonen MJ. Validity of the Finnish prescription register for measuring psychotropic drug exposures among elderly Finns: a population-based intervention study. Drugs Aging. 2010;27:337–49.
Acknowledgments
The authors thank the maintainers of Finnish healthcare registers for enabling this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None to declare.
Conflicts of interest
JT has served as a consultant to Lundbeck, Organon, Janssen-Cilag, Eli Lilly, AstraZeneca, F. Hoffman-La Roche and Bristol-Myers Squibb. He has received fees for giving expert opinions to Bristol-Myers Squibb and GlaxoSmithKline, lecture fees from Janssen-Cilag, Bristol-Myers Squibb, Eli Lilly, Pfizer, Lundbeck, GlaxoSmithKline, AstraZeneca and Novartis; and a grant from the Stanley Foundation. JT is a member of advisory boards for AstraZeneca, Janssen-Cilag and Otsuka. Other authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Taipale, H., Vuorikari, H., Tanskanen, A. et al. Prevalence of Drug Combinations Increasing Bleeding Risk Among Warfarin Users With and Without Alzheimer’s Disease. Drugs Aging 32, 937–945 (2015). https://doi.org/10.1007/s40266-015-0316-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-015-0316-3