Abstract
Objective
To quantify the risk of arrhythmias and conduction disorders (ACD) in patients receiving direct-acting antiviral (DAA) therapy for hepatitis C.
Design
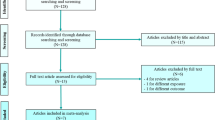
All individuals aged 18 to 85 years old treated with DAAs between 01 January 2014 and 31 December 2021 were selected from the French national healthcare database (SNDS). Individuals with a history of ACD were excluded. The primary outcome was the incidence of hospitalization or medical procedure for ACD. Marginal structural models were used to adjust for age, sex, medical comorbidities, and concomitant medications.
Results
After analyzing 87,589 individuals (median age, 52 years; 60% male) from 01 January 2014 to 31 December 2021, 2131 hospitalizations or medical procedures for ACD were observed over 672,572 person-years (PY) of follow-up. The incidence of ACD was 245/100,000 PY [95% confidence interval (CI), 228–263/100,000 PY] before DAA and 375/100,000 PY (95% CI 355–395/100,000 PY) after DAA exposure (rate ratio 1.53; 95% CI 1.40–1.68; P < 0.001). The risk of ACD was increased after DAA exposure, compared with the pre-DAA period (adjusted hazard ratio,1.66; 95% CI 1.43–1.93; P < 0.001). The increase in ACD risk was similar among individuals treated with sofosbuvir-based and sofosbuvir-free regimens. Of the 1398 ACD detected after DAA exposure, 30% were hospitalizations for atrial fibrillation, 25% were medical procedures for ACD, and 15% were hospitalizations for atrioventricular blocks.
Conclusion
A significant increase in the risk of ACD was observed in the population-level cohort of individuals treated with DAAs, regardless of the regimen. Further research is needed to identify patients at risk of ACD, determine cardiac monitoring strategies, and evaluate the need for Holter monitoring after DAA therapy.

Similar content being viewed by others
References
Pol S, Lair-Mehiri L, Vallet-Pichard A. Is elimination of HCV realistic by 2030: France. Liver Int. 2021;41(Suppl 1):45–9.
Pawlotsky J-M, Negro F, Aghemo A, Berenguer M, Dalgard O, Dusheiko G, et al. EASL recommendations on treatment of hepatitis C: final update of the series☆. J Hepatol. 2020;73:1170–218.
Carrat F, Fontaine H, Dorival C, Simony M, Diallo A, Hezode C, et al. Clinical outcomes in patients with chronic hepatitis C after direct-acting antiviral treatment: a prospective cohort study. The Lancet. 2019;393:1453–64.
McGlynn EA, Adams JL, Kramer J, Sahota AK, Silverberg MJ, Shenkman E, et al. Assessing the safety of direct-acting antiviral agents for hepatitis C. JAMA Netw Open. 2019;2: e194765.
Herbst AL, Ulfelder H, Poskanzer DC. Adenocarcinoma of the vagina: association of maternal stilbestrol therapy with tumor appearance in young women. N Engl J Med. 1971;284:878–81.
Brewer T, Colditz GA. Postmarketing surveillance and adverse drug reactions: current perspectives and future needs. JAMA. 1999;281:824.
Fontaine H, Lazarus A, Pol S, Pecriaux C, Bagate F, Sultanik P, et al. Bradyarrhythmias associated with sofosbuvir treatment. N Engl J Med. 2015;373:1886–8.
FDA. Center for Drug Evaluation and Research. Application number: 204671Orig1s000. Pharmacology Review(s). [Internet]. 2013. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204671Orig1s000PharmR.pdf
Food and Drug Administration. FDA Drug Safety Communication: FDA warns of serious slowing of the heart rate when antiarrhythmic drug amiodarone is used with hepatitis C treatments containing sofosbuvir (Harvoni) or Sovaldi in combination with another direct acting antiviral drug [Internet]. FDA; 2015. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-serious-slowing-heart-rate-when-antiarrhythmic-drug
Lam L, Fontaine H, Lapidus N, Dorival C, Bellet J, Larrey D, et al. Impact of direct-acting antiviral treatment for hepatitis C on cardiovascular diseases and extrahepatic cancers. Pharmacoepidemiol Drug Saf. 2023;32:486–95.
Tuppin P, Rudant J, Constantinou P, Gastaldi-Ménager C, Rachas A, de Roquefeuil L, et al. Value of a national administrative database to guide public decisions: from the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017;65:S149–67.
Hayes KN, Burkard T, Weiler S, Tadrous M, Burden AM. Global adverse events reported for direct-acting antiviral therapies for the treatment of hepatitis C: an analysis of the World Health Organization VigiBase. Eur J Gastroenterol Hepatol. 2021;33:e1017–21.
Lam L, Carrat F. Immortal time and selection biases in study of direct-acting antiviral treatment and hepatitis c outcomes. JAMA Intern Med. 2023;183:624.
Ogawa E, Chien N, Kam L, Yeo YH, Ji F, Huang DQ, et al. Association of direct-acting antiviral therapy with liver and nonliver complications and long-term mortality in patients with chronic hepatitis C. JAMA Intern Med. 2023;183:97.
Back DJ, Burger DM. Interaction between amiodarone and sofosbuvir-based treatment for hepatitis C virus infection: potential mechanisms and lessons to be learned. Gastroenterology. 2015;149:1315–7.
Ahmad T, Yin P, Saffitz J, Pockros PJ, Lalezari J, Shiffman M, et al. Cardiac dysfunction associated with a nucleotide polymerase inhibitor for treatment of hepatitis C. Hepatology. 2015;62:409–16.
Laurain A, Kramer L, Sultanik P, Vallet-Pichard A, Sogni P, Pol S. Mortality associated with the treatment of HCV with direct-acting antivirals. Gut. 2018;67:197–8.
Mazzitelli M, Torti C, Sabatino J, D’Ascoli GL, Costa C, Pisani V, et al. Evaluation of cardiac function by global longitudinal strain before and after treatment with sofosbuvir-based regimens in HCV infected patients. BMC Infect Dis. 2018;18:518.
Lamarre D, Anderson PC, Bailey M, Beaulieu P, Bolger G, Bonneau P, et al. An NS3 protease inhibitor with antiviral effects in humans infected with hepatitis C virus. Nature. 2003;426:186–9.
Touafchia A, Bagheri H, Carrié D, Durrieu G, Sommet A, Chouchana L, et al. Serious bradycardia and remdesivir for coronavirus 2019 (COVID-19): a new safety concerns. Clin Microbiol Infect. 2021;27:791.e5-791.e8.
Bezin J, Duong M, Lassalle R, Droz C, Pariente A, Blin P, et al. The national healthcare system claims databases in France, SNIIRAM and EGB: powerful tools for pharmacoepidemiology. Pharmacoepidemiol Drug Saf. 2017;26:954–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
FC reports grants from INSERM-ANRS; personal fees from Sanofi, outside the submitted work. SP has received consulting and lecturing fees from Janssen, Gilead, MSD, Abbvie, Biotest, Shinogui, Viiv, LFB, and grants from Bristol-Myers Squibb, Gilead, Roche and MSD without relation to this manuscript. AC has received research grants from ARS, RESICARD (research nurses), and Boehringer-Ingelheim; and consultant and lecture fees from Amgen, AstraZeneca, Bayer Pharma, BMS-Pfizer alliance, Boehringer-Ingelheim, Daiichi Sankyo, Novartis, and VIFOR. LL has nothing to disclose.
Availability of data and material
Due to the nature of this research based on the French administrative health care database, data that support the findings of this study are not available due to ethical and legal restrictions.
Ethics approval
The authors had permanent access to the SNDS (French decree no. 2021-848). All data were anonymized, and no informed consent was required. The study was approved by INSERM CepiDC and conducted in accordance with the Declaration of Helsinki and the French law on biomedical research. Ethics approval by an ethics committee or institutional review board was not required for this research.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Code availability
Not applicable.
Author Contributions
LL and FC had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: LL and FC. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: LL. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: LL and FC. All authors read and approved the final version of the submission.
Transparency Statement
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lam, L., Pol, S., Cohen, A. et al. Direct-Acting Antivirals and the Risk of Arrhythmias and Conduction Disorders in Patients with Chronic Hepatitis C: A French Nationwide Cohort Study. Drugs 83, 1207–1213 (2023). https://doi.org/10.1007/s40265-023-01918-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01918-0