Abstract
Idarucizumab (Praxbind®) is a fully humanized, monoclonal antibody fragment developed by Boehringer Ingelheim as a specific antidote to reverse the anticoagulant effect of the direct oral thrombin inhibitor dabigatran etexilate (Pradaxa®). Idarucizumab received its first global approval, in the USA, in October 2015 for use in adult patients treated with dabigatran etexilate when rapid reversal of its anticoagulant effects is required for emergency surgery/urgent procedures or in life-threatening or uncontrolled bleeding. Regulatory applications have been submitted in Canada and in the EU, where it has received a positive opinion from the European Medicines Agency’s Committee for Medicinal Products for Human Use. This article summarizes the milestones in the development of idarucizumab leading to this first approval for reversing the anticoagulant effects of dabigatran in adults.
Similar content being viewed by others
References
Boehringer Ingelheim. Pradaxa® (dabigatran etexilate mesylate) capsules for oral use: US prescribing infomation. 2015. http://www.boehringer-ingelheim.com/. Accessed 19 Oct 2015.
European Medicines Agency. Pradaxa 110 mg hard capsules: summary of product characteristics. 2015. http://www.ema.europa.eu/. Accessed 19 Oct 2015.
Siegal DM. Managing target-specific oral anticoagulant associated bleeding including an update on pharmacological reversal agents. J Thromb Thrombol. 2015;39(3):395–402.
Costin J, Ansell J, Laulicht B, et al. Reversal agents in development for the new oral anticoagulants. Postgrad Med. 2014;126(7):19–24.
Boehringer Ingelheim. Praxbind® (idarucizumab) injection, for intravenous use: US prescribing information. 2015. http://us.boehringer-ingelheim.com. Accessed 2015.
Boehringer Ingelheim. Boehringer Ingelheim’s investigational antidote for Pradaxa® (dabigatran etexilate mesylate) receives FDA breakthrough therapy designation [media release]. 26 Jun 2014.
Boehringer Ingelheim. FDA grants priority review to Boehringer Ingelheim’s biologics license application for idarucizumab [media release]. 23 Apr 2015.
FDA. FDA approves Praxbind, the first reversal agent for the anticoagulant Pradaxa [media release]. Accessed 16 Oct 2015. http://fda.gov.
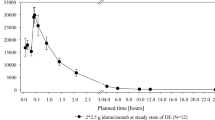
Glund S, Stangier J, Schmohl M, et al. Safety, tolerability, and efficacy of idarucizumab for the reversal of the anticoagulant effect of dabigatran in healthy male volunteers: a randomised, placebo-controlled, double-blind phase 1 trial. Lancet. 2015;386(9994):680–90.
EMA. EMA fast-tracks antidote to anticoagulant Pradaxa [media release]. http://www.ema.europa.eu/. Accessed 25 Sep 2015.
Boehringer Ingelheim Pharmaceuticals Inc. FDA approves Praxbind® (idarucizumab), specific reversal agent for Pradaxa® (dabigatran etexilate mesylate) [media release]. http://us.boehringer-ingelheim.com/news_events/press_releases/press_release_archive/2015/10-16-2015-fda-approves-praxbind-idarucizumab-specific-reversal-agent-pradaxa-dabigatran-etexilate-mesylate.html. Accessed 16 Oct 2015.
Boehringer Ingelheim. Boehringer Ingelheim submits applications for approval of idarucizumab, specific reversal agent to dabigatran etexilate (Pradaxa®), to EMA, FDA and Health Canada [media release]. Accessed 3 Mar 2015.
Schiele F, van Ryn J, Canada K, et al. A specific antidote for dabigatran: functional and structural characterization. Blood. 2013;121(18):3554–62.
Grottke O, Honickel M, van Ryn J, et al. Idarucizumab, a specific dabigatran reversal agent, reduces blood loss in a porcine model of trauma with dabigatran anticoagulation. J Am Coll Cardiol. 2015;66(13):1518–9.
Honickel M, Grottke O, Van Ryn J, et al. Use of a specific antidote to dabigatran (idarucizumab) reduces blood loss and mortality in dabigatran-induced and trauma-induced bleeding in pigs [abstract no. P99]. Crit Care. 2014;18(Suppl 1):S34–5.
Honickel M, van Ryn J, Rossaint R, et al. Effects of idarucizumab, given as a split dose, in a blunt liver double trauma model in pigs receiving dabigatran [abstract no. OR067]. J Thromb Haemost. 2015;13(Suppl 2):119.
Grottke O, Honickel M, Van Ryn J, et al. Dabigatran-induced anticoagulant and bleeding effects can be reversed with both prothrombin complex concentrates and a specific antidote (idarucizumab) in a lethal porcine polytrauma model [abstract no. 4844]. Eur Heart J. 2014;35(Abstract Supplement):863.
Grottke O, Van Ryn J, Rossaint R. In a trauma experimental pig model prothrombin complex concentrates and a specific antidote (idarucizumab) are effective to reverse the anticoagulant effects of dabigatran [abstract no. P118]. Crit Care. 2014;18(Suppl 1):S41.
Honickel M, Braunschweig T, Ryn JV, et al. Efficacy of idarucizumab, prothrombin complex concentrate (PCC) and activated PCC to reverse the anticoagulatory potential of dabigatran in a porcine polytrauma model [abstract no. P351]. Crit Care. 2015;19(Suppl 1):S123.
Honickel M, Braunschweig T, Rossaint R, et al. Prothrombin complex concentrate or idarucizumab in combination with fibrinogen plus tranexamic acid are equally effective in a dabigatran anticoagulation experimental polytrauma model [abstract no. 4978]. Eur Heart J. 2015;36(Abstract Supplement):861.
Honickel M, Treutler S, van Ryn J, et al. Reversal of dabigatran anticoagulation ex vivo: porcine study comparing prothrombin complex concentrates and idarucizumab. Thromb Haemost. 2015;113(4):728–40.
Grottke O, van Ryn J, Zentai C. Resuscitation with different infusion solutions does not influence binding of dabigatran to its specific antidote in a pig model of hemorrhagic shock [abstract]. Circulation. 2013;128(Suppl):356.
Glund S, Moschetti V, Norris S, et al. A randomised study in healthy volunteers to investigate the safety, tolerability and pharmacokinetics of idarucizumab, a specific antidote to dabigatran. Thromb Haemost. 2015;113(5):943–51.
Stangier J, Schmohl M, Glund S, et al. Idarucizumab does not have prothrombotic effects: assessment of coagulation markers in healthy volunteers [abstract no. OR320]. J Thromb Haemost. 2015;13(Suppl 2):217.
van Ryn J, Schmoll M, Pillu H, et al. Effect of dabigatran on the ability to generate fbrin at a wound site and its reversal by idarucizumab, the antidote to dabigatran, in healthy volunteers: an exploratory marker of blood loss [abstract no. 18403]. Circulation. 2014;130(Suppl 2).
Pollack CV, Reilly PA, Eikelboom J, et al. Idarucizumab for dabigatran reversal. N Engl J Med. 2015;373(6):511–20.
Levy JH, Verhamme P, Sellke FW, et al. Initial experience with idarucizumab in dabigatran-treated patients requiring emergency surgery or interventon: interim results from the RE-VERSE AD study [abstract no. P5967]. Eur Heart J. 2015;36(Abstract Supplement):1043.
Glund S, Stangier J, Schmohl M, et al. Idarucizumab, a specific antidote for dabigatran: immediate, complete and sustained reversal of dabigatran induced anticoagulation in elderly and renally impaired subjects [abstract no. 344]. 56th Annual Meeting and Exposition of the American Society of Hematology; 8 Dec 2014; San Francisco, CA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the author on the basis of scientific completeness and accuracy. C.B. Burness is a salaried employee of Adis, Springer SBM.
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Burness, C.B. Idarucizumab: First Global Approval. Drugs 75, 2155–2161 (2015). https://doi.org/10.1007/s40265-015-0508-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-015-0508-5