Abstract
Introduction
Globally, chronic kidney disease (CKD) is one of the leading causes of mortality. Impaired renal function makes CKD patients vulnerable to drug-related problems (DRPs).
Aim
The aim of this systematic review was to investigate the prevalence and nature of DRPs among hospital in-patients with CKD.
Methods
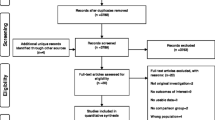
A systematic review of the literature was conducted using Medline, EMBASE, PsycINFO, Web of Science (Core Collection), CINAHL plus (EBSCO), Cochrane Library (Wiley), Scopus (ELSEVIER) and PubMed (U.S.NLM) from index inception to January 2020. Studies investigating DRPs in hospitalised CKD patients published in the English language were included. Two independent reviewers extracted the data and undertook quality assessment using the Joanna Briggs Institute (JBI) tool.
Results
A total of 2895 unique titles were identified; with 20 meeting the inclusion criteria. DRPs prevalence in CKD was reported between 12 and 87%. The most common DRPs included ineffective treatment, inappropriate drug choice and dosing problems. Antibiotics, H2-antihistamines and oral antidiabetics (metformin) were common drug classes involved in DRPs. Factors associated with DRPs included severity of CKD, the number of medications taken, age, length of hospital stay, and gender.
Conclusion
This systematic review provides evidence that DRPs are a frequent occurrence and burden for hospitalised patients with stage 1–4 CKD. Heterogeneity in study design, case detection and definitions are common, and future studies should use clearer definitions and study designs.
Protocol Registration: PROSPERO: CRD42018096364




Similar content being viewed by others
References
Levin A, Stevens PE, Bilous RW, Coresh J, De Francisco ALM, De Jong PE, et al. Kidney disease: Improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter 2013;3(1):1–150. https://doi.org/10.1038/kisup.2012.73.
Berns J. Patient education: Chronic kidney disease (Beyond the Basics). In: UpToDate, Curhan GC and Motwani S (Ed), UpToDate, Waltham, MA. Accessed 4 May 2021.
Cao H. Medication in Chronic Kidney Disease. In: Yang J, He W (eds). Chronic Kidney Disease: Diagnosis and Treatment. Singapore: Springer Singapore; 2020. p. 187–98. https://doi.org/10.1007/978-981-32-9131-7_15.
Pannu N, Nadim MK. An overview of drug-induced acute kidney injury. Crit Care Med. 2008;36(4):S216–23. https://doi.org/10.0473/CCM.0b013e318168e375.
Kerr M, Bray B, Medcalf J, O’Donoghue DJ, Matthews B. Estimating the financial cost of chronic kidney disease to the NHS in England. Nephrol Dial Transplant. 2012;27(Suppl 3):iii73–80. https://doi.org/10.1093/ndt/gfs269.
Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1459–544. https://doi.org/10.1016/S0140-6736(16)31012-1.
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE. 2016;11(7): e0158765. https://doi.org/10.1371/journal.pone.0158765.
Public Health England. Chronic kidney disease prevalence model. In: CKD prevalence estimates for local and regional populations Public Health England, London. 2014. https://www.assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/612303/ChronickidneydiseaseCKDprevalencemodelbriefing.pdf. Accessed 6 May 2021.
Adusumilli PK, Adepu R. Drug related problems: an over view of various classification systems. Asian J Pharm Clin Res. 2014;7(4):7–10.
Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–43. https://doi.org/10.1093/ajhp/47.3.533.
Van Mil J, Horvat N, Westerlund T. The Pharmaceutical Care Network Europe Classification for Drug related problems V9.1. Pharmaceutical Care Network Europe Association, Zuidlaren, p. 10. 2020. https://www.pcne.org/working-groups/2/drug-related-problem-classification. Accessed 6 May 2021.
Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168(17):1890–6. https://doi.org/10.03233/archinternmed.2008.3.
Aronson JK, Ferner RE. Clarification of terminology in drug safety. Drug Saf. 2005;28(10):851–70. https://doi.org/10.2165/00002018-200528100-00003.
Ferner RE, Aronson JK. Clarification of terminology in medication errors. Drug Saf. 2006;29(11):1011–22. https://doi.org/10.2165/00002018-200629110-00001.
Ruths S, Viktil KK, Blix HS. Classification of drug-related problems. Tidsskr Nor Laegeforen. 2007;127(23):3073–6.
Wester K, Jonsson AK, Spigset O, Druid H, Hagg S. Incidence of fatal adverse drug reactions: a population based study. Br J Clin Pharmacol. 2008;65(4):573–9. https://doi.org/10.1111/j.1365-2125.2007.03064.x.
Rozich JD, Resar RK. Medication safety: one organization’s approach to the challenge. J Clin Outcomes Manag. 2001;8(10):27–34.
Quintana-Bárcena P, Lord A, Lizotte A, Berbiche D, Lalonde L. Prevalence and management of drug-related problems in chronic kidney disease patients by severity level: a subanalysis of a cluster randomized controlled trial in community pharmacies. J Manag Care Spec Pharm. 2018;24(2):173–81. https://doi.org/10.18553/jmcp.2018.24.2.173.
Adibe MO, Igboeli NU, Ukwe CV. Evaluation of drug therapy problems among renal patients receiving care in some tertiary hospitals in Nigeria. Trop J Pharm Res. 2017;16(3):697–704. https://doi.org/10.4314/tjpr.v16i3.27.
Abunahlah N, Elawaisi A, Velibeyoglu FM, Sancar M. Drug related problems identified by clinical pharmacist at the Internal Medicine Ward in Turkey. Int J Clin Pharm. 2018;40(2):360–7. https://doi.org/10.1007/s11096-017-0585-5.
Breton G, Froissart M, Janus N, Launay-Vacher V, Berr C, Tzourio C, et al. Inappropriate drug use and mortality in community-dwelling elderly with impaired kidney function—the Three-City population-based study. Nephrol Dial Transplant. 2011;26(9):2852–9. https://doi.org/10.1093/ndt/gfq827.
Danial M, Hassali MA, Meng OL, Kin YC, Khan AH. Development of a mortality score to assess risk of adverse drug reactions among hospitalized patients with moderate to severe chronic kidney disease. BMC Pharmacol Toxicol. 2019;20(1):41. https://doi.org/10.1186/s40360-019-0318-6.
Nivya K, Kiran VSS, Ragoo N, Jayaprakash B, Sekhar MS. Systemic review on drug related hospital admissions—a pubmed based search. Saudi Pharm J. 2015;23(1):1–8. https://doi.org/10.03248/j.jsps.2013.05.006.
Patel NS, Patel TK, Patel PB, Naik VN, Tripathi C. Hospitalizations due to preventable adverse reactions—a systematic review. Eur J Clin Pharmacol. 2017;73(4):385–98. https://doi.org/10.1007/s00228-016-2170-6.
Dorks M, Allers K, Schmiemann G, Herget-Rosenthal S, Hoffmann F. Inappropriate medication in non-hospitalized patients with renal insufficiency: a systematic review. J Am Geriatr Soc. 2017;65(4):853–62. https://doi.org/10.1111/jgs.14809.
Tesfaye WH, Castelino RL, Wimmer BC, Zaidi STR. Inappropriate prescribing in chronic kidney disease: A systematic review of prevalence, associated clinical outcomes and impact of interventions. Int J Clin Pract. 2017;71:7. https://doi.org/10.1111/ijcp.12960.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147–53. https://doi.org/10.0473/XEB.0000000000000054.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1.
Alruqayb W, Price M, Paudyal V, Cox A. Drug-related problems in hospitalised patients with chronic kidney disease: a systematic review protocol. PROSPERO 2018 CRD42018096364. 2018.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123. https://doi.org/10.05967/ijhpm.2014.71.
Sheen SS, Choi JE, Park RW, Kim EY, Lee YH, Kang UG. Overdose rate of drugs requiring renal dose adjustment: data analysis of 4 years prescriptions at a tertiary teaching hospital. J Gen Intern Med. 2007;23(4):423–8. https://doi.org/10.03239/s11606-007-0336-8.
Gomez-Lobon A, Delgado-Sanchez O, Modamio P, Alvarez-Arroyo L, Campoamor-Ladin F, Marino EL. Drug prescribing in patients with impaired renal function: are interventions still needed to improve patient safety? Lat Am J Pharm. 2012;31(2):340–3.
Shigematsu T, Muraoka R, Sugimoto T, Nishizawa Y. Risedronate therapy in patients with mild-to-moderate chronic kidney disease with osteoporosis: post-hoc analysis of data from the risedronate phase III clinical trials. BMC Nephrol. 2017;18(1):1–8. https://doi.org/10.1186/s12882-017-0478-9.
Won H-J, Chung G, Lee KJ, Lee E, Son S, Choi S, et al. Evaluation of medication dosing errors in elderly patients with renal impairment. Int J Clin Pharmacol Ther. 2018;56(8):358. https://doi.org/10.5414/CP203258.
Garedow AW, Mulisa Bobasa E, Desalegn Wolide A, Kerga Dibaba F, Gashe Fufa F, Idilu Tufa B, et al. Drug-related problems and associated factors among patients admitted with chronic kidney disease at Jimma University Medical Center, Jimma Zone, Jimma, Southwest Ethiopia: a hospital-based prospective observational study. Int J Nephrol. 2019;2019:9. https://doi.org/10.1155/2019/1504371.
Sweileh WM, Janem SA, Sawalha AF, Abu-Taha AS, Zyoud SH, Sabri IA, et al. Medication dosing errors in hospitalized patients with renal impairment: a study in Palestine. Pharmacoepidemiol Drug Saf. 2007;16(8):908–12. https://doi.org/10.1002/pds.1412.
Prajapati A, Ganguly B. Appropriateness of drug dose and frequency in patients with renal dysfunction in a tertiary care hospital: a cross-sectional study. J Pharm Bioallied Sci. 2013;5(2):136. https://doi.org/10.0167/0975-7406.111829.
Manjula Devi AS, Thomas B, Joseph A, Sravani K. Prospective evaluation of drug prescribing and improvement of drug safety in renal failure patients. Hygeia J D Med. 2014;6(2):25–35. https://doi.org/10.15254/H.J.D.Med.6.2014.133.
Juarez-Cedillo T, Martinez-Hernandez C, Hernandez-Constantino A, Garcia-Cruz JC, et al. Clinical weighting of drug-drug interactions in hospitalized elderly. Basic Clin Pharmacol Toxicol. 2016;118(4):298–305. https://doi.org/10.1111/bcpt.12495.
O’Shaughnessy M, Allen N, O’Regan J, Payne-Danson E, Mentre L, Davin D, et al. Agreement between renal prescribing references and determination of prescribing appropriateness in hospitalized patients with chronic kidney disease. QJM-Int J Med. 2017;110(10):623–8. https://doi.org/10.1093/qjmed/hcx086.
Getachew H, Tadesse Y, Shibeshi W. Drug dosage adjustment in hospitalized patients with renal impairment at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. BMC Nephrol. 2015;16(1):1–9. https://doi.org/10.1186/s12882-015-0155-9.
Yang P, Chen N, Wang RR, Li L, Jiang SP. Inappropriateness of medication prescriptions about chronic kidney disease patients without dialysis therapy in a Chinese tertiary teaching hospital. Ther Clin Risk Manag. 2016;12:1517–24. https://doi.org/10.0899/TCRM.S116789.
Markota NP, Markota I, Tomic M, Zelenika A. Inappropriate drug dosage adjustments in patients with renal impairment. J Nephrol. 2009;22(4):497–501.
Shalini A, Agarwal S, Joshi MC. A study of inappropriate dosing of antibacterial agents in consideration with estimated GFR values. Indian J Public Health Res Dev. 2013;4(4):173–8.
Nielsen AL, Henriksen DP, Marinakis C, Hellebek A, Birn H, Nybo M, et al. Drug dosing in patients with renal insufficiency in a hospital setting using electronic prescribing and automated reporting of estimated glomerular filtration rate. Basic Clin Pharmacol Toxicol. 2013;114(5):407–13. https://doi.org/10.1111/bcpt.12185.
Saleem A, Masood I. Pattern and predictors of medication dosing errors in chronic kidney disease patients in pakistan: a single center retrospective analysis. PLoS ONE. 2016;11(7):e0158677. https://doi.org/10.1371/journal.pone.0158677.
Saleem A, Masood I, Khan TM. Clinical relevancy and determinants of potential drug-drug interactions in chronic kidney disease patients: results from a retrospective analysis. Integr Pharm Res Pract. 2017;6:71–7. https://doi.org/10.0899/IPRP.S128816.
Sharif-Askari FS, Syed-Sulaiman SA, Saheb-Sharif-Askari N, Al-Sayed-Hussain A. Development of an adverse drug reaction risk assessment score among hospitalized patients with chronic kidney disease. PLoS ONE. 2014;9(4):e95991. https://doi.org/10.1371/journal.pone.0095991.
Taner N, Cattik BN, Berk B. A contraindication to metfromin therapy: renal impairment—adherence to prescribing guidelines at a hospital in Turkey. Acta Pharmaceutica Sci. 2018;56(1):63–70. https://doi.org/10.23893/1307-2080.APS.05604.
Holm H, Bjerke K, Holst L, Mathiesen L. Use of renal risk drugs in patients with renal impairment. Int J Clin Pharm. 2015;37(6):1136–42. https://doi.org/10.1007/s11096-015-0175-3.
Stemer G, Lemmens-Gruber R. Clinical pharmacy activities in chronic kidney disease and end-stage renal disease patients: a systematic literature review. BMC Nephrol. 2011;12(1):35. https://doi.org/10.1186/1471-2369-12-35.
Long CL, Raebel MA, Price DW, Magid DJ. Compliance with dosing guidelines in patients with chronic kidney disease. Ann Pharmacother. 2004;38(5):853–8. https://doi.org/10.1345/aph.1D399.
Jones GR. Estimating renal function for drug dosing decisions. Clincs. 2011;32(2):81–8.
Karsch-Volk M, Schmid E, Wagenpfeil S, Linde K, Heemann U, Schneider A. Kidney function and clinical recommendations of drug dose adjustment in geriatric patients. BMC Geriatr. 2013;10(13):92. https://doi.org/10.1186/1471-2318-13-92.
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47. https://doi.org/10.7326/0003-4819-139-2-200307150-00013.
Poggio ED, Wang X, Greene T, Van Lente F, Hall PM. Performance of the modification of diet in renal disease and Cockcroft-Gault equations in the estimation of GFR in health and in chronic kidney disease. J Am Soc Nephrol. 2005;16(2):459–66. https://doi.org/10.1681/ASN.2004060447.
Trinkley KE, Michelle-Nikels S, Page IRL, Joy MS. Automating and estimating glomerular filtration rate for dosing medications and staging chronic kidney disease. Int J Gen Med. 2014;7:211–8. https://doi.org/10.2147/IJGM.S61795.
Khanal A, Peterson GM, Jose MD, Castelino RL. Comparison of equations for dosing of medications in renal impairment. Nephrology. 2017;22(6):470–7. https://doi.org/10.1111/nep.12834.
Lessard BA, Zaiken K. Comparison of equations for dosing of medications requiring renal adjustment. J Am Pharm Assoc. 2013;53(1):54–7. https://doi.org/10.1331/JAPhA.2013.11241.
Drion I, Joosten H, Santing L, Logtenberg SJJ, Groenier KH, Lieverse AG, et al. The Cockcroft-Gault: a better predictor of renal function in an overweight and obese diabetic population. Obes Fact. 2011;4(5):393–9. https://doi.org/10.1159/000333399.
Park EJ, Wu K, Mi Z, Dong T, Lawrence JP, Ko CW, et al. A systematic comparison of Cockcroft-Gault and modification of diet in renal disease equations for classification of kidney dysfunction and dosage adjustment. Ann Pharmacother. 2012;46(9):1174–87. https://doi.org/10.1345/aph.1Q757.
Gill J, Malyuk R, Djurdjev O, Levin A. Use of GFR equations to adjust drug doses in an elderly multi-ethnic group—a cautionary tale. Nephrol Dial Transplant. 2007;22(10):2894–9. https://doi.org/10.1093/ndt/gfm289.
National Kidney Disease Education Program. CKD & Drug Dosing: Information for Providers Estimation of Kidney Function for Prescription Medication Dosage in Adults. 2015. https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/ckd-drug-dosing-providers.
Dowling TC, Wang ES, Ferrucci L, Sorkin JD. Glomerular filtration rate equations overestimate creatinine clearance in older individuals enrolled in the baltimore longitudinal study on aging: Impact on renal drug dosing. Pharmacotherapy. 2013;33(9):912–21. https://doi.org/10.1002/phar.1282.
Hoffmann F, Boeschen D, Dorks M, Herget-Rosenthal S, Petersen J, Schmiemann G. Renal insufficiency and medication in nursing home residents-a cross-sectional study (IMREN) [German]. Dtsch Ärzteblatt Int. 2016;113(6):92–8. https://doi.org/10.3238/arztebl.2016.0092.
The National Institute of Diabetes and Digestive and Kidney Diseases. Estimation of Kidney Function for Prescription Medication Dosage in Adults. In: CKD & Drug Dosing: Information for Providers 2015. http://www.niddk.nih.gov/health-information/professionals/advanced-search/ckd-drug-dosing-providers. Accessed 4 May 2021.
Manias E. Detection of medication-related problems in hospital practice: a review. Br J Clin Pharmacol. 2013;76(1):7–20. https://doi.org/10.1111/bcp.12049.
Meyer-Massetti C, Cheng CM, Schwappach DL, Paulsen L, Ide B, Meier CR, et al. Systematic review of medication safety assessment methods. Am J Health Syst Pharm. 2011;68(3):227–40. https://doi.org/10.2146/ajhp100019.
Grasso BC, Genest R, Jordan CW, Bates DW. Use of chart and record reviews to detect medication errors in a state psychiatric hospital. Psychiatr Serv. 2003;54(5):677–81. https://doi.org/10.1176/appi.ps.54.5.677.
Vidal L, Shavit M, Fraser A, Paul M, Leibovici L. Systematic comparison of four sources of drug information regarding adjustment of dose for renal function. Br Med J. 2005;331(7511):263. https://doi.org/10.1136/bmj.38476.471088.3A.
Khanal A, Castelino R, Peterson G, Jose M. Dose adjustment guidelines for medications in patients with renal impairment: how consistent are drug information sources? Intern Med J. 2014;44(1):77–85. https://doi.org/10.1111/imj.12291.
Dalrymple LS, Go AS. Epidemiology of acute infections among patients with chronic kidney disease. Clin J Am Soc Nephrol. 2008;3(5):1487–93. https://doi.org/10.2215/CJN.01290308.
Ishigami J, Matsushita K. Clinical epidemiology of infectious disease among patients with chronic kidney disease. Clin Exp Nephrol. 2019;23(4):437–47. https://doi.org/10.1007/s10157-018-1641-8.
Doody HK, Peterson GM, Watson D, Castelino RL. Retrospective evaluation of potentially inappropriate prescribing in hospitalized patients with renal impairment. Curr Med Res Opin. 2015;31(3):525–35. https://doi.org/10.1185/03007995.2015.1010036.
Chang F, O’Hare AM, Miao Y, Steinman MA. Use of renally inappropriate medications in older veterans: a national study. J Am Geriatr Soc. 2015;63(11):2290–7. https://doi.org/10.1111/jgs.13790.
Roberts DM, Sevastos J, Carland JE, Stocker SL, Lea-Henry TN. Clinical pharmacokinetics in kidney disease: Application to rational design of dosing regimens. Clin J Am Soc Nephrol. 2018;13(8):1254–63. https://doi.org/10.2215/CJN.05150418.
Lea-Henry TN, Carland JE, Stocker SL, Sevastos J, Roberts DM. Clinical pharmacokinetics in kidney disease: fundamental principles. Clin J Am Soc Nephrol. 2018;13(7):1085–95. https://doi.org/10.2215/CJN.00340118.
Manlucu J, Tonelli M, Ray JG, Papaioannou A, Youssef G, Thiessen-Philbrook HR, et al. Dose-reducing H2 receptor antagonists in the presence of low glomerular filtration rate: a systematic review of the evidence. Nephrol Dial Transplant. 2005;20(11):2376–84. https://doi.org/10.1093/ndt/gfi025.
Defronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: current perspectives on causes and risk. Metabolism. 2016;65(2):20–9. https://doi.org/10.1016/j.metabol.2015.10.014.
Inzucchi SEMD, Lipska KJMDMHS, Mayo HMLS, Bailey CJP, McGuire DKMDM. Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA. 2014;312(24):2668–75. https://doi.org/10.03233/jama.2014.15298.
Vecchio S, Giampreti A, Petrolini VM, Lonati D, Protti A, Papa P, et al. Metformin accumulation: lactic acidosis and high plasmatic metformin levels in a retrospective case series of 66 patients on chronic therapy. Clin Toxicol. 2014;52(2):129–35. https://doi.org/10.3109/15563650.2013.860985.
Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol. 2017;69(23):2779–90. https://doi.org/10.08245/atm.2017.09.19.
Peterson C, Gustafsson M. Characterisation of drug-related problems and associated factors at a clinical pharmacist service-naïve hospital in northern Sweden. Drugs-Real World Outcomes. 2017;4(2):97–107. https://doi.org/10.1007/s40801-017-0108-7.
Scott IA, Hilmer SN, Reeve E, Potter K, Le Couteur D, Rigby D, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827–34. https://doi.org/10.1001/jamainternmed.2015.0324.
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314(17):1818–30. https://doi.org/10.03233/jama.2015.13766.
Whittaker CF, Miklich MA, Patel RS, Fink JC. Medication safety principles and practice in CKD. Clin J Am Soc Nephrol. 2018;13(11):1738–46. https://doi.org/10.2215/CJN.00580118.
Urbina O, Ferrández O, Grau S, Luque S, Mojal S, Marin-Casino M, et al. Design of a score to identify hospitalized patients at risk of drug-related problems. Pharmacoepidemiol Drug Saf. 2014;23(9):923–32. https://doi.org/10.1002/pds.3634.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study was funded by the University of Birmingham, and The Saudi Cultural Bureau funded Wadia Alruqayb’s PhD studies. MJP is supported by the NIHR Birmingham Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Conflicts of Interest/Competing Interests
Wadia S. Alruqayb, Malcolm J. Price, Vibhu Paudyal and Anthony R. Cox have no conflicts of interest relevant to the content of this study.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Collated data from the study is available from the authors on request.
Code Availability
Not applicable.
Authors’ Contributions
All authors contributed to this systematic review and writing the manuscript. WA conducted the searches, data extraction and synthesis, with contributions and review by VP and AC. MP reviewed the data and synthesis. All authors read and approved the final version of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alruqayb, W.S., Price, M.J., Paudyal, V. et al. Drug-Related Problems in Hospitalised Patients with Chronic Kidney Disease: A Systematic Review. Drug Saf 44, 1041–1058 (2021). https://doi.org/10.1007/s40264-021-01099-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-021-01099-3