Abstract
Introduction
Antidepressant use during the first trimester is reported in 4–8% of pregnancies. The use of some selective serotonin reuptake inhibitors during the first trimester has been identified as increasing the odds for congenital heart defects; however, little is known about the safety of non-selective serotonin reuptake inhibitor antidepressants.
Objective
The objective of this study was to assess the odds of congenital heart defects associated with the use of antidepressants during the first trimester of pregnancy, and to update the literature as newer studies have been published since the latest systematic literature review and meta-analysis.
Methods
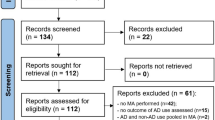
PubMed and Embase were searched till 3 June, 2020. Study quality was assessed, and study details were extracted. Meta-analyses were performed using RevMan 5.4, which assessed: (1) any antidepressant usage; (2) classes of antidepressants; and (3) individual antidepressants.
Results
Twenty studies were identified, encompassing 5,337,223 pregnancies. The odds ratio for maternal use of any antidepressant during the first trimester of pregnancy and the presence of congenital heart defects from the random effects meta-analysis was 1.28 (95% confidence interval [CI] 1.17–1.41). Significant odds ratios of 1.69 (95% CI 1.37–2.10) and 1.25 (95% CI 1.15–1.37) were reported for serotonin norepinephrine reuptake inhibitors and selective serotonin reuptake inhibitors, respectively. A non-statistically significant odds ratio of 1.02 (95% CI 0.82–1.25) was reported for the tricyclic antidepressants. Analyses of individual SSRIs produced significant odds ratios of 1.57 (95% CI 1.25–1.97), 1.36 (95% CI 1.08–1.72), and 1.29 (95% CI 1.14–1.45) for paroxetine, fluoxetine, and sertraline, respectively. The norepinephrine-dopamine-reuptake inhibitor bupropion also produced a significant odds ratio of 1.23 (95% CI 1.01–1.49).
Conclusions
The selective serotonin reuptake inhibitor and serotonin norepinephrine reuptake inhibitor classes of antidepressants pose a greater risk for causing congenital heart defects than the tricyclic antidepressants. However, this risk for individual antidepressants within each class varies, and information regarding some antidepressants is still lacking.





Similar content being viewed by others
References
Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Andersen NL, Torp-Pedersen C, et al. Prevalence of antidepressant use during pregnancy in Denmark, a nation-wide cohort study. PLoS ONE. 2013;8(4):e63034. https://doi.org/10.1371/journal.pone.0063034.
Mitchell AA, Gilboa SM, Werler MM, Kelley KE, Louik C, Hernandez-Diaz S. Medication use during pregnancy, with particular focus on prescription drugs: 1976–2008. Am J Obstet Gynecol. 2011;205(1):51.e1-8. https://doi.org/10.1016/j.ajog.2011.02.029.
Hanley GE, Mintzes B. Patterns of psychotropic medicine use in pregnancy in the United States from 2006 to 2011 among women with private insurance. BMC Pregnancy Childbirth. 2014;14:242. https://doi.org/10.1186/1471-2393-14-242.
Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1–21. https://doi.org/10.1037/a0038550.
Nevels RM, Gontkovsky ST, Williams BE. Paroxetine-the antidepressant from hell? Probably not, but caution required. Psychopharmacol Bull. 2016;46(1):77–104.
Williams M, Wooltorton E. Paroxetine (Paxil) and congenital malformations. CMAJ. 2005;173(11):1320–1. https://doi.org/10.1503/cmaj.051421.
Bérard A, Iessa N, Chaabane S, Muanda FT, Boukhris T, Zhao JP. The risk of major cardiac malformations associated with paroxetine use during the first trimester of pregnancy: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;81(4):589–604. https://doi.org/10.1111/bcp.12849.
Einarson A, Selby P, Koren G. Abrupt discontinuation of psychotropic drugs during pregnancy: fear of teratogenic risk and impact of counselling. J Psychiatry Neurosci. 2001;26(1):44–8.
Cohen LS, Altshuler LL, Harlow BL, Nonacs R, Newport DJ, Viguera AC, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499–507. https://doi.org/10.1001/jama.295.5.499.
Myles N, Newall H, Ward H, Large M. Systematic meta-analysis of individual selective serotonin reuptake inhibitor medications and congenital malformations. Aust NZ J Psychiat. 2013;47(11):1002–12. https://doi.org/10.1177/0004867413492219.
Bar-Oz B, Einarson T, Einarson A, Boskovic R, O’Brien L, Malm H, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918–26. https://doi.org/10.1016/j.clinthera.2007.05.003.
Gao SY, Wu QJ, Zhang TN, Shen ZQ, Liu CX, Xu X, et al. Fluoxetine and congenital malformations: a systematic review and meta-analysis of cohort studies. Br J Clin Pharmacol. 2017;83(10):2134–47. https://doi.org/10.1111/bcp.13321.
Riggin L, Frankel Z, Moretti M, Pupco A, Koren G. The fetal safety of fluoxetine: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2013;35(4):362–9. https://doi.org/10.1016/s1701-2163(15)30965-8.
Shen ZQ, Gao SY, Li SX, Zhang TN, Liu CX, Lv HC, et al. Sertraline use in the first trimester and risk of congenital anomalies: a systemic review and meta-analysis of cohort studies. Br J Clin Pharmacol. 2017;83(4):909–22. https://doi.org/10.1111/bcp.13161.
Grigoriadis S, VonderPorten EH, Mamisashvili L, Roerecke M, Rehm J, Dennis CL, et al. Antidepressant exposure during pregnancy and congenital malformations: is there an association? A systematic review and meta-analysis of the best evidence. J Clin Psychiat. 2013;74(4):e293-308. https://doi.org/10.4088/JCP.12r07966.
Ban L, Gibson JE, West J, Fiaschi L, Sokal R, Smeeth L, et al. Maternal depression, antidepressant prescriptions, and congenital anomaly risk in offspring: a population-based cohort study. BJOG. 2014;121(12):1471–81. https://doi.org/10.1111/1471-0528.12682.
Bérard A, Zhao JP, Sheehy O. Sertraline use during pregnancy and the risk of major malformations. Am J Obstet Gynecol. 2015;212(6):795.e1-12. https://doi.org/10.1016/j.ajog.2015.01.034.
Furu K, Kieler H, Haglund B, Engeland A, Selmer R, Stephansson O, et al. Selective serotonin reuptake inhibitors and venlafaxine in early pregnancy and risk of birth defects: population based cohort study and sibling design. BMJ. 2015;350:h1798. https://doi.org/10.1136/bmj.h1798.
Knudsen TM, Hansen AV, Garne E, Andersen AM. Increased risk of severe congenital heart defects in offspring exposed to selective serotonin-reuptake inhibitors in early pregnancy: an epidemiological study using validated EUROCAT data. BMC Pregnancy Childbirth. 2014;14:333. https://doi.org/10.1186/1471-2393-14-333.
Louik C, Kerr S, Mitchell AA. First-trimester exposure to bupropion and risk of cardiac malformations. Pharmacoepidemiol Drug Saf. 2014;23(10):1066–75. https://doi.org/10.1002/pds.3661.
Jordan S, Morris JK, Davies GI, Tucker D, Thayer DS, Luteijn JM, et al. Selective serotonin reuptake inhibitor (SSRI) antidepressants in pregnancy and congenital anomalies: analysis of linked databases in Wales, Norway and Funen, Denmark. PLoS ONE. 2016;11(12):e0165122. https://doi.org/10.1371/journal.pone.0165122.
Dolk H, McCullough N, Callaghan S, Casey F, Craig B, Given J, et al. Risk factors for congenital heart disease: the Baby Hearts Study, a population-based case-control study. PLoS ONE. 2020;15(2):e0227908. https://doi.org/10.1371/journal.pone.0227908.
Huybrechts KF, Bateman BT, Pawar A, Bessette LG, Mogun H, Levin R, et al. Maternal and fetal outcomes following exposure to duloxetine in pregnancy: cohort study. BMJ. 2020;368:m237. https://doi.org/10.1136/bmj.m237.
Hartling L, Milne A, Hamm MP, Vandermeer B, Ansari M, Tsertsvadze A, et al. Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J Clin Epidemiol. 2013;66(9):982–93. https://doi.org/10.1016/j.jclinepi.2013.03.003.
Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14(1):45. https://doi.org/10.1186/1471-2288-14-45.
Davis RL, Rubanowice D, McPhillips H, Raebel MA, Andrade SE, Smith D, et al. Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiol Drug Saf. 2007;16(10):1086–94. https://doi.org/10.1002/pds.1462.
The Cochrane Collaboration. Review Manager (RevMan). 5.4 ed. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration; 2014.
Huybrechts KF, Palmsten K, Avorn J, Cohen LS, Holmes LB, Franklin JM, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397–407. https://doi.org/10.1056/NEJMoa1312828.
Vasilakis-Scaramozza C, Aschengrau A, Cabral H, Jick SS. Antidepressant use during early pregnancy and the risk of congenital anomalies. Pharmacotherapy. 2013;33(7):693–700. https://doi.org/10.1002/phar.1211.
Margulis AV, Abou-Ali A, Strazzeri MM, Ding Y, Kuyateh F, Frimpong EY, et al. Use of selective serotonin reuptake inhibitors in pregnancy and cardiac malformations: a propensity-score matched cohort in CPRD. Pharmacoepidemiol Drug Saf. 2013;22(9):942–51. https://doi.org/10.1002/pds.3462.
Nordeng H, van Gelder MM, Spigset O, Koren G, Einarson A, Eberhard-Gran M. Pregnancy outcome after exposure to antidepressants and the role of maternal depression: results from the Norwegian Mother and Child Cohort Study. J Clin Psychopharmacol. 2012;32(2):186–94. https://doi.org/10.1097/JCP.0b013e3182490eaf.
Colvin L, Slack-Smith L, Stanley FJ, Bower C. Dispensing patterns and pregnancy outcomes for women dispensed selective serotonin reuptake inhibitors in pregnancy. Birth Defects Res A Clin Mol Teratol. 2011;91(3):142–52. https://doi.org/10.1002/bdra.20773.
Merlob P, Birk E, Sirota L, Linder N, Berant M, Stahl B, et al. Are selective serotonin reuptake inhibitors cardiac teratogens? Echocardiographic screening of newborns with persistent heart murmur. Birth Defects Res A Clin Mol Teratol. 2009;85(10):837–41. https://doi.org/10.1002/bdra.20615.
Oberlander TF, Warburton W, Misri S, Riggs W, Aghajanian J, Hertzman C. Major congenital malformations following prenatal exposure to serotonin reuptake inhibitors and benzodiazepines using population-based health data. Birth Defects Res B Dev Reprod Toxicol. 2008;83(1):68–76. https://doi.org/10.1002/bdrb.20144.
Diav-Citrin O, Shechtman S, Weinbaum D, Wajnberg R, Avgil M, Di Gianantonio E, et al. Paroxetine and fluoxetine in pregnancy: a prospective, multicentre, controlled, observational study. Br J Clin Pharmacol. 2008;66(5):695–705. https://doi.org/10.1111/j.1365-2125.2008.03261.x.
Kulin NA, Pastuszak A, Sage SR, Schick-Boschetto B, Spivey G, Feldkamp M, et al. Pregnancy outcome following maternal use of the new selective serotonin reuptake inhibitors: a prospective controlled multicenter study. JAMA. 1998;279(8):609–10. https://doi.org/10.1001/jama.279.8.609.
Polen KN, Rasmussen SA, Riehle-Colarusso T, Reefhuis J. Association between reported venlafaxine use in early pregnancy and birth defects, national birth defects prevention study, 1997–2007. Birth Defects Res A Clin Mol Teratol. 2013;97(1):28–35. https://doi.org/10.1002/bdra.23096.
de Jonge L, van der Woude ZPA, Bos HJ, de Berg JDLT, Bakker MK. Identifying associations between maternal medication use and birth defects using a case-population approach: an exploratory study on signal detection. Drug Saf. 2013;36(11):1069–78. https://doi.org/10.1007/s40264-013-0082-2.
Alwan S, Reefhuis J, Botto LD, Rasmussen SA, Correa A, Friedman JM. Maternal use of bupropion and risk for congenital heart defects. Am J Obstet Gynecol. 2010;203(1):52.e1-6. https://doi.org/10.1016/j.ajog.2010.02.015.
Kornum JB, Nielsen RB, Pedersen L, Mortensen PB, Norgaard M. Use of selective serotonin-reuptake inhibitors during early pregnancy and risk of congenital malformations: updated analysis. Clin Epidemiol. 2010;2(1):29–36.
Källén BA, Otterblad OP. Maternal use of selective serotonin re-uptake inhibitors in early pregnancy and infant congenital malformations. Birth Defects Res A Clin Mol Teratol. 2007;79(4):301–8. https://doi.org/10.1002/bdra.20327.
Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Jensen JK, Afzal S, et al. Exposure to selective serotonin reuptake inhibitors and the risk of congenital malformations: a nationwide cohort study. BMJ Open. 2012;2(3):e001148. https://doi.org/10.1136/bmjopen-2012-001148.
Malm H, Artama M, Gissler M, Ritvanen A. Selective serotonin reuptake inhibitors and risk for major congenital anomalies. Obstet Gynecol. 2011;118(1):111–20. https://doi.org/10.1097/AOG.0b013e318220edcc.
Lambert O, Bourin M. SNRIs: mechanism of action and clinical features. Expert Rev Neurother. 2002;2(6):849–58. https://doi.org/10.1586/14737175.2.6.849.
Sangkuhl K, Klein TE, Altman RB. Selective serotonin reuptake inhibitors pathway. Pharmacogenet Genom. 2009;19(11):907–9. https://doi.org/10.1097/FPC.0b013e32833132cb.
Gadzhanova S, Roughead E. Use of prescription medicines in Australian women of child-bearing age. BMC Pharmacol Toxicol. 2015;16:33. https://doi.org/10.1186/s40360-015-0033-x.
Mann CJ. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emerg Med J. 2003;20(1):54. https://doi.org/10.1136/emj.20.1.54.
Norvell DC. Study types and bias: don’t judge a study by the abstract’s conclusion alone. Evid Based Spine Care J. 2010;1(2):7–10. https://doi.org/10.1055/s-0028-1100908.
Narchi H, Kulaylat N. Heart disease in infants of diabetic mothers. Images Paediatr Cardiol. 2000;2(2):17–23.
Zhang Y-F, Zeng X-L, Zhao E-F, Lu H-W. Diagnostic value of fetal echocardiography for congenital heart disease: a systematic review and meta-analysis. Medicine. 2015;94(42):e1759. https://doi.org/10.1097/MD.0000000000001759.
Davis AP, Grondin CJ, Johnson RJ, Sciaky D, McMorran R, Wiegers J, et al. The comparative toxicogenomics database: update 2019. Nucleic Acids Res. 2019;47(D1):D948–54. https://doi.org/10.1093/nar/gky868.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this work.
Conflicts of interest/competing interests
Courtney De Vries, Svetla Gadzhanova, Matthew J. Sykes, Michael Ward, and Elizabeth Roughead have no conflicts of interest that are directly relevant to the content of this article and declare no support from any organization for the submitted work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
CDV has the right to grant on behalf of all authors and does grant on behalf of all authors, a worldwide licence to the publishers and its licensees in perpetuity, in all forms, formats, and media.
Availability of data and material
All data generated or analyzed during this study are included in this published article (and its Electronic Supplementary Material).
Code availability
Not applicable.
Authors’ contributions
ER and CDV designed the study. CDV performed the literature search. CDV and SG extracted data from the identified articles. CDV conducted the meta-analyses and drafted the manuscript. All authors reviewed the manuscript, contributed to its revision, and approved the final version submitted.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Vries, C., Gadzhanova, S., Sykes, M.J. et al. A Systematic Review and Meta-Analysis Considering the Risk for Congenital Heart Defects of Antidepressant Classes and Individual Antidepressants. Drug Saf 44, 291–312 (2021). https://doi.org/10.1007/s40264-020-01027-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-020-01027-x