Abstract
Background
Biologic agents were initially introduced as treatment for rheumatoid arthritis (RA) but have since been used for other medical conditions. As new biologics become increasingly widespread in treatment regimens, it is important to understand their safety and utilization in the post-marketing context.
Purpose
The aim of this study was to investigate long-term prescribing patterns and the safety of biologics in real clinical settings in Hong Kong.
Methods
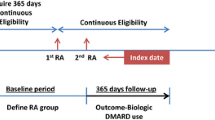
This was a population-based drug utilization study in Hong Kong using a territory-wide electronic medical database Clinical Data Analysis and Reporting System (CDARS). Patients who received biologic treatments from 2001 to 2015 were identified and their corresponding demographic and clinical details retrieved from CDARS. The annual prevalence of biologic prescriptions, the long-term retention rates and incidence rates of infections associated with biologic treatments were evaluated.
Results
A total of 30,298 patients (male: 44%) prescribed biologic treatments were identified from CDARS from 2001 to 2015. The annual prevalence of biologic prescriptions increased from 0.1 to 16.1 per 100 persons for both sexes. Infliximab had the highest first-year retention rate of 95.6% among all biologics and continuously attained the highest retention rate from second to fifth year. The overall incidence rate of serious infections was less than five per 100 person-years. Specifically, the incidence rates of tuberculosis, upper and lower respiratory infections and herpes zoster were 0.52, 3.24, 4.99 and 1.01 per 100 person-years, respectively.
Conclusion
This population-based study revealed an increasing prevalence of biologic prescribing. Results from the study described the long-term retention rates and incidence rates of serious infections of biologic treatments for all indications, and confirmed the safety of biologic treatments. Since this study provides an overview of all biologic utilization, further studies on cost effectiveness, safety and compliance of treatment in different patient groups are still warranted.






Similar content being viewed by others
References
FDA US. What are “biologics” questions and answers. US food and drug administration. 2018. https://www.fda.gov/aboutfda/centersoffices/officeofmedicalproductsandtobacco/cber/ucm133077.htm. Accessed 02 June 2018.
Morrow T, Felcone LH. Defining the difference: what makes biologics unique. Biotechnol Healthc. 2004;1(4):24–9.
Rosman Z, Shoenfeld Y, Zandman-Goddard G. Biologic therapy for autoimmune diseases: an update. BMC Med. 2013;11(1):88. https://doi.org/10.1186/1741-7015-11-88.
Raychaudhuri SP, Raychaudhuri SK. Biologics: target-specific treatment of systemic and cutaneous autoimmune diseases. Indian J Dermatol. 2009;54(2):100–9. https://doi.org/10.4103/0019-5154.53175.
Sebba A. Tocilizumab: the first interleukin-6-receptor inhibitor. Am J Health Syst Pharm. 2008;65(15):1413–8. https://doi.org/10.2146/ajhp070449.
Rozenblit M, Lebwohl M. New biologics for psoriasis and psoriatic arthritis. Dermatol Ther. 2009;22(1):56–60. https://doi.org/10.1111/j.1529-8019.2008.01216.x.
Tobin AM, Kirby B. TNF alpha inhibitors in the treatment of psoriasis and psoriatic arthritis. Biodrugs. 2005;19(1):47–57.
Gulyas K, Bodnar N, Nagy Z, Szamosi S, Horvath A, Vancsa A, et al. Real-life experience with switching TNF-alpha inhibitors in ankylosing spondylitis. Eur J Health Econ. 2014;15(Suppl 1):S93–100. https://doi.org/10.1007/s10198-014-0598-0.
Behm BW, Bickston SJ. Tumor necrosis factor-alpha antibody for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2008;1:CD006893. https://doi.org/10.1002/14651858.cd006893.
Sandborn WJ, Gasink C, Gao L-L, Blank MA, Johanns J, Guzzo C, et al. Ustekinumab induction and maintenance therapy in refractory Crohn’s disease. N Engl J Med. 2012;367(16):1519–28. https://doi.org/10.1056/NEJMoa1203572.
Carethers JM. Systemic treatment of advanced colorectal cancer: tailoring therapy to the tumor. Therap Adv Gastroenterol. 2008;1(1):33–42. https://doi.org/10.1177/1756283X08093607.
Crawford S. Is it time for a new paradigm for systemic cancer treatment? Lessons from a century of cancer chemotherapy. Front Pharmacol. 2013;4:68. https://doi.org/10.3389/fphar.2013.00068.
Brennan DC, Daller JA, Lake KD, Cibrik D, Del Castillo D. Rabbit antithymocyte globulin versus basiliximab in renal transplantation. N Engl J Med. 2006;355(19):1967–77.
Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364(20):1897–908. https://doi.org/10.1056/NEJMoa1102673.
McClung MR, Lewiecki EM, Cohen SB, Bolognese MA, Woodson GC, Moffett AH, et al. Denosumab in postmenopausal women with low bone mineral density. N Engl J Med. 2006;354(8):821–31. https://doi.org/10.1056/NEJMoa044459.
Group I-RS. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics. 1998;102(3):531–7.
Martin-Mola E, Balsa A. Infectious complications of biologic agents. Rheum Dis Clin North Am. 2009;35(1):183–99. https://doi.org/10.1016/j.rdc.2009.03.009.
Mohan AK, Cote TR, Siegel JN, Braun MM. Infectious complications of biologic treatments of rheumatoid arthritis. Curr Opin Rheumatol. 2003;15(3):179–84.
Sathish JG, Sethu S, Bielsky MC, de Haan L, French NS, Govindappa K, et al. Challenges and approaches for the development of safer immunomodulatory biologics. Nat Rev Drug Discov. 2013;12(4):306–24. https://doi.org/10.1038/nrd3974.
Bresnihan B, Cunnane GJR. Infection complications associated with the use of biologic agents. Rheum Dis Clin North Am. 2003;29(1):185–202.
National Institute for Health and Clinical Excellence. Rheumatoid arthritis: the management of rheumatoid arthritis in adults. NICE Clinical Guideline 79. 2009. http://www.nice.org.uk/nicemedia/pdf/CG79NICEGuideline.pdf. Accessed 11 Dec 2012.
Listing J, Strangfeld A, Kary S, Rau R, von Hinueber U, Stoyanova-Scholz M, et al. Infections in patients with rheumatoid arthritis treated with biologic agents. Arthritis Rheum. 2005;52(11):3403–12. https://doi.org/10.1002/art.21386.
Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V. Anti-tnf antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006;295(19):2275–85. https://doi.org/10.1001/jama.295.19.2275.
Lai EC, Man KK, Chaiyakunapruk N, Cheng CL, Chien HC, Chui CS, et al. brief report: databases in the asia-pacific region: the potential for a distributed network approach. Epidemiology. 2015;26(6):815–20. https://doi.org/10.1097/ede.0000000000000325.
Man KKC, Chan EW, Ip P, Coghill D, Simonoff E, Chan PKL, et al. Prenatal antidepressant use and risk of attention-deficit/hyperactivity disorder in offspring: population based cohort study. BMJ. 2017;357:j2350. https://doi.org/10.1136/bmj.j2350.
Man KKC, Coghill D, Chan EW, Lau WCY, Hollis C, Liddle E, et al. Association of risk of suicide attempts with methylphenidate treatment. JAMA Psychiatry. 2017;74(10):1048–55. https://doi.org/10.1001/jamapsychiatry.2017.2183.
Lau WC, Chan EW, Cheung C-L, Sing CW, Man KK, Lip GY, et al. Association between dabigatran vs warfarin and risk of osteoporotic fractures among patients with nonvalvular atrial fibrillation. JAMA. 2017;317(11):1151–8.
Man KKC, Ip P, Hsia Y, Chan EW, Chui CSL, Lam MPS, et al. ADHD drug prescribing trend is increasing among children and adolescents in Hong Kong. J Atten Disord. 2017;21(14):1161–8. https://doi.org/10.1177/1087054714536047.
Raman SR, Man KKC, Bahmanyar S, Berard A, Bilder S, Boukhris T, et al. Trends in attention-deficit hyperactivity disorder medication use: a retrospective observational study using population-based databases. Lancet Psychiatry. 2018;5(10):824–35. https://doi.org/10.1016/s2215-0366(18)30293-1.
Wong ICK. New antiepileptic drugs—study suggests that under a quarter of patients will still be taking the new drugs after six years. BMJ. 1997;314(7080):603–4.
Wong ICK, Chadwick DW, Fenwick PBC, Mawer GE, Sander JWAS. The long-term use of gabapentin, lamotrigine, and vigabatrin in patients with chronic epilepsy. Epilepsia. 1999;40(10):1439–45. https://doi.org/10.1111/j.1528-1157.1999.tb02017.x.
Wong ICK. New antiepileptic drugs. Study suggests that under a quarter of patients will still be taking the new drugs after six years. BMJ. 1997;314(7080):603–4.
Lhatoo SD, Wong IC, Sander JW. Prognostic factors affecting long-term retention of topiramate in patients with chronic epilepsy. Epilepsia. 2000;41(3):338–41.
Beal GM, Bohlen JM. The diffusion process. Agricultural experiment station. Ames: Iowa State College; 1957.
Simard JF, Arkema EV, Sundstrom A, Geborek P, Saxne T, Baecklund E, et al. Ten years with biologics: to whom do data on effectiveness and safety apply? Rheumatology (Oxford). 2011;50(1):204–13. https://doi.org/10.1093/rheumatology/keq326.
Bridges SL. National institute of arthritis and musculoskeletal and skin diseases. Arthritis Res Ther. 2000;2(1):0003.
Wing-ho Shiu TKW, Chao DVK. A review on the diagnosis and management of rheumatoid arthritis in general practice. HK Pract. 2018;40:61–72.
Ip TP, Cheung SK, Cheung TC, Choi TC, Chow SL, Ho YY, et al. The osteoporosis Society of Hong Kong (OSHK): 2013 OSHK guideline for clinical management of postmenopausal osteoporosis in Hong Kong. Hong Kong Med J. 2013;19(Suppl 2):1–40.
Frazier-Mironer A, Dougados M, Mariette X, Cantagrel A, Deschamps V, Flipo RM, et al. Retention rates of adalimumab, etanercept and infliximab as first and second-line biotherapy in patients with rheumatoid arthritis in daily practice. Jt Bone Spine. 2014;81(4):352–9.
Favalli EG, Pontikaki I, Becciolini A, Biggioggero M, Ughi N, Romano M, et al. Real-life 10-year retention rate of first-line anti-TNF drugs for inflammatory arthritides in adult- and juvenile-onset populations: similarities and differences. Clin Rheumatol. 2017;36(8):1747–55. https://doi.org/10.1007/s10067-017-3712-8.
Hetland ML, Christensen IJ, Tarp U, Dreyer L, Hansen A, Hansen IT, et al. Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: results from eight years of surveillance of clinical practice in the nationwide Danish DANBIO registry. Arthritis Rheum. 2010;62(1):22–32. https://doi.org/10.1002/art.27227.
Waugh AW, Garg S, Matic K, Gramlich L, Wong C, Sadowski DC, et al. Maintenance of clinical benefit in Crohn’s disease patients after discontinuation of infliximab: long-term follow-up of a single centre cohort. Aliment Pharmacol Ther. 2010;32(9):1129–34. https://doi.org/10.1111/j.1365-2036.2010.04446.x.
Van Assche G, Vermeire S, Ballet V, Gabriels F, Noman M, D’Haens G, et al. Switch to adalimumab in patients with Crohn’s disease controlled by maintenance infliximab: prospective randomised SWITCH trial. Gut. 2012;61(2):229–34. https://doi.org/10.1136/gutjnl-2011-300755.
Wan R, Mok Chi C. The Hong Kong Society of Rheumatology Biologics Registry: updated report (May 2018). Hong Kong Bull Rheum Dis. 2018;18(1):30. https://doi.org/10.2478/hkbrd-2018-0006.
Mok CC, Tam LS, Chan TH, Lee GKW, Li EKM, Hong Kong Society of R. Management of rheumatoid arthritis: consensus recommendations from the Hong Kong Society of Rheumatology. Clin Rheumatol. 2011;30(3):303–12. https://doi.org/10.1007/s10067-010-1596-y.
Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American College of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2016;68(1):1–26.
Scheinberg M, Goldenberg J, Feldman DP, Nobrega JL. Retrospective study evaluating dose standards for infliximab in patients with rheumatoid arthritis at Hospital Israelita Albert Einstein, Sao Paulo. Brazil. Clin Rheumatol. 2008;27(8):1049–52. https://doi.org/10.1007/s10067-008-0908-y.
Leung GM, Tin KY, O’Donnell O. Redistribution or horizontal equity in Hong Kong’s mixed public-private health system: a policy conundrum. Health Econ. 2009;18(1):37–54. https://doi.org/10.1002/hec.1342.
Acknowledgements
The authors would like to thank Ms Lisa Lam for copyediting the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by Pfizer Corporation Hong Kong Limited [project tracking number: W1198308].
Ethics Statement
The study protocol was approved by the Hospital Authority Hong Kong West Cluster and University of Hong Kong Institutional Review Board (UW14-602).
Conflict of Interest
Xue Li has received research funding from the Food and Health Bureau of the Government of Hong Kong. Kenneth Man received the CW Maplethorpe Fellowship and personal fees from IQVIA Holdings, Inc., unrelated to this work. Esther Chan has received research funding from Wellcome Trust, United Kingdom; National Natural Science Fund of China, China; The Hong Kong Research Grants Council; The Research Fund Secretariat of the Food and Health Bureau; Narcotics Division of the Security Bureau of The Government of the Hong Kong Special Administrative Region; and Bristol-Myers Squibb, Pfizer, Bayer and Janssen, a Division of Johnson & Johnson, for work unrelated to this study. Ian Wong has received grants from the Research Grants Council (RGC, Hong Kong), Innovative Medicines Initiative (IMI), Shire, Janssen-Cilag, Eli-Lily, Pfizer, Bayer, and the European Union FP7 program, outside the submitted work. Ian Wong is a member of the National Institute for Health and Clinical Excellence (NICE) ADHD Guideline Group, the British Association for Psychopharmacology ADHD guideline group, and advisor to Shire. Mengqin Ge and Celine Chui declare no conflict of interest.
Additional information
Mengqin Ge and Kenneth K. Man are co-first author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ge, M., Man, K.K., Chui, C.S. et al. Prevalence, Safety and Long-Term Retention Rates of Biologics in Hong Kong from 2001 to 2015. Drug Saf 42, 1091–1102 (2019). https://doi.org/10.1007/s40264-019-00844-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-019-00844-z