Abstract
Background
Early prediction and accurate characterization of risk for serious liver injury associated with newly marketed drugs remains an important challenge for clinicians, the pharmaceutical industry, and regulators. To date, a biomarker that specifically indicates exposure to a drug as the etiologic cause of liver injury has not been identified.
Objectives
Using cumulative proportional reporting ratios (PRRs), we investigated ‘real-time’ profiles of a set of pharmaceuticals, over the first 3 years of US marketing, for the signaling of clinically serious drug-induced liver injury (DILI) in a large spontaneous-reporting database.
Methods
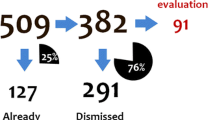
Using report counts of hepatic failure or clinically serious liver injury obtained from the FDA Adverse Events Reporting System (FAERS) database, PRRs of adverse drug event terms were calculated by division of counts of domestic reports of these events by counts of all serious adverse events for each of 13 selected drugs associated with a broad range of hepatotoxic risk (including three linked to only rare instances of clinically apparent liver injury) with reference to all other drugs in the database. Drug-specific cumulative PRRs were measured at successive intervals (calendar quarters) using cumulative tallies of FAERS reports to generate time-based profiles over the initial 3 years of US marketing.
Results
In the set of drugs analyzed, those with no known hepatotoxic risk demonstrated time-based cumulative PRR profiles that approximate the background rates of hepatic failure and serious liver injury reported in the entire FAERS database. In contrast, those that were removed from marketing or subjected to marketing restrictions due to their potential to cause liver injury were associated with profiles of rapidly rising cumulative PRRs that were greater than 5 within the first 10 million domestic prescriptions or the first four quarters of US marketing. The systematic tracking and identification of rising PRRs for DILI associated with newly marketed pharmaceutical and biological agents is a valuable tool for identification of safety signals within the FAERS database.
Limitations
Disproportionality profiling of spontaneous reports in FAERS (e.g., cumulative PRR measurements), which signals an association between a recently marketed drug and liver injury, is not a method to quantitatively measure drug-related risk. Regulatory actions in response to emerging drug safety concerns often depend on an accurate assessment of risks using multiple sources of data and the consideration of overall benefits and risks of the agent. Causality must be determined through analysis of individual cases to exclude other etiologies of liver injury.
Conclusion
The FAERS database can be used to advance empiric hepatotoxicity time-trending reporting levels for newly marketed agents in order to rapidly identify recently launched potential hepatotoxic agents and initiate further evaluation.




Similar content being viewed by others
Notes
MedDRA® is an internationally recognized adverse event coding system used by regulatory authorities and the biopharmaceutical industry. MedDRA® was developed by the International Conference on Harmonisation (ICH) and is managed by the Maintenance and Support Services Organization (MSSO)/International Federation of Pharmaceutical Manufacturers and Associations (IFPMA).
Reference
Temple RJ, Himmel MH. Safety of newly approved drugs: implications for prescribing. JAMA. 2002;287(17):2273–5.
Lucena MI, García-Cortés M, Cueto R, et al. Assessment of drug-induced liver injury in clinical practice. Fundam Clin Pharmacol. 2008;22(2):141–58.
Benichou C. Criteria of drug-induced liver disorders. Report of an international consensus meeting. J Hepatol. 1990;11:272–6.
Andrade RJ, Camargo R, Lucena MI, González-Grande R. Causality assessment in drug-induced hepatotoxicity. Expert Opin Drug Saf. 2004;3(4):329–44.
Uetrecht JP. New concepts in immunology relevant to idiosyncratic drug reactions: the “danger hypothesis” and innate immune system. Chem Res Toxicol. 1999;12:387–95.
Gupta NK, Lewis JH. Review article: the use of potentially hepatotoxic drugs in patients with liver disease. Aliment Pharmacol Ther. 2008;28:1021–41.
Gunawan BK, Kaplowitz N. Mechanisms of drug-induced liver disease. Clin Liver Dis. 2007;11(3):459–75.
Wallace KB, Starkov AA. Mitochondrial targets of drug toxicity. Annu Rev Pharmacol Toxicol. 2000;40:353–88.
Boelsterli UA, Lim PL. Mitochondrial abnormalities—a link to idiosyncratic drug hepatotoxicity? Toxicol Appl Pharmacol. 2007;220:92–107.
Jones DP, Lemasters JJ, Han D, Boelsterli UA, Kaplowitz N. Mechanisms of pathogenesis in drug hepatotoxicity putting the stress on mitochondria. Mol Interv. 2010;10(2):98–111.
Senior JR, Avigan M. Detection of hepatotoxicity during drug development: practical problems and regulatory measures. In: Arroyo V, Andrade R, editors. International hepatology updates. Barcelona: Permanyer Publications; 2007. p. 147–66.
Watkins PB, Seligman PJ, Pears JS, Avigan MI, Senior JR. Using controlled clinical trials to learn more about acute drug-induced liver injury. Hepatology. 2008;48(5):1680–9.
Fontana RJ, Seeff LB, Andrade RJ, Björnsson E, Day CP, Serrano J, Hoofnagle JH. Standardization of nomenclature and causality assessment in drug-induced liver injury: summary of a clinical research workshop. Hepatology. 2010;52(2):730–42.
Begaud B, Martin K, Haramburu F, Moore N. Rates of spontaneous reporting of adverse drug reactions in France [letter]. JAMA. 2002;288(13):1588.
Goldman SA. Limitations and strengths of spontaneous reports data. Clin Ther. 1998;20 Suppl C:C40–4.
Sachs RM, Bortnichak EA. An evaluation of spontaneous adverse drug reaction monitoring systems. Am J Med. 1986;81(5B):49–55.
Brinker A, Beitz J. Use of a spontaneous adverse drug events database for identification of unanticipated drug benefits. Clin Pharmacol Ther. 2002;71(1):99–102.
Evans SJ, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf. 2001;10(6):483–6.
Friedman MA, Woodcock J, Lumpkin MM, Shuren JE, Hass AE, Thompson LJ. The safety of newly approved medicines: do recent market removals mean there is a problem? JAMA. 1999;281(18):1728–34.
Moses PL, Schroeder B, Alkhatib O, Ferrentino N, Suppan T, Lidofsky SD. Severe hepatotoxicity associated with bromfenac. Am J Gastroenterol. 1999;94(5):1393–6.
Hunter EB, Johnston PE, Tanner G, Pinson CW, Awad JA. Bromfenac (Duract)-associated hepatic failure requiring liver transplantation. Am J Gastroenterol. 1999;94(8):2299–301.
Rabkin JM, Smith MJ, Orloff SL, Corless CL, Stenzel P, Olyaei AJ. Fatal fulminant hepatitis associated with bromfenac use. Ann Pharmacother. 1999;33(9):945–7.
Fontana RJ, McCashland TM, Benner KG, for the Acute Liver Failure Study Group, et al. Acute liver failure associated with prolonged use of bromfenac leading to liver transplantation. Liver Transpl Surg. 1999;5(6):480–4.
McAdams M, Staffa J, Dal Pan G. Estimating the extent of reporting to FDA: a case study of statin-associated rhabdomyolysis. Pharmacoepidemiol Drug Saf. 2008;17(3):229–39.
Pariente A, Gregoire F, Fourrier-Reglat A, Haramburu F, Moore N. Impact of safety alerts on measures of disproportionality in spontaneous reporting databases: the notoriety bias. Drug Saf. 2007;30(10):891–8.
Lumpkin MM. Troglitazone: presentation to advisory committee. Presentation before the Metabolic and Endocrine Advisory Committee; 2000. Slide presentation http://www.fda.gov/ohrms/dockets/ac/00/slides/3615s1a.ppt. Accessed 10 Oct 2012.
Murphy EJ, Davern TJ, Shakil AO, for the Acute Liver Failure Study Group, et al. Troglitazone-induced fulminant hepatic failure. Dig Dis Sci. 2000;45(3):549–53.
Graham DJ, Green L, Senior JR, Nourjah P. Troglitazone-induced liver failure: a case study. Am J Med. 2003;114(4):299–306.
Floyd JS, Barbehenn E, Lurie P, Wolfe SM. Case series of liver failure associated with rosiglitazone and pioglitazone. Pharmacoepidemiol Drug Saf. 2009;18(12):1238–43.
FDA Public Health Advisory. Postmarketing Drug Safety Information: trovafloxacin. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ucm053104.htm. Accessed 10 Oct 2012.
Clay KD, Hanson JS, Pope SD, Rissmiller RW, Purdum PP 3rd, Banks PM. Brief communication: severe hepatotoxicity of telithromycin: three case reports and literature review. Ann Intern Med. 2006;144(6):415–20.
Brinker AD, Wassel RT, Lyndly J, Serrano J, Avigan M, Lee WM, Seeff LB. Telithromycin-associated hepatotoxicity: clinical spectrum and causality assessment of 42 cases. Hepatology. 2009;49(1):250–7.
FDA post-marketing safety information on telithromycin [posted February 12, 2007]. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm107824.htm. Accessed 8 Oct 2012.
Orman ES, Conjeevaram HS, Vuppalanchi R, for the DILIN Research Group, et al. Clinical and histopathologic features of fluoroquinolone-induced liver injury. Clin Gastroenterol Hepatol. 2011;9(6):517–23.
Brinker A. Telithromycin-associated hepatotoxicity. Presentation before the Anti-Infective Drugs Advisory Committee in Joint Session with the Drug Safety and Risk Management Advisory Committee, December 14, 2006. Slide presentation: http://www.fda.gov/ohrms/dockets/AC/06/slides/2006-4266s1-01-07-FDA-Brinker.ppt. Accessed 8 Oct 2012.
Deshpande G, Gogolak V, Smith SW. Data mining in drug safety: review of published threshold criteria for defining signals of disproportionate reporting. Pharm Med. 2010;24(1):37–43.
Hauben M, Madigan D, Gerrits CM, Walsh L, Van Puijenbroek EP. The role of data mining in pharmacovigilance. Expert Opin Drug Saf. 2005;4(5):929–48.
McAdams MA, Governale LA, Swartz L, Hammad TA, Dal Pan GJ. Identifying patterns of adverse event reporting for four members of the angiotensin II receptor blockers class of drugs: revisiting the Weber effect. Pharmacoepidemiol Drug Saf. 2008;17(9):882–9.
Taubes G. Epidemiology faces its limits. Science. 1995;269(5221):164–9.
Livertox: clinical and research information on drug-induced liver injury. Liver Disease Research Branch of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the Division of Specialized Information Services of the National Library of Medicine (NLM), National Institutes of Health. http://www.livertox.nih.gov/index.html. Accessed 12 Mar 2013.
Bjornsson E. Drug-induced liver injury: Hy’s rule revisited. Clin Pharmacol Ther. 2006;79:521–8.
Senior JR. Drug hepatotoxicity from a regulatory perspective. Clin Liver Dis. 2007;11(3):507–24.
Weaver J, Grenade LL, Kwon H, Avigan M. Finding, evaluating, and managing drug-related risks: approaches taken by the US Food and Drug Administration (FDA). Dermatol Ther. 2009;22(3):204–15.
Weaver J, Willy M, Avigan M. Informatic tools and approaches in postmarketing pharmacovigilance used by FDA. AAPS J. 2008;10(1):35–41.
Begaud B, Moride Y, Tubert-Bitter P, Chaslerie A, Haramburu F. False-positives in spontaneous reporting: should we worry about them? Br J Clin Pharmacol. 1994;38(5):401–4.
Suzuki A, Andrade RJ, Bjornsson E, Lucena MI, Lee WM, et al. Drugs associated with hepatotoxicity and their reporting frequency of liver adverse events in VigiBase: unified list based on international collaborative work. Drug Saf. 2010;33(6):503–22.
Acknowledgments
The authors wish to thank Dr. Gerald Dal Pan for his thoughtful critique of the manuscript.
Financial Support
The authors list no grants, direct financial support, or financial interests in the presentation of these data.
Conflict of Interest
Allen Brinker, Joseph Tonning, Jenna Lyndly, David Moeny, Jonathan Levine, and Mark Avigan are currently employed at the US Food and Drug Administration and have no conflicts of interest to declare that are directly relevant to the content of this study.
Disclaimer
The views expressed are those of the authors and do not necessarily represent the position of, nor imply endorsement from, the US Food and Drug Administration or the US Government.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brinker, A.D., Lyndly, J., Tonning, J. et al. Profiling Cumulative Proportional Reporting Ratios of Drug-Induced Liver Injury in the FDA Adverse Event Reporting System (FAERS) Database. Drug Saf 36, 1169–1178 (2013). https://doi.org/10.1007/s40264-013-0116-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0116-9