Abstract
Background
Both antidepressants and non-steroidal anti-inflammatory drugs (NSAIDs) have been reported to affect platelet aggregation, blood pressure and heart rate. Despite the high prevalence of the combined use of antidepressants and NSAIDs, there is limited evidence on the potential risk of major adverse cardiovascular events (MACE) associated with their use.
Objective
The objective of this study was to assess the association between concomitant antidepressant and NSAID use and MACE.
Methods
We conducted a retrospective cohort study using South Korea’s nationwide healthcare database. The study cohort was defined as those with new prescriptions for antidepressants and NSAIDs between 2004 and 2015. Exposure was assessed as time varying into four discrete periods: non-use, antidepressant use, NSAID use and concomitant use. Our primary outcome was MACE, a composite of haemorrhagic and thromboembolic events; secondary outcomes were the individual events of MACE. A multivariable Cox proportional hazards model was used to estimate hazards ratios with 95% confidence intervals. We also performed subgroup analyses by class of antidepressant/type of NSAIDs, age and sex.
Results
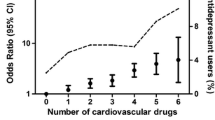
From 240,982 patients, 235,080, 4393 and 1509 patients were users of NSAIDs, antidepressants or both drugs at cohort entry, respectively. The cohort generated 2.1 million person-years of follow-up with 22,453 events of MACE (incidence rate 1.07 per 100 person-years). Compared with non-use, concomitant use (hazard ratio 1.13, 95% confidence interval 1.01–1.26) and NSAID-only use (1.05, 1.001–1.10) were positively associated with MACE, while antidepressant-only use showed a negative association (0.91, 0.83–0.99). Concomitant use increased the individual risk of haemorrhagic stroke (1.46, 1.06–2.00), ischaemic stroke (1.22, 1.07–1.38) and heart failure (1.19, 1.02–1.38), but showed a protective effect on cardiovascular deaths (0.36, 0.21–0.62). Of the six possible combinations of antidepressants and NSAIDs by their classes, only concomitant use of tricyclic antidepressants and non-selective NSAIDs was positively associated with MACE (1.26, 1.09–1.47). The risk of MACE remained elevated with concomitant use among those aged ≥ 45 years (1.14, 1.01–1.29) and male patients (1.19, 1.01–1.42).
Conclusions
Concomitant use of antidepressants and NSAIDs moderately elevated the risk of MACE, of which the observed risk appears to be driven by the concomitant use of tricyclic antidepressants and non-selective NSAIDs. Thus, healthcare providers should take precaution when co-prescribing these drugs, weighing the potential benefits and risks associated with their use.





Similar content being viewed by others
References
Biffi A, Scotti L, Corrao G. Use of antidepressants and the risk of cardiovascular and cerebrovascular disease: a meta-analysis of observational studies. Eur J Clin Pharmacol. 2017;73(4):487–97.
Pepine C, Gurbel P. Cardiovascular safety of NSAIDs: additional insights after PRECISION and point of view. Clin Cardiol. 2017;40(12):1352–6.
Gunter B, Butler K, Wallace R, Smith S, Harirforoosh S. Non-steroidal anti-inflammatory drug-induced cardiovascular adverse events: a meta-analysis. J Clin Pharm Ther. 2017;42(1):27–38.
Sondergaard K, Weeke P, Wissenberg M, Olsen A-M, Fosbol E, Lippert F, et al. Non-steroidal anti-inflammatory drug use is associated with increased risk of out-of-hospital cardiac arrest: a nationwide case-time-control study. Eur Heart J Cardiovasc Pharmacother. 2017;3(2):100–7.
Shin J, Park M, Lee S, Choi S, Kim M, Choi N, et al. Risk of intracranial haemorrhage in antidepressant users with concurrent use of non-steroidal anti-inflammatory drugs: nationwide propensity score matched study. BMJ. 2015;14(351):h3517.
Moore N, Pollack C, Butkerait P. Adverse drug reactions and drug-drug interactions with over-the-counter NSAIDs. Ther Clin Risk Manag. 2015;11:1061–75.
Schellander R, Donnerer J. Antidepressants: clinically relevant drug interactions to be considered. Pharmacology. 2010;86(4):203–15.
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–8.
Roth G, Johnson C, Abajobir A, Abd-Allah F, Abera S, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25.
Morriss R. Antidepressants are associated with hospital admitted intracranial bleeds in people taking other medication associated with bleeding. Evid Based Ment Health. 2016;19(1):24.
Mercer SW, Payne RA, Nicholl BI, Morrison J. Risk of intracranial haemorrhage linked to co-treatment with antidepressants and NSAIDs. BMJ. 2015;14(351):h3745.
Coupland C, Hill T, Morriss R, Moore M, Arthur A, Hippisley-Cox J. Antidepressant use and risk of cardiovascular outcomes in people aged 20 to 64: cohort study using primary care database. BMJ. 2016;352:i1350.
Choi N, Park B, Jeong S, Yu K, Yoon B. Nonaspirin nonsteroidal anti-inflammatory drugs and hemorrhagic stroke risk: the Acute Brain Bleeding Analysis study. Stroke. 2008;39(3):845–9.
Renoux C, Vahey S, Dell'Aniello S, Boivin JF. Association of selective serotonin reuptake inhibitors with the risk for spontaneous intracranial hemorrhage. JAMA Neurol. 2017;74(2):173–80.
Lee J, Lee J, Park S, Shin S, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46(2):e15.
de Abajo F, García-Rodríguez L. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents. Arch Gen Psychiatry. 2008;65:795–803.
Sahlberg M, Holm E, Gislason G, Kober L, Torp-Pedersen C, Andersson C. Association of selected antipsychotic agents with major adverse cardiovascular events and noncardiovascular mortality in elderly persons. J Am Heart Assoc. 2015;4(9):e001666.
Egeberg A, Bruun L, Mallbris L, Gislason G, Skov L, Wu J, et al. Family history predicts major adverse cardiovascular events (MACE) in young adults with psoriasis. J Am Acad Dermatol. 2016;75(2):340–6.
Ou S-M, Chu S, Chao P-W, Lee Y-J, Kuo S-C, Chen T-J, et al. Long-term mortality and major adverse cardiovascular events in sepsis survivors: a nationwide population-based study. Am J Respir Crit Care Med. 2016;194:209–17.
Health Insurance Review and Assessment Service. Evaluation and consideration methods of consistency between health insurance claims diagnostic codes and medical records. Health Insurance Review and Assessment Service, Wonju-si, South Korea; 2017.
Shin HY, Lee JY, Song J, Lee S, Lee J, Lim B, et al. Cause-of-death statistics in the Republic of Korea, 2014. J Korean Med Assoc. 2016;59(3):221–32.
Austin P, Fine J. Practical recommendations for reporting Fine–Gray model analyses for competing risk data. Stat Med. 2017;36(27):4391–400.
VanderWeele T, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74.
Kohler O, Petersen L, Mors O, Gasse C. Inflammation and depression: combined use of selective serotonin reuptake inhibitors and NSAIDs or paracetamol and psychiatric outcomes. Brain Behav. 2015;5(8):e00338.
Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343:d4551.
Hippisley-Cox J. Risk of myocardial infarction in patients taking cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs: population based nested case-control analysis. BMJ. 2005;330:1366.
Ungprasert P, Srivali N, Thongprayoon C. Nonsteroidal anti-inflammatory drugs and risk of incident heart failure: a systematic review and meta-analysis of observational studies. Clin Cardiol. 2016;39(2):111–8.
Kim J-M, Stewart R, Lee Y-S, Lee H-J, Kim M, Kim J-W, et al. Effect of escitalopram vs placebo treatment for depression on long-term cardiac outcomes in patients with acute coronary syndrome: a randomized clinical trial. JAMA. 2018;320(4):350–8.
Gillman P. Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br J Pharmacol. 2007;151(6):737–48.
Almuwaqqat Z, Jokhadar M, Norby F, Lutsey P, O'Neal W, Seyerle A, et al. Association of antidepressant medication type with the incidence of cardiovascular disease in the ARIC study. J Am Heart Assoc. 2019;8(11):e012503.
Bhala N, Emberson J, Merhi A, Abramson S, Arber N, Baron J, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382(9894):769–79.
Howren M, Lamkin D, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71(2):171–86.
Kaptoge S, Di Angelantonio E, Lowe G, Pepys M, Thompson S, Collins R, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375(9709):132–40.
Penninx B, Beekman A, Honig A, Deeg D, Schoevers R, van Eijk J, et al. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58(3):221–7.
Zellweger M, Osterwalder R, Langewitz W, Pfisterer M. Coronary artery disease and depression. Eur Heart J. 2004;25(1):3–9.
Chan A, Manson J, Albert C, Chae C, Rexrode K, Curhan G, et al. Nonsteroidal antiinflammatory drugs, acetaminophen, and the risk of cardiovascular events. Circulation. 2006;113(12):1578–87.
Singh G, Wu O, Langhorne P, Madhok R. Risk of acute myocardial infarction with nonselective non-steroidal anti-inflammatory drugs: a meta-analysis. Arthritis Res Ther. 2006;8:R153.
de Abajo F, Rodríguez L, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319(7217):1106–9.
Varga Z, Sabzwari S, Vargova V. Cardiovascular risk of nonsteroidal anti-inflammatory drugs: an under-recognized public health issue. Cureus. 2017;9(4):e1144.
Kubera M, Lin A-H, Kenis G, Bosmans E, van Bockstaele D, Maes M. Anti-inflammatory effects of antidepressants through suppression of the interferon-γ/interleukin-10 production ratio. J Clin Pyschopharmacol. 2001;21(2):199–206.
Trongtorsak P, Olankijanunt W, Trongtorsak A, Intamaso U. Antidepressant and anti-inflammatory effects of a combined fluoxetine and celecoxib treatment in a rat model of depression. Chula Med J. 2018;62(4):653–65.
Warner-Schmidt J, Vanover K, Chen E, Marshall J, Greengard P. Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans. Proc Natl Acad Sci USA. 2011;108:9262–7.
Rahman I, Humphreys K, Bennet A, Ingelsson E, Pedersen N, Magnusson P. Clinical depression, antidepressant use and risk of future cardiovascular disease. Eur J Epidemiol. 2013;28(7):589–95.
Hare D, Toukhsati S, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365–72.
Lippi G, Montagnana M, Favaloro E, Franchini M. Mental depression and cardiovascular disease: a multifaceted, bidirectional association. Semin Thromb Hemost. 2009;35:325–36.
Oh I, Filion K, Jeong H, Shin J. An empirical assessment of immeasurable time bias in the setting of nested case-control studies: statins and all-cause mortality among patients with heart failure. Pharmacoepidemiol Drug Saf. 2019;28(10):1318–27.
Blais L, Ernst P, Suissa S. Confounding by indication and channeling over time: the risks of beta 2-agonists. Am J Epidemiol. 1996;144(12):1161–9.
Bruehl S, Olsen R, Tronstad C, Sevre K, Burns J, Schirmer H, et al. Chronic pain-related changes in cardiovascular regulation and impact on comorbid hypertension in a general population: the Tromsø study. Pain. 2018;159(1):119–27.
Acknowledgements
We appreciate the National Health Insurance Service for their cooperation in providing access to the database (Data number: NHIS-2018-2-113).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the conduct of this study or the preparation of this article.
Conflict of interest
Han Eol Jeong, In-Sun Oh, Woo Jung Kim, and Ju-Young Shin have no conflicts of interest that are directly relevant to the content of this study.
Ethics Approval
Our study complies with the Declaration of Helsinki and the study protocol was approved by the Institutional Review Board of Sungkyunkwan University (SKKU 2018-03-010) and obtaining informed consent was waived by the Institutional Review Board.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
The health insurance claims database of the National Health Insurance Service can be accessed at https://nhiss.nhis.or.kr/bd/ab/bdaba022eng.do.
Code Availability
SAS syntax codes are available upon request.
Author Contributions
All authors contributed to the study design and interpretation of the data. HEJ wrote the manuscript. ISO conducted the statistical analyses. WJK interpreted the data and critically revised the manuscript. All authors reviewed and commented on drafts and approved the final manuscript and the decision to submit it for publication. JYS is the guarantor.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jeong, H.E., Oh, IS., Kim, W.J. et al. Risk of Major Adverse Cardiovascular Events Associated with Concomitant Use of Antidepressants and Non-steroidal Anti-inflammatory Drugs: A Retrospective Cohort Study. CNS Drugs 34, 1063–1074 (2020). https://doi.org/10.1007/s40263-020-00750-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00750-4