Abstract
Outcome assessment in the pharmacological treatment of alcohol use disorders (AUDs) faces specific challenges resulting from low adherence to treatment, high rates of dropout, and the susceptibility of patient self-reports to bias. This review discusses methodological issues in planning, conducting, and interpreting clinical trials on AUD treatment against the background of the principle of ‘strictness and fairness’ of testing. Threats to fairness include factors that limit the implementation of an intervention, such as low compliance and early treatment termination. In turn, fairness of testing is increased by factors that support the degree to which an intervention is implemented, such as the use of adequate pretreatments and the matching of psychosocial and pharmacological treatment strategies. Furthermore, selecting outcomes on the basis of an intervention’s mechanism of action and including continuous outcomes as sensitive measures of drinking change further increases fairness by increasing the likelihood that the data will adequately reflect the effects of the intervention. On the other hand, strictness of testing is increased by all measures that limit the influence of confounders that could potentially lead to an overestimation of effects. The use of a side effect-mimicking placebo to prevent an unmasking of blinding and the repeated assessment of alcohol biomarkers to validate drinking self-reports might be valid strategies to further increase the strictness of testing by limiting risks of bias in trials of AUD treatment.
Similar content being viewed by others
References
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry. 2015;72(8):757–66.
Kranzler HR, Soyka M. Diagnosis and pharmacotherapy of alcohol use disorder: a review. JAMA. 2018;320(8):815–24.
Rehm J, Dawson D, Frick U, Gmel G, Roerecke M, Shield KD, et al. Burden of disease associated with alcohol use disorders in the United States. Alcohol Clin Exp Res. 2014;38(4):1068–77.
Donoghue K, Elzerbi C, Saunders R, Whittington C, Pilling S, Drummond C. The efficacy of acamprosate and naltrexone in the treatment of alcohol dependence, Europe versus the rest of the world: a meta-analysis. Addiction. 2015;110(6):920–30.
Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275–93.
Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33(8):1010–24.
Raes V, De Jong CA, De Bacquer D, Broekaert E, De Maeseneer J. The effect of using assessment instruments on substance-abuse outpatients’ adherence to treatment: a multi-centre randomised controlled trial. BMC Health Serv Res. 2011;11:123.
Matthews S, Dwyer R, Snoek A. Stigma and self-stigma in addiction. J Bioeth Inq. 2017;14(2):275–86.
Schomerus G, Matschinger H, Angermeyer MC. Attitudes towards alcohol dependence and affected individuals: persistence of negative stereotypes and illness beliefs between 1990 and 2011. Eur Addict Res. 2014;20(6):293–9.
Yoshino A, Kato M. Influence of social desirability response set on self-report for assessing the outcome of treated alcoholics. Alcohol Clin Exp Res. 1995;19(6):1517–9.
Rosner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010;9:CD004332.
Allen JP. Measuring outcome in interventions for alcohol dependence and problem drinking: executive summary of a conference sponsored by the National Institute on alcohol abuse and alcoholism. Alcohol Clin Exp Res. 2003;27(10):1657–60.
Westermann R, Hager W. Error probabilities in educational and psychological research. J Educ Stat. 1986;11:117–46.
Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101(2):212–22.
Witkiewitz K, Finney JW, Harris AH, Kivlahan DR, Kranzler HR. Guidelines for the reporting of treatment trials for alcohol use disorders. Alcohol Clin Exp Res. 2015;39(9):1571–81.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311(18):1889–900.
Shen WW. Anticraving therapy for alcohol use disorder: a clinical review. Neuropsychopharmacol Rep. 2018;38(3):105–16.
Minozzi S, Saulle R, Rosner S. Baclofen for alcohol use disorder. Cochrane Database Syst Rev. 2018;11:CD012557.
Pierce M, Sutterland A, Beraha EM, Morley K, van den Brink W. Efficacy, tolerability, and safety of low-dose and high-dose baclofen in the treatment of alcohol dependence: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2018;28(7):795–806.
Mutschler J, Grosshans M, Soyka M, Rosner S. Current findings and mechanisms of action of disulfiram in the treatment of alcohol dependence. Pharmacopsychiatry. 2016;49(4):137–41.
Rosner S, Grosshans M, Mutschler JH. Disulfiram: Aktuelle Befunde und Wirkmechanismen. Suchtmedizin. 2014;16(2):47–52.
Skinner MD, Lahmek P, Pham H, Aubin HJ. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis. PLoS One. 2014;9(2):e87366.
Bujarski S, O’Malley SS, Lunny K, Ray LA. The effects of drinking goal on treatment outcome for alcoholism. J Consult Clin Psychol. 2013;81(1):13–22.
Hasin DS, Wall M, Witkiewitz K, Kranzler HR, Falk D, Litten R, et al. Change in non-abstinent WHO drinking risk levels and alcohol dependence: a 3 year follow-up study in the US general population. Lancet Psychiatry. 2017;4(6):469–76.
European Medicines Agency. Guideline on the development of medicinal products for the treatment of alcohol dependence. London: European Medicines Agency; 2010.
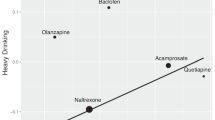
Palpacuer C, Duprez R, Huneau A, Locher C, Boussageon R, Laviolle B, et al. Pharmacologically controlled drinking in the treatment of alcohol dependence or alcohol use disorders: a systematic review with direct and network meta-analyses on nalmefene, naltrexone, acamprosate, baclofen and topiramate. Addiction. 2018;113(2):220–37.
Bakhshi E, McArdle B, Mohammad K, Seifi B, Biglarian A. Let continuous outcome variables remain continuous. Comput Math Methods Med. 2012;2012:639124.
MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychol Methods. 2002;7(1):19–40.
Yoo B. The impact of dichotomization in longitudinal data analysis: a simulation study. Pharm Stat. 2010;9(4):298–312.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res. 2017;41(1):179–86.
Tiffany ST, Friedman L, Greenfield SF, Hasin DS, Jackson R. Beyond drug use: a systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction. 2012;107(4):709–18.
Carr AJ, Gibson B, Robinson PG. Measuring quality of life: is quality of life determined by expectations or experience? BMJ. 2001;322(7296):1240–3.
Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, Greenfield SF. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in the COMBINE study. Addiction. 2006;101(12):1696–704.
Becker SJ, Curry JF, Yang C. Longitudinal association between frequency of substance use and quality of life among adolescents receiving a brief outpatient intervention. Psychol Addict Behav. 2009;23(3):482–90.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. Totowa: Human Press; 1992.
Miller WR. Form 90. A structured assessment interview for drinking and related behaviors: test manual. Bethesda: National Institute on Alcohol Abuse and Alcoholism; 1996.
Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychol Assess. 2009;21(4):486–97.
Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: self-report, transdermal assessment, and prediction of dependence symptoms. Addict Behav. 2015;50:205–12.
Maisto SA, Conigliaro JC, Gordon AJ, McGinnis KA, Justice AC. An experimental study of the agreement of self-administration and telephone administration of the timeline followback interview. J Stud Alcohol Drugs. 2008;69(3):468–71.
Pedersen ER, Grow J, Duncan S, Neighbors C, Larimer ME. Concurrent validity of an online version of the timeline followback assessment. Psychol Addict Behav. 2012;26(3):672–7.
Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12.
Finney JW, Moyer A, Swearingen CE. Outcome variables and their assessment in alcohol treatment studies: 1968–1998. Alcohol Clin Exp Res. 2003;27(10):1671–9.
Andresen-Streichert H, Muller A, Glahn A, Skopp G, Sterneck M. Alcohol biomarkers in clinical and forensic contexts. Dtsch Arztebl Int. 2018;115(18):309–15.
Ingall GB. Alcohol biomarkers. Clin Lab Med. 2012;32(3):391–406.
Tavakoli HR, Hull M, Michael Okasinski L. Review of current clinical biomarkers for the detection of alcohol dependence. Innov Clin Neurosci. 2011;8(3):26–33.
Cabezas J, Lucey MR, Bataller R. Biomarkers for monitoring alcohol use. Clin Liver Dis. 2016;2:59–63.
Karns-Wright TE, Roache JD, Hill-Kapturczak N, Liang Y, Mullen J, Dougherty DM. Time delays in transdermal alcohol concentrations relative to breath alcohol concentrations. Alcohol Alcohol. 2017;52(1):35–41.
Swift R. Transdermal alcohol measurement for estimation of blood alcohol concentration. Alcohol Clin Exp Res. 2000;24(4):422–3.
Voas RB, DuPont RL, Talpins SK, Shea CL. Towards a national model for managing impaired driving offenders. Addiction. 2011;106(7):1221–7.
Dougherty DM, Hill-Kapturczak N, Liang Y, Karns TE, Cates SE, Lake SL, et al. Use of continuous transdermal alcohol monitoring during a contingency management procedure to reduce excessive alcohol use. Drug Alcohol Depend. 2014;142:301–6.
Roache JD, Karns-Wright TE, Goros M, Hill-Kapturczak N, Mathias CW, Dougherty DM. Processing transdermal alcohol concentration (TAC) data to detect low-level drinking. Alcohol. 2018. https://doi.org/10.1016/j.alcohol.2018.08.014.
Koffarnus MN, Bickel WK, Kablinger AS. Remote alcohol monitoring to facilitate incentive-based treatment for alcohol use disorder: a randomized trial. Alcohol Clin Exp Res. 2018;42(12):2423–31.
Deci EL, Koestner R, Ryan RM. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull. 1999;125(6):627–68 (discussion 92–700).
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80(3):179–89.
Ray LA, Bujarski S, Roche DJO, Magill M. Overcoming the “valley of death” in medications development for alcohol use disorder. Alcohol Clin Exp Res. 2018;42(9):1612–22.
Cook TD, Campbell DT. Quasi-experimentation: design and analysis issues for field settings. Chicago: Rand McNally; 1979.
Del Re AC, Maisel NC, Blodgett JC, Finney JW. Intention-to-treat analyses and missing data approaches in pharmacotherapy trials for alcohol use disorders. BMJ Open. 2013;3(11):e003464.
Heinala P, Alho H, Kiianmaa K, Lonnqvist J, Kuoppasalmi K, Sinclair JD. Targeted use of naltrexone without prior detoxification in the treatment of alcohol dependence: a factorial double-blind, placebo-controlled trial. J Clin Psychopharmacol. 2001;21(3):287–92.
O’Malley SS, Jaffe AJ, Chang G, Schottenfeld RS, Meyer RE, Rounsaville B. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry. 1992;49(11):881–7.
Witkiewitz K, Falk DE, Kranzler HR, Litten RZ, Hallgren KA, O’Malley SS, et al. Methods to analyze treatment effects in the presence of missing data for a continuous heavy drinking outcome measure when participants drop out from treatment in alcohol clinical trials. Alcohol Clin Exp Res. 2014;38(11):2826–34.
Stout RL. Methodological and statistical considerations in measuring alcohol treatment effects. Alcohol Clin Exp Res. 2003;27(10):1686–91.
Lehert P. Review and discussion of statistical analysis of controlled clinical trials in alcoholism. Alcohol Alcohol Suppl. 1993;2:157–63.
Moncrieff J. A comparison of antidepressant trials using active and inert placebos. Int J Methods Psychiatr Res. 2003;12(3):117–27.
Jensen JS, Bielefeldt AO, Hrobjartsson A. Active placebo control groups of pharmacological interventions were rarely used but merited serious consideration: a methodological overview. J Clin Epidemiol. 2017;87:35–46.
Rosner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2010;12:CD001867.
Litten RZ, Castle IJ, Falk D, Ryan M, Fertig J, Chen CM, et al. The placebo effect in clinical trials for alcohol dependence: an exploratory analysis of 51 naltrexone and acamprosate studies. Alcohol Clin Exp Res. 2013;37(12):2128–37.
Khan A, Detke M, Khan SR, Mallinckrodt C. Placebo response and antidepressant clinical trial outcome. J Nerv Ment Dis. 2003;191(4):211–8.
Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the food and drug administration. PLoS Med. 2008;5(2):e45.
Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–17.
Fertig JB, Ryan ML, Falk DE, Litten RZ, Mattson ME, Ransom J, et al. A double-blind, placebo-controlled trial assessing the efficacy of levetiracetam extended-release in very heavy drinking alcohol-dependent patients. Alcohol Clin Exp Res. 2012;36(8):1421–30.
Chan AW, Tetzlaff JM, Altman DG, Dickersin K, Moher D. SPIRIT 2013: new guidance for content of clinical trial protocols. Lancet. 2013;381(9861):91–2.
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH Harmonised Tripartite Guideline: Statistical Principles for Clinical Trials E9. London: European Medicines Agency; 1998.
Heffner JL, Tran GQ, Johnson CS, Barrett SW, Blom TJ, Thompson RD, et al. Combining motivational interviewing with compliance enhancement therapy (MI-CET): development and preliminary evaluation of a new, manual-guided psychosocial adjunct to alcohol-dependence pharmacotherapy. J Stud Alcohol Drugs. 2010;71(1):61–70.
Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet. 2002;359(9308):781–5.
Spieth PM, Kubasch AS, Penzlin AI, Illigens BM, Barlinn K, Siepmann T. Randomized controlled trials—a matter of design. Neuropsychiatr Dis Treat. 2016;12:1341–9.
Hallgren KA, Witkiewitz K. Missing data in alcohol clinical trials: a comparison of methods. Alcohol Clin Exp Res. 2013;37(12):2152–60.
Jackson D, White IR, Mason D, Sutton S. A general method for handling missing binary outcome data in randomized controlled trials. Addiction. 2014;109(12):1986–93.
Klemperer EM, Hughes JR, Naud S. Study characteristics influence the efficacy of substance abuse treatments: a meta-analysis of medications for alcohol use disorder. Drug Alcohol Depend. 2018;190:229–34.
Sobell MB, Sobell LC. Controlled drinking after 25 years: how important was the great debate? Addiction. 1995;90(9):1149–53 (discussion 57–77).
Jones JD, Comer SD, Kranzler HR. The pharmacogenetics of alcohol use disorder. Alcohol Clin Exp Res. 2015;39(3):391–402.
Acknowledgements
The authors thank Jacquie Klesing, Board-certified Editor in the Life Sciences (ELS), for editing assistance with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this review.
Conflict of interest
Susanne Rösner and Michael Soyka declare that they have no conflict of interest related to the content of this review.
Rights and permissions
About this article
Cite this article
Rösner, S., Soyka, M. Outcome Assessment in Trials of Pharmacological Treatments for Alcohol Use Disorders: Fair and Strict Testing. CNS Drugs 33, 649–657 (2019). https://doi.org/10.1007/s40263-019-00644-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-019-00644-0