Abstract
Background
Ketamine is an emerging third-line medication for refractory status epilepticus, a medical and neurological emergency requiring prompt and appropriate treatment. Owing to its pharmacological properties, ketamine represents a practical alternative to conventional anaesthetics.
Objective
The objective of this study was to assess the efficacy and safety of ketamine to treat refractory status epilepticus in paediatric and adult populations.
Methods
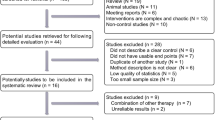
We conducted a literature search using the PubMed database, Cochrane Database of Systematic Reviews and ClinicalTrials.gov website.
Results
We found no results from randomised controlled trials. The literature included 27 case reports accounting for 30 individuals and 14 case series, six of which included children. Overall, 248 individuals (29 children) with a median age of 43.5 years (range 2 months to 67 years) were treated in 12 case series whose sample size ranged from 5 to 67 patients (median 11). Regardless of the status epilepticus type, ketamine was twice as effective if administered early, with an efficacy rate as high as 64% in refractory status epilepticus lasting 3 days and dropping to 32% when the mean refractory status epilepticus duration was 26.5 days. Ketamine doses were extremely heterogeneous and did not appear to be an independent prognostic factor. Endotracheal intubation, a negative prognostic factor for status epilepticus, was unnecessary in 12 individuals (10 children), seven of whom were treated with oral ketamine for non-convulsive status epilepticus.
Conclusions
Although ketamine has proven to be effective in treating refractory status epilepticus, available studies are hampered by methodological limitations that prevent any firm conclusion. Results from two ongoing studies (ClinicalTrials.gov identification number: NCT02431663 and NCT03115489) and further clinical trials will hopefully confirm the better efficacy and safety profile of ketamine compared with conventional anaesthetics as third-line therapy in refractory status epilepticus, both in paediatric and adult populations.

Similar content being viewed by others
References
Commission on Classification and Terminology of the International. League Against Epilepsy. Proposal for revised clinical and electrographic classification of epileptic seizures. Epilepsia. 1981;22:489–501.
Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus: report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015;56:1515–23.
Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134:2802–18.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23.
Abend NS, Duglas DT. Treatment of refractory status epilepticus: literature review and a proposed protocol. Pediatr Neurol. 2008;38:377–80.
Sofou K, Kristjansdòttir R, Papachatzakis N, Ahmadzadeh A, Uvebrant P. Management of prolonged seizures and status epilepticus in childhood: a systematic review. J Child Neurol. 2009;24:918–26.
Fernandez A, Claassen J. Refractory status epilepticus. Curr Opin Crit Care. 2012;18:127–31.
Leitinger M, Beniczky S, Rohracher A, et al. Salzburg consensus criteria for non-convulsive status epilepticus: approach to clinical application. Epilepsy Behav. 2015;49:158–63.
Meierkord H, Holtkamp M. Non-convulsive status epilepticus in adults: clinical forms and treatment. Lancet Neurol. 2007;6:329–39.
Wasterlain CG, Chen JW. Mechanistic and pharmacologic aspects of status epilepticus and its treatment with new antiepileptic drugs. Epilepsia. 2008;49(Suppl. 9):63–73.
Naylor DE. Glutamate and GABA in the balance: convergent pathways sustain seizures during status epilepticus. Epilepsia. 2010;5(Suppl. 3):106–9.
Zeiler FA, Teitelbaum J, Gillman LM, West M. NMDA antagonists for refractory seizures. Neurocrit Care. 2014;20:502–13.
Dorandeu F, Dhote F, Barbier L, Baccus B, Testylier G. Treatment of status epilepticus with ketamine, are we there yet? CNS Neurosci Ther. 2013;19:411–27.
Borris DJ, Bertram EH, Kapur J. Ketamine controls prolonged status epilepticus. Epilepsy Res. 2000;42:117–22.
Martin BS, Kapur J. A combination of ketamine and diazepam synergistically controls refractory status epilepticus induced by cholinergic stimulation. Epilepsia. 2008;49:248–55.
Niquet J, Baldwin R, Norman K, Suchomelova L, Lumley L, Wasterlain CG. Midazolam-ketamine dual therapy stops cholinergic status epilepticus and reduces Morris water maze deficits. Epilepsia. 2016;57:1406–15.
Zanos P, Moaddel R, Morris PJ, et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70:621–60.
Craven R. Ketamine. Anaesthesia. 2007;62:48–53.
Shibuta S, Varathan S, Mashimo T. Ketamine and thiopental sodium: individual and combined neuroprotective effects on cortical cultures exposed to NMDA or nitric oxide. Br J Anaesth. 2006;97:517–24.
Schmutzhard E, Pfausler B. Complications of the management of status epilepticus in the intensive care unit. Epilepsia. 2011;52(Suppl. 8):39–41.
Dorandeu F, Barbier L, Dhote F, Testylier G, Carpentier P. Ketamine combinations for the field treatment of soman-induced self-sustaining status epilepticus: review of current data and perspectives. Chem Biol Interact. 2013;203:154–9.
Ilvento L, Rosati A, Marini C, L’Erario M, Mirabile L, Guerrini R. Ketamine in refractory convulsive status epilepticus in children avoids endotracheal intubation. Epilepsy Behav. 2015;49:343–6.
Zeiler FA, West M. Ketamine for status epilepticus: Canadian physician views and time to push forward. Can J Neurol Sci. 2015;42:132–4.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Guyatt GH, Oxman AD, Vist G, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, et al. Rating quality of evidence and strength of recommendations: what is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–8.
Rosati A, L’Erario M, Ilvento L, Pisano T, Mirable L, Guerrini R. An ongoing open-label uncontrolled study of the efficacy and safety of ketamine in children with refractory status epilepticus. Epilepsia. 2013;54(Suppl. 3):17.
Rosati A, L’Erario M, Ilvento L, Cecchi C, Pisano T, Mirabile L, et al. Efficacy and safety of ketamine in refractory status epilepticus in children. Neurology. 2012;79:2355–8.
Bleck TP, Quigg MS, Nathan BR, Smith TL, Kapur J. Electroencephalographic effects of ketamine treatment for refractory status epilepticus. Epilepsia. 2002;43(Suppl. 7):282.
Singh D, Kelly K, Rana S, Valeriano J. Use of ketamine in treating refractory status epilepticus. Epilepsia. 2009;50(Suppl. 11):63.
Gaspard N, Foreman B, Judd LM, et al. Intravenous ketamine for the treatment of refractory status epilepticus: a retrospective multicenter study. Epilepsia. 2013;54:1498–503.
Gosselin-Lefebvre S, Rabinstein A, Rossetti A, Savard M. Ketamine usefulness in refractory status epilepticus: a retrospective multicenter study. Can J Neurol Sci. 2013;40(Suppl. 1):S31.
Synowiec AS, Singh DS, Yenugadhati V, et al. Ketamine use in the treatment of refractory status epilepticus. Epilepsy Res. 2013;105:183–8.
Basha MM, Alqallaf A, Shah AK. Drug-induced EEG pattern predicts effectiveness of ketamine in treating refractory status epilepticus. Epilepsia. 2015;56:e44–8.
Sabharwal V, Ramsay E, Martinez R, Shumate R, Khan F, Dave H, Iwuchukwu I, McGrade H. Propofol-ketamine combination therapy for effective control of super-refractory status epilepticus. Epilepsy Behav. 2015;52:264–6.
Höfler J, Rohracher A, Kalss G, Zimmermann G, Dobesberger J, Pilz G, Leitinger M, Kuchukhidze G, Butz K, Taylor A, Novak H, Trinka E. (S)-Ketamine in refractory and super-refractory status epilepticus: a retrospective study. CNS Drugs. 2016;30:869–76.
Walker MC, Howard RS, Smith SJ, et al. Diagnosis and treatment of status epilepticus on a neurological intensive care unit. QJM. 1996;89:913–20.
Ubogu EE, Sagar SM, Lerner AJ, et al. Ketamine for refractory status epilepticus: a case of possible ketamine induced neurotoxicity. Epilepsy Behav. 2003;4:70–5.
Robakis TK, Hirsch LJ. Literature review, case report, and expert discussion of prolonged refractory status epilepticus. Neurocrit Care. 2006;4:35–46.
Prüss H, Holtkamp M. Ketamine successfully terminates malignant status epilepticus. Epilepsy Res. 2008;82:219–22.
Hsieh CY, Sung PS, Tsai JJ, et al. Terminating prolonged refractory status epilepticus using ketamine. Clin Neuropharmacol. 2010;33:165–7.
Yeh PS, Shen HN, Chen TY. Oral ketamine controlled refractory nonconvulsive status epilepticus in an elderly patient. Seizure. 2011;20:723–6.
Kramer AH. Early ketamine to treat refractory status epilepticus. Neurocrit Care. 2012;16:299–305.
Zeiler FA, Kaufmann AM, Gillman LM, et al. Ketamine for medically refractory status epilepticus after elective aneurysm clipping. Neurocrit Care. 2013;19:119–24.
Esaian D, Joset D, Lazarovits C, Dugan PC, Fridman D. Ketamine continuous infusion for refractory status epilepticus in a patient with anticonvulsant hypersensitivity syndrome. Ann Pharmacother. 2013;47:1569–76.
Shrestha GS, Joshi P, Chhetri S, et al. Intravenous ketamine for treatment of super-refractory convulsive status epilepticus with septic shock: a report of two cases. Indian J Crit Care Med. 2015;19:283–5.
McGinn KA, Bishop L, Sarwal A. Use of ketamine in barbiturate coma for status epilepticus. Clin Neuropharmacol. 2016;39:62–5.
Dillien P, Ferrao Santos S, van Pesch V, Suin V, Lamoral S, Hantson P. New-onset refractory status epilepticus: more investigations, more questions. Case Rep Neurol. 2016;8:127–33.
Al-Busaidi M, Burad J, Al-Belushi A, Gujjar A. Super refractory status epilepticus in Hashimoto’s encephalopathy. Oman Med J. 2017;32:247–50.
Pizzi MA, Kamireddi P, Tatum WO, Shih JJ, Jackson DA, Freeman WD. Transition from intravenous to enteral ketamine for treatment of nonconvulsive status epilepticus. J Intensive Care. 2017;5:54.
Koffman L, Yan Yiu H, Farrokh S, Lewin J, Geocadin R, Ziai W. Ketamine infusion for refractory status epilepticus: a case report of cardiac arrest. J Clin Neurosci. 2018;47:149–51.
Mutkule DP, Rao SM, Chaudhuri JR, Rajasri K. Successful use of ketamine for burst suppression in super refractory status epilepticus following substance Abuse. Indian J Crit Care Med. 2018;22:49–50.
Mewasingh LD, Sekhara T, Aeby A, Christiaens FJC, Dan B. Oral ketamine in paediatric non-convulsive status epilepticus. Seizure. 2003;12:483–9.
Kravljanac R, Nikolic LJ, Djuric M, Jovic N, Jankovic B. Treatment of status epilepticus in children: 15-year single center experience. Acta Paediatr. 2010;99(Suppl. 462):107.
Al-Otaibi AD, McCoy B, Cortez M, Hutchison JS, Hahn CS. The use of ketamine in refractory status epilepticus. Can J Neurol Sci. 2010;37(3 Suppl. 1):S69.
Sheth RD, Gidal BE. Refractory status epilepticus: response to ketamine. Neurology. 1998;51:1765–6.
Kramer U, Shorer Z, Ben-Zeev B, Lerman-Sagie T, Goldberg-Stern H, Lahat E. Severe refractory status epilepticus owing to presumed encephalitis. J Child Neurol. 2005;20:184–7.
Elting JW, Naalt JV, Fock JM. Mild hypothermia for refractory focal status epilepticus in an infant with hemimegalencephaly. Eur J Paediatr Neurol. 2010;14:452–5.
Andrade C, Franca S, Sampaio M, et al. Successful use of ketamine in paediatric super-refractory status epilepticus—case report. Epilepsia. 2012;53:98.
Tarocco A, Ballardini E, Garani G. Use of ketamine in a newborn with refractory status epilepticus: a case report. Pediatr Neurol. 2014;51:154–6.
Horino A, Kawawaki H, Fukuoka M, et al. A case of succinic semialdehyde dehydrogenase deficiency with status epilepticus and rapid regression. Brain Dev. 2016;38:866–70.
Mirás Veiga A, Moreno DC, Menéndez AI, et al. Effectiveness of electroconvulsive therapy for refractory status epilepticus in febrile infection-related epilepsy syndrome. Neuropaediatrics. 2017;48:45–8.
Chiusolo F, Diamanti A, Bianchi R, et al. From intravenous to enteral ketogenic diet in PICU: a potential treatment strategy for refractory status epilepticus. Eur J Paediatr Neurol. 2016;20:843–7.
Li D, Yuan H, Ortiz-Gonzalez XR, et al. GRIN2D recurrent de novo dominant mutation causes a severe epileptic encephalopathy treatable with NMDA receptor channel blockers. Am J Hum Genet. 2016;99:802–16.
Aroor S, Shravan K, Mundkur SC, Jayakrishnan C, Rao SS. Super-refractory status epilepticus: a therapeutic challenge in paediatrics. J Clin Diagn Res. 2017;11:SR01–4.
Caputo D, Iorio R, Vigevano F, Fusco L. Febrile infection-related epilepsy syndrome (FIRES) with super-refractory status epilepticus revealing autoimmune encephalitis due to GABAAR antibodies. Eur J Paediatr Neurol. 2018;22:182–5.
Löscher W. Single versus combinatorial therapies in status epilepticus: novel data from preclinical models. Epilepsy Behav. 2015;49:20–5.
Griesdale DE, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Int Care Med. 2008;34:1835–42.
Carroll CL, Spinella PC, Corsi JM, Stoltz P, Zucker AR. Emergent endotracheal intubations in children: be careful if it’s late when you intubate. Pediatr Crit Care Med. 2010;11:343–8.
Fujikawa DG. Neuroprotective effect of ketamine administered after status epilepticus onset. Epilepsia. 1995;36:186–95.
Cunha AO, Mortari MR, Liberato JL, dos Santos WF. Neuroprotective effects of diazepam, carbamazepine, phenytoin and ketamine after pilocarpine-induced status epilepticus. Basic Clin Pharmacol Toxicol. 2009;104:470–7.
Dorandeu F, Baille V, Mikler J, et al. Protective effects of S+ ketamine and atropine against lethality and brain damage during soman-induced status epilepticus in guinea-pigs. Toxicology. 2007;234:185–93.
Vargas-Sánchez K, Mogilevskaya M, Rodríguez-Pérez J, Rubiano MG, Javela JJ, González-Reyes RE. Astroglial role in the pathophysiology of status epilepticus: an overview. Oncotarget. 2018;9(42):26954–76.
Loix S, De Kock M, Henin P. The anti-inflammatory effects of ketamine: state of the art. Acta Anaesthesiol Belg. 2011;62:47–58.
Dorandeu F. Ketamine for the treatment of (super) refractory status epilepticus? Not quite yet. Expert Rev Neurother. 2017;17:419–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this study.
Conflict of interest
Anna Rosati, Salvatore De Masi and Renzo Guerrini have no conflicts of interest that are directly relevant to the contents of this study.
Rights and permissions
About this article
Cite this article
Rosati, A., De Masi, S. & Guerrini, R. Ketamine for Refractory Status Epilepticus: A Systematic Review. CNS Drugs 32, 997–1009 (2018). https://doi.org/10.1007/s40263-018-0569-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-018-0569-6