Abstract
Background and objective
(Patho)physiological changes in older people may influence the pharmacokinetics (PK), and consequently the target attainment, of ß-lactam antibiotics using standard dosing regimens. This systematic review compiles the current knowledge on the PK and target attainment of ß-lactam antibiotics in older people, with the aim to identify priorities for dose optimization in this patient population.
Methods
A systematic literature search of the PubMed and EMBASE databases was conducted. Relevant articles published prior to 1 December 2021 were identified as eligible when they included data on the PK of ß-lactam antibiotics in adults ≥ 65 years of age. Extracted information included reported PK parameters (volume of distribution, clearance [CL], elimination rate constant, intercompartmental CL, elimination half-life, area under the concentration-time curve, maximum and trough concentration), covariates on PK parameters, target attainment rate, and dosing recommendations.
Results
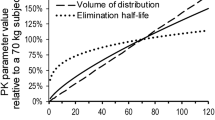
Ninety-one relevant articles were included in this review. Four main ß-lactam subclasses were represented: 59.3% on cephalosporins + cephamycins, 25.3% on penicillins, 15.4% on carbapenems, and 3.3% on monobactams; 65.9% of articles involved intravenous administration, 16.5% mixed administration routes, 12.1% oral administration, and 5.5% intramuscular administration. The majority of studies had a small sample size, often did not include detailed information on the study population and methods, and were fairly old. CL was, on average, decreased, while elimination half-life was prolonged in aged subjects compared with young subjects. Volume of distribution was generally similar between age groups. Most studies identified renal function as the most important contributor to altered drug CL. In only 30.8% of the articles, target attainment was studied, and in 35.7% of these articles, target attainment was found to be suboptimal. Dosing recommendations were incorporated in 87.9% of articles.
Conclusion
Studies frequently fail to provide an evidence-based dosing recommendation for this diverse patient population. Model-based PK studies that address both physiological and disease-related changes are urgently needed. This review identified gaps of knowledge to set priorities for further research.

Similar content being viewed by others
References
Eurostat. Population structure and ageing. 2022 [cited 2 Apr 2022]. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Population_structure_and_ageing#Past_and_future_population_ageing_trends_in_the_EU. Accessed 14 Sept 2022.
Benson JM. Antimicrobial pharmacokinetics and pharmacodynamics in older adults. Infect Dis Clin N Am. 2017;31(4):609–17.
Ljungberg B, Nilsson-Ehle I. Pharmacokinetics of antimicrobial agents in the elderly. Rev Infect Dis. 1987;9(2):250–64.
Noreddin AM, El-Khatib W, Haynes V. Optimal dosing design for antibiotic therapy in the elderly: a pharmacokinetic and pharmacodynamic perspective. Recent Pat Anti-Infect Drug Discov. 2008;3(1):45–52. https://doi.org/10.2174/157489108783413191.
Tan SJ, Cockcroft M, Page-Sharp M, Arendts G, Davis TME, Moore BR, et al. Population pharmacokinetic study of ceftriaxone in elderly patients, using cystatin C-based estimates of renal function to account for frailty. Antimicrob Agents Chemother. 2020;64(10):e00874-e920. https://doi.org/10.1128/AAC.00874-20.
Soto E, Shoji S, Muto C, Tomono Y, Marshall S. Population pharmacokinetics of ampicillin and sulbactam in patients with community-acquired pneumonia: evaluation of the impact of renal impairment. Br J Clin Pharmacol. 2014;77(3):509–21. https://doi.org/10.1111/bcp.12232.
Anderson BJ, Holford NH. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol. 2008;48:303–32. https://doi.org/10.1146/annurev.pharmtox.48.113006.094708.
Kanji S, Hayes M, Ling A, Shamseer L, Chant C, Edwards DJ, et al. Reporting guidelines for clinical pharmacokinetic studies: the ClinPK Statement. Clin Pharmacokinet. 2015;54(7):783–95. https://doi.org/10.1007/s40262-015-0236-8.
Haeseker M, Havenith T, Stolk L, Neef C, Bruggeman C, Verbon A. Is the standard dose of amoxicillin-clavulanic acid sufficient? BMC Pharmacol Toxicol. 2014;15(1):38. https://doi.org/10.1186/2050-6511-15-38.
Sjövall J, Alvan G, Huitfeldt B. Intra- and inter-individual variation in pharmacokinetics of intravenously infused amoxycillin and ampicillin to elderly volunteers. Br J Clin Pharmacol. 1986;21(2):171–81.
Ball P, Barford T, Gilbert J. Prolonged serum elimination half-life of amoxycillin in the elderly. J Antimicrob Chemother. 1978;4(4):385–6.
Janknegt R, Boogaard-Van Den Born J, Hameleers BAMJ, Hooymans PM, Rang J, Smits CAM, et al. Pharmacokinetics of amoxycillin in elderly inpatients. Pharm Weekbl Sci. 1992;14(1):27–9.
Lee SW, Choi Y, Jang K, Yoon SH, Chung J-Y. Multiple-dose pharmacokinetics and safety of amoxicillin/clavulanate in healthy elderly subjects. Int J Clin Pharmacol Ther. 2020;58(11):634–41.
Triggs EJ, Johnson JM, Learoyd B. Absorption and disposition of ampicillin in the elderly. Eur J Clin Pharmacol. 1980;18(2):195–8.
Champoux N, Du Souich P, Ravaoarinoro M, Phaneuf D, Latour J, Cusson JR. Single-dose pharmacokinetics of ampicillin and tobramycin administered by hypodermoclysis in young and older healthy volunteers. Br J Clin Pharmacol. 1996;42(3):325–31. https://doi.org/10.1046/j.1365-2125.1996.03967.x.
Rho JP, Jones A, Woo M, Castle S, Smith K, Bawdon RW, et al. Single-dose pharmacokinetics of intravenous ampicillin plus sulbactam in healthy elderly and young adult subjects. J Antimicrob Chemother. 1989;24(4):573–80.
Meyers BR, Wilkinson P, Mendelson MH, Walsh S, Bournazos C, Hirschman SZ. Pharmacokinetics of ampicillin-sulbactam in healthy elderly and young volunteers. J Antimicrob Agents Chemother. 1991;35(10):2098–101.
Majcher-Peszynska J, Loebermann M, Klammt S, Frimmel S, Mundkowski RG, Welte T, et al. Ampicillin/sulbactam in elderly patients with community-acquired pneumonia. Infection. 2014;42(1):79–87. https://doi.org/10.1007/s15010-013-0518-8.
Matsubara K, Matsumoto K, Yokoyama Y, Watanabe E, Enoki Y, Shigemi A, et al. Dosing optimization of ampicillin-sulbactam based on cystatin C in elderly patients with pneumonia. Biol Pharm Bull. 2021;44(5):732–6. https://doi.org/10.1248/bpb.b20-00781.
Gath J, Charles B, Sampson J, Smithurst B. Pharmacokinetics and bioavailability of flucloxacillin in elderly hospitalized patients. J Clin Pharmacol. 1995;35(1):31–6.
Anderson P, Bluhm G, Ehrnebo M, Herngren L, Jacobson B. Pharmacokinetics and distribution of flucloxacillin in pacemaker patients. Eur J Clin Pharmacol. 1985;27(6):713–9. https://doi.org/10.1007/bf00547055.
Fourtillan JB, Couet W, Mignot A. Pharmacokinetics of piperacillin in the young and the elderly. Presse Med. 1986;15(46):2321–3.
Hatti M, Solomonidi N, Odenholt I, Tham J, Resman F. Considerable variation of trough β-lactam concentrations in older adults hospitalized with infection: a prospective observational study. Eur J Clin Microbiol Infect Dis. 2018;37(3):485–93. https://doi.org/10.1007/s10096-018-3194-x.
Cojutti PG, Morandin E, Baraldo M, Pea F. Population pharmacokinetics of continuous infusion of piperacillin/tazobactam in very elderly hospitalized patients and considerations for target attainment against Enterobacterales and Pseudomonas aeruginosa. Int J Antimicrob Agents. 2021. https://doi.org/10.1016/j.ijantimicag.2021.106408.
Ishihara N, Nishimura N, Ikawa K, Karino F, Miura K, Tamaki H, et al. Population pharmacokinetic modeling and pharmacodynamic target attainment simulation of piperacillin/tazobactam for dosing optimization in late elderly patients with pneumonia. Antibiotics (Basel). 2020;9(3):113.
Karino F, Nishimura N, Ishihara N, Moriyama H, Miura K, Hamaguchi S, et al. Nephrotoxicity induced by piperacillin-tazobactam in late elderly Japanese patients with nursing and healthcare associated pneumonia. Biol Pharm Bull. 2014;37(12):1971–6.
Ball AP, Viswan AK, Mitchard M, Wise R. Plasma concentrations and excretion of mecillinam after oral administration of pivmecillinam in elderly patients. J Antimicrob Chemother. 1978;4(3):241–6.
Simon C, Malerczyk V, Tenschert B, Moehlenbeck F. Geriatric pharmacology of cefazolin, cefradine and sulfisomidine. Arzneimittelforschung. 1976;26(7):1377–82.
Broekhuysen J, Deger F, Douchamps J, Freschi E, Mal N, Neve P, et al. Pharmacokinetic study of cefuroxime in the elderly. Br J Clin Pharmacol. 1981;12(6):801–5. https://doi.org/10.1111/j.1365-2125.1981.tb01310.x.
Naber K. Cefuroxime: Pharmacokinetics in geriatric patients and results in complicated urinary tract infections. Therapiewoche. 1979;29(37):5944–53.
Douglas JG, Bax RP, Munro JF. The pharmacokinetics of cefuroxime in the elderly. J Antimicrob Chemother. 1980;6(4):543–9. https://doi.org/10.1093/jac/6.4.543.
Ridgway E, Stewart K, Rai G, Kelsey MC, Bielawska C. The pharmacokinetics of cefuroxime axetil in the sick elderly patient. J Antimicrob Chemother. 1991;27(5):663–8. https://doi.org/10.1093/jac/27.5.663.
Veyssier P, Darchis JP, Devillers A. Pharmacokinetics of cefuroxime-axetil administered by the oral route in the elderly. Therapie. 1988;43:355–9.
Schött D, Micklefield GH, Zimmermann I, Ritzerfeld W, Ulmer WT. Pharmacokinetics of cefuroxime axetil in elderly patients with lower respiratory tract infections. ATEMWEGS- LUNGENKR. 1991;17(1):29–30.
Renneberg J, Christensen OM, Thomsen NO, Tørholm C. Cefuroxime concentrations in serum, joint fluid and bone in elderly patients undergoing arthroplasty after administration of cefuroxime axetil. J Antimicrob Chemother. 1993;32(5):751–5. https://doi.org/10.1093/jac/32.5.751.
Faulkner RD, Bohaychuk W, Lanc RA, Haynes JD, Desjardins RE, Yacobi A, et al. Pharmacokinetics of cefixime in the young and elderly. J Antimicrob Chemother. 1988;21(6):787–94.
Deeter RG, Weinstein MP, Swanson KA, Gross JS, Bailey LC. Crossover assessment of serum bactericidal activity and pharmacokinetics of five broad-spectrum cephalosporins in the elderly. Antimicrob Agents Chemother. 1990;34(6):1007–13. https://doi.org/10.1128/AAC.34.6.1007.
Grabe M, Andersson KE, Forsgren A, Hellsten S. Concentrations of cefotaxime in serum, urine and tissues of urological patients. Infection. 1981;9(3):154–8.
Urien S, Laurent N, Barre J, Druguet M, Bouvier D’Yvoire M, Maire P. Pharmacokinetic modelling of cefotaxime and desacetylcefotaxime—a population study in 25 elderly patients. Eur J Clin Pharmacol. 2004;60(1):11–6. https://doi.org/10.1007/s00228-003-0725-9.
Ludwig E, Székely E, Csiba A, Graber H. Pharmacokinetics of cefotaxime and desacetylcefotaxime in elderly patients. Drugs. 1988;35:51–6. https://doi.org/10.2165/00003495-198800352-00012.
Jonsson M, Walder M. Pharmacokinetics of intravenous antibiotics in acutely ill elderly patients. Eur J Clin Microbiol. 1986;5(6):629–33. https://doi.org/10.1007/BF02013286.
Sugihara H, Yoneyama K, Sorimachi H, Kamo T, Imamura S, Akashi N, et al. Pharmacokinetics of cefotaxime in elderly patients. Drugs. 1988;35:93–6. https://doi.org/10.2165/00003495-198800352-00020.
Naber K, Adam D. Pharmacokinetics of cefotaxime in geriatric patients [in German]. Münchener Medizinische Wochenschrift. 1980;122(46):1651–4.
Mühlberg W, Platt D. Elimination of desacetyl cefotaxime in geriatric patients with multiple diseases [in German]. Klin Wochenschr. 1982;60(24):1497–500. https://doi.org/10.1007/BF01716101.
Borin MT, Ferry JJ, Forbes KK, Hughes GS. Pharmacokinetics of cefpodoxime proxetil in healthy young and elderly volunteers. J Clin Pharmacol. 1994;34(7):774–81.
Tremblay D, Dupront A, Ho C, Coussediere D, Lenfant B. Pharmacokinetics of cefpodoxime in young and elderly volunteers after single doses. J Antimicrob Chemother. 1990;26 Suppl E:21–8.
Ishioka T. Pharmacokinetic study and clinical evaluation of cefpodoxime proxetil in the elderly with impaired renal function. J Chemother. 1995;7:122–3.
Backhouse C, Wade A, Williamson P, Tremblay D, Lenfant B. Multiple dose pharmacokinetics of cefpodoxime in young adult and elderly patients. J Antimicrob Chemother. 1990;26 Suppl E:29–34.
Ljungberg B, Nilsson-Ehle I. Pharmacokinetics of ceftazidime in elderly patients and young volunteers. Scand J Infect Dis. 1984;16(3):325–6. https://doi.org/10.3109/00365548409070410.
Naber KG, Kees F, Grobecker H. Ceftazidime: Pharmacokinetics in young volunteers versus elderly patients and therapeutic efficacy with complicated urinary tract infections. J Antimicrob Chemother. 1983;12:41–5.
Higbee MD, Swenson E, Gooch WM 3rd. Pharmacokinetics of ceftazidime in elderly patients. Clin Pharm. 1989;8(1):59–62.
Ljungberg B, Nilsson-Ehle I. Influence of age on the pharmacokinetics of ceftazidime in acutely ill, adult patients. Eur J Clin Pharmacol. 1988;34(2):173–8.
Li J, Lovern M, Green ML, Chiu J, Zhou D, Comisar C, et al. Ceftazidime-avibactam population pharmacokinetic modeling and pharmacodynamic target attainment across adult indications and patient subgroups. Clin Transl Sci. 2019;12(2):151–63.
Jonsson M, Walder M. Pharmacokinetics of ceftazidime in acutely ill hospitalised elderly patients. Eur J Clin Microbiol Infect Dis. 1992;11(1):15–21. https://doi.org/10.1007/bf01971265.
Radwanski E, Teal M, Affrime M, Cayen M, Lin CC. Multiple-dose pharmacokinetics of ceftibuten in healthy adults and geriatric volunteers. Am J Ther. 1994;1(1):42–8. https://doi.org/10.1097/00045391-199406000-00008.
Luderer JR, Pael IH, Durkin J, Schneck DW. Age and ceftriaxone kinetics. Clin Pharmacol Ther. 1984;35(1):19–25. https://doi.org/10.1038/clpt.1984.3.
Geny F, Costa P, Bressolle F, Galtier M. Ceftriaxone pharmacokinetics in elderly subjects and penetration into epididymis. Biopharm Drug Dispos. 1993;14(2):161–9.
Melin-Coviaux F, Hary L, Hurtel AS, Andrejak M, Grumbach Y. A comparative pharmaco-clinic study of ceftriaxone after subcutaneous and intravenous administration in the elderly [in French]. Revue de Geriatrie. 2000;25(5):337–47.
Barbhaiya RH, Knupp CA, Pittman KA. Effects of age and gender on pharmacokinetics of cefepime. Antimicrob Agents Chemother. 1992;36(6):1181–5. https://doi.org/10.1128/aac.36.6.1181.
Pilmis B, Mizrahi A, Petitjean G, Le Monnier A, El Helali N. Clinical evaluation of subcutaneous administration of cefepime [in French]. Med Mal Infect. 2020;50(3):308–10. https://doi.org/10.1016/j.medmal.2019.12.006.
Riccobene T, Jakate A, Rank D. A series of pharmacokinetic studies of ceftaroline fosamil in select populations: Normal subjects, healthy elderly subjects, and subjects with renal impairment or end-stage renal disease requiring hemodialysis. J Clin Pharmacol. 2014;54(7):742–52. https://doi.org/10.1002/jcph.265.
Garcia MJ, Garcia A, Nieto MJ. Disposition of cefoxitin in the elderly. Int J Clin Pharmacol Ther Toxicol. 1980;18(11):503–9.
Roubaud Baudron C, Legeron R, Ollivier J, Bonnet F, Greib C, Guerville F, et al. Is the subcutaneous route an alternative for administering ertapenem to older patients? PHACINERTA study. J Antimicrob Chemother. 2019;74(12):3546–54. https://doi.org/10.1093/jac/dkz385.
Musson DG, Majumdar A, Holland S, Birk K, Xi L, Mistry G, et al. Pharmacokinetics of total and unbound ertapenem in healthy elderly subjects. Antimicrob Agents Chemother. 2004;48(2):521–4.
Finch RG, Craddock C, Kelly J, Deaney NB. Pharmacokinetic studies of imipenem/cilastatin in elderly patients. J Antimicrob Chemother. 1986;18:103–7. https://doi.org/10.1093/jac/18.supplement_e.103.
Pietroski NA, Graziani AL, Lawson LA, Bland JA, Rogers JD, MacGregor RR. Steady-state pharmacokinetics of intramuscular imipenem-cilastatin in elderly patients with various degrees of renal function. Antimicrob Agents Chemother. 1991;35(5):972–5. https://doi.org/10.1128/AAC.35.5.972.
Zhou QT, He B, Zhang C, Zhai SD, Liu ZY, Zhang J. Pharmacokinetics and pharmacodynamics of meropenem in elderly Chinese with lower respiratory tract infections: Population pharmacokinetics analysis using nonlinear mixed-effects modelling and clinical pharmacodynamics study. Drugs Aging. 2011;28(11):903–12. https://doi.org/10.2165/11595960-000000000-00000.
Ljungberg B, Nilsson-Ehle I. Pharmacokinetics of meropenem and its metabolite in young and elderly healthy men. Antimicrob Agents Chemother. 1992;36(7):1437–40.
Zhou QT, He B, Shen N, Liang Y, Sun LN. Meropenem dosing based on a population pharmacokinetic-pharmacodynamic model in elderly patients with infection of the lower respiratory tract. Drugs Aging. 2017;34(2):115–21. https://doi.org/10.1007/s40266-016-0431-9.
Ikawa K, Nakashima A, Morikawa N, Ikeda K, Murakami Y, Ohge H, et al. Clinical pharmacokinetics of meropenem and biapenem in bile and dosing considerations for biliary tract infections based on site-specific pharmacodynamic target attainment. Antimicrob Agents Chemother. 2011;55(12):5609–15. https://doi.org/10.1128/AAC.00497-11.
Aimiya K, Mamiya T, Tabuchi K, Kita T, Hiramatsu M. Comparison of twice a day and three times a day meropenem administration in elderly patients in a Japanese community hospital. Nagoya J Med Sci. 2018;80(3):391–400. https://doi.org/10.18999/nagjms.80.3.391.
Meyers BR, Wilkinson P, Mendelson MH, Bournazos C, Tejero C, Hirschman SZ. Pharmacokinetics of aztreonam in healthy elderly and young adult volunteers. J Clin Pharmacol. 1993;33(5):470–4.
Naber KG, Dette GA, Kees F, Knothe H, Grobecker H. Pharmacokinetics, in-vitro activity, therapeutic efficacy and clinical safety of aztreonam vs. cefotaxime in the treatment of complicated urinary tract infections. J Antimicrob Chemother. 1986;17(4):517–27.
Creasey WA, Platt TB, Frantz M, Sugerman AA. Pharmacokinetics of aztreonam in elderly male volunteers. Br J Clin Pharmacol. 1985;19(2):233–7.
Keij FM, Tramper-Stranders GA, Koch BCP, Reiss IKM, Muller AE, Kornelisse RF, et al. Pharmacokinetics of clavulanic acid in the pediatric population: a systematic literature review. Clin Pharmacokinet. 2022;61(5):637–53. https://doi.org/10.1007/s40262-022-01116-3.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. https://doi.org/10.1159/000180580.
Silva MA, Dias G, Cardoso T. Correlation of estimated creatinine clearance and glomerular filtration rate in very elderly patients and antibiotic prescribing errors: Cohort study. Acta Med Port. 2021;34(5):335–41.
McCue JD. Antimicrobial therapy. Clin Geriatr Med. 1992;8(4):925–45.
Schwinghammer TL, Norden CW, Gill E. Pharmacokinetics of cephradine administered intravenously and orally to young and elderly subjects. J Clin Pharmacol. 1990;30(10):893–9.
Drenth-van Maanen AC, Wilting I, Jansen PAF. Prescribing medicines to older people-How to consider the impact of ageing on human organ and body functions. Br J Clin Pharmacol. 2020;86(10):1921–30. https://doi.org/10.1111/bcp.14094.
Johnston C, Hilmer SN, McLachlan AJ, Matthews ST, Carroll PR, Kirkpatrick CM. The impact of frailty on pharmacokinetics in older people: using gentamicin population pharmacokinetic modeling to investigate changes in renal drug clearance by glomerular filtration. Eur J Clin Pharmacol. 2014;70(5):549–55. https://doi.org/10.1007/s00228-014-1652-7.
Hilmer SN, Kirkpatrick CMJ. New Horizons in the impact of frailty on pharmacokinetics: latest developments. Age Ageing. 2021;50(4):1054–63. https://doi.org/10.1093/ageing/afab003.
The Geriatric Expert Group of the European Medicine Agency. Reflection paper on physical frailty: instruments for baseline characterisation of older populations in clinical trials. EMA. 2021. https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-physical-frailty-instruments-baseline-characterisation-older-populations-clinical_en.pdf. Accessed 14 Oct 2022.
Q. Mattingly commissioned by the World Health Organization. Health Topics: Antimicrobial Resistance. 2021. https://www.who.int/health-topics/antimicrobial-resistance. Accessed 14 Sept 2022.
European Medicines Agency. Committee for Medicinal Products for Human Use. Guideline on the use of pharmacokinetics and pharmacodynamics in the development of antimicrobial medicinal products. 2016. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-use-pharmacokinetics-pharmacodynamics-development-antimicrobial-medicinal-products_en.pdf. Accessed 14 Sept 2022.
Meyers BR, Mendelson MH, Deeter RG, Srulevitch-Chin E, Sarni MT, Hirschman SZ. Pharmacokinetics of cefoperazone in ambulatory elderly volunteers compared with young adults. Antimicrob Agents Chemother. 1987;31(6):925–9.
Rho JP, Castle S, Smith K, Bawdon RE, Norman DC. Effect of age and renal function on the pharmacokinetics of coadministered cefoperazone and sulbactam. Drug Invest. 1993;6(6):303–10.
Meyers BR, Mendelson MH, Srulevitch-Chin E, Bradbury K, McMurdo L, Hirschman SZ. Pharmacokinetic properties of mezlocillin in ambulatory elderly subjects. J Clin Pharmacol. 1987;27(9):678–81.
Aboulatta L, Sugita H, Wakabayashi H, Noma H, Sasaki T. Comparison of extended versus intermittent infusion of antipseudomonal beta-lactams for the treatment of critically ill patients with respiratory infections: a systematic review and meta-analysis. Int J Infect Dis. 2020;98:41–50. https://doi.org/10.1016/j.ijid.2020.06.022.
Gabriel J. Understanding the challenges to vascular access in an ageing population. Br J Nurs. 2017;26(14):S15-s23. https://doi.org/10.12968/bjon.2017.26.14.S15.
Kato M, Fauziah W, Koesnadi H, Nishijima S, Kima M, Iida M, Pham HTT. Prevalence and prevention of unplanned removal of tubes and catheters among hospitalized patients. Int J Caring Sci. 2021;14(1):385–91.
Jung H, Park HA, Lee HY. Comparisons of fall prevention activities using electronic nursing records: a case-control study. J Patient Saf. 2022;18(3):145–51. https://doi.org/10.1097/pts.0000000000000930.
Hailu BY, Berhe DF, Gudina EK, Gidey K, Getachew M. Drug related problems in admitted geriatric patients: the impact of clinical pharmacist interventions. BMC Geriatr. 2020;20(1):13. https://doi.org/10.1186/s12877-020-1413-7.
Jonsson TB, Nilsson TK, Breimer LH, Schneede J, Arfvidsson B, Norgren L. Cloxacillin concentrations in serum, subcutaneous fat, and muscle in patients with chronic critical limb ischemia. Eur J Clin Pharmacol. 2014;70(8):957–63.
Lofgren S, Bucht G, Hermansson B. Single-dose pharmacokinetics of dicloxacillin in healthy subjects of young and old age. Scand J Infect Dis. 1986;18(4):365–9.
Mellin HE, Welling PG, Madsen PO. Pharmacokinetics of cefamandole in patients with normal and impaired renal function. Antimicrob Agents Chemother. 1977;11(2):262–6. https://doi.org/10.1128/aac.11.2.262.
Borin MT, Peters GR, Smith TC. Pharmacokinetics and dose proportionality of cefmetazole in healthy young and elderly volunteers. Antimicrob Agents Chemother. 1990;34(10):1944–8.
Trang JM, Monson TP, Ackerman BH, Underwood FL, Manning JT, Kearns GL. Effect of age and renal function on cefonicid pharmacokinetics. Antimicrob Agents Chemother. 1989;33(2):142–6.
Karki SD, Bentley DW, Luzier A, Taylor C, Morse GD. Disposition of intramuscular cefonicid in elderly patients. J Am Geriatr Soc. 1993;41(8):808–10. https://doi.org/10.1111/j.1532-5415.1993.tb06174.x.
Gaillat J, Croize J, Bru JP, Stahl JP, Le Noc P, Micoud M. Cefotetan: clinical trial in elderly persons using a single daily dose of 2 grams as the sole therapy [in French]. Pathol Biol (Paris). 1986;34(5):461–4.
Ripa S, Mignini F, Prenna M. Pharmacokinetics of cefotetan in elderly subjects after intramuscular administration. Chemioterapia. 1987;6(5):359–63.
Blouin RA, Kneer J, Stoeckel K. Pharmacokinetics of intravenous cefetamet (Ro 15–8074) and oral cefetamet pivoxil (Ro 15–8074) in young and elderly subjects. Antimicrob Agents Chemother. 1989;33(3):291–6. https://doi.org/10.1128/AAC.33.3.291.
Veyssier P, Bryskier A, Modai J. Pharmacokinetics of cefmenoxime in elderly patients (60 to 90 years old) after 1 g IV bolus [in French]. Pathol Biol (Paris). 1986;34(10):1081–3.
Nilsen OG, Rennemo F, Rennemo R, Lenfant B. Pharmacokinetics of cefodizime in the elderly following single and repeated intravenous administration of 1 g. J Antimicrob Chemother. 1990;26 Suppl C:71–5.
Veyssier P, Devillers A, Domart Y, Fourtillan JB, Bryskier A, Procyk T. Pharmacokinetics of cefodizime in elderly patients with moderate or severe renal impairment. J Amtimicrob Chemother. 1990;26 Suppl C:77–81.
Schwartz JI, Jauregui LE, Bachmann KA, Martin ME, Reitberg DP. Multiple-dose pharmacokinetics of intravenously administered cefoperazone and sulbactam when given in combination to infected, seriously ill, elderly patients. Antimicrob Agents Chemother. 1988;32(5):730–5. https://doi.org/10.1128/AAC.32.5.730.
Wittmann DH, Schassan HH. Distribution of moxalactam in serum, bone, tissue fluid, and peritoneal fluid. Rev Infect Dis. 1982;4:S610–6. https://doi.org/10.1093/clinids/4.supplement_3.s610.
Andritz MH, Smith RP, Baltch AL, Griffin PE, Conroy JV, Sutphen N, et al. Pharmacokinetics of moxalactam in elderly subjects. Antimicrob Agents Chemother. 1984;25(1):33–6. https://doi.org/10.1128/aac.25.1.33.
Sugihara H, Narita N, Takatsu R, Horiuchi M, Yonenami K, Hotta M, et al. Study of the pharmacokinetics of cefpirome sulphate in the elderly. J Clin Pharm Ther. 1998;23(5):375–9. https://doi.org/10.1046/j.1365-2710.1998.00176.x.
Kozawa O, Uematsu T, Matsuno H, Niwa M, Takiguchi Y, Matsumoto S, et al. Pharmacokinetics and safety of a new parenteral carbapenem antibiotic, biapenem (L-627), in elderly subjects. Antimicrob Agents Chemother. 1998;42(6):1433–6. https://doi.org/10.1128/aac.42.6.1433.
Karino F, Deguchi N, Kanda H, Ohe M, Kondo K, Tada M, et al. Evaluation of the efficacy and safety of biapenem against pneumonia in the elderly and a study on its pharmacokinetics. J Infect Chemother. 2013;19(1):98–102. https://doi.org/10.1007/s10156-012-0463-y.
Namkoong H, Kameyama Y, Yasuda H, Nakayama S, Kaneko H, Kawashima C, et al. The efficacy, safety, and pharmacokinetics of biapenem administered thrice daily for the treatment of pneumonia in the elderly. J Infect Chemother. 2014;20(6):356–60. https://doi.org/10.1016/j.jiac.2013.12.010.
Harada M, Inui N, Suda T, Nakamura Y, Wajima T, Matsuo Y, et al. Pharmacokinetic analysis of doripenem in elderly patients with nosocomial pneumonia. Int J Antimicrob Agents. 2013;42(2):149–54. https://doi.org/10.1016/j.ijantimicag.2013.03.012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest/competing interests
Jeroen Vervalcke, Arnaud De Clercq, Peter De Paepe, Mirko Petrovic, Tania Desmet, and Pieter A. De Cock declare they have no conflicts of interest in relation to this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
PADC, PDP, MP and TD provided the concept for this systematic review. JV, ADC and PADC performed the literature search and data analysis. JV, ADC, and PADC drafted the original manuscript, and PDP, MP and TD critically reviewed and edited the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vervalcke, J., De Clercq, A., De Paepe, P. et al. Pharmacokinetics and Target Attainment of ß-lactam Antibiotics in Older People: A Systematic Review of Current Literature. Clin Pharmacokinet 62, 1–43 (2023). https://doi.org/10.1007/s40262-022-01196-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01196-1