Abstract
Background
Fat-free mass has gained wide acceptance as a scaler of the maintenance dose rate in obese patients. The choice of fat-free mass as a size scaler for the maintenance dose rate is based on its relationship with drug clearance, on the basis that only lean tissue is sufficiently metabolically active to provide capacity for elimination. For xenobiotics, the majority of biotransformation occurs in the liver and hence fat-free mass is implied to scale linearly with the component of liver that is metabolically active. The liver, like the body, can be assumed to comprise two components, lean mass and fat mass. We expect the lean liver mass (or volume) to be the component that most closely relates to drug clearance.
Objective
The objective of this study was to investigate the relationship of lean liver volume and fat-free mass.
Methods
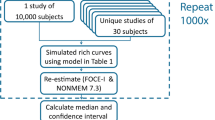
Total liver volume and liver fat volume were measured in 100 Indian adults by computed tomography. Lean liver volume was derived as the difference between the two measurements (as liver volume − liver fat volume). Covariate modelling to describe lean liver volume, using NONMEM version 7.3, involved testing the influence of body weight, sex, body surface area and fat-free mass with or without allometric scaling (by estimating the exponent) and the influence of clinical chemistry variables.
Results
The final model did not exclude a linear relationship between lean liver volume and fat-free mass, while allometric scaling by body weight0.75 was also supported by the data. While scaling by fat-free mass, the coefficient of proportionality (i.e. lean liver volume per kg fat-free mass) was higher in female (31.25 mL) than male (25.81 mL) subjects.
Conclusions
A model to predict lean liver volume from readily available patient data was developed and evaluated. Fat-free mass plus sex was found to be the best body descriptor to scale lean liver volume. The utility of this model in scaling drug clearance and dose requirements of hepatically cleared drugs needs further exploration.



Similar content being viewed by others
References
Collaboration NRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96.
Prospective Studies C. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Leykin Y, Miotto L, Pellis T. Pharmacokinetic considerations in the obese. Best Pract Res Clin Anaesthesiol. 2011;25(1):27–36.
Blouin RA, Warren GW. Pharmacokinetic considerations in obesity. J Pharm Sci. 1999;88(1):1–7.
Cheymol G. Effects of obesity on pharmacokinetics. Clin Pharmacokinet. 2000;39(3):215–31.
Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet. 2010;49(2):71–87.
Green B, Duffull SB. What is the best size descriptor to use for pharmacokinetic studies in the obese? Br J Clin Pharmacol. 2004;58(2):119–33.
De Baerdemaeker LE, Mortier EP, Struys MM. Pharmacokinetics in obese patients. Contin Educ Anaesth Crit Care Pain. 2004;4(5):152–5.
Han P, Duffull S, Kirkpatrick C, Green B. Dosing in obesity: a simple solution to a big problem. Clin Pharmacol Ther. 2007;82(5):505–8.
Eleveld DJ, Proost JH, Absalom AR, Struys MM. Obesity and allometric scaling of pharmacokinetics. Clin Pharmacokinet. 2011;50(11):751–3.
De Baerdemaeker LEC, Van Limmen JGM, Van Nieuwenhove Y. How should obesity be measured and how should anesthetic drug dosage be calculated? In: Leykin Y, Brodsky JB, editors. Controversies in the anesthetic management of the obese surgical patient. Milan: Springer; 2013. p. 15–30.
Ingrande J, Brodsky JB, Lemmens HJ. Lean body weight scalar for the anesthetic induction dose of propofol in morbidly obese subjects. Anesth Analg. 2011;113(1):57–62.
Cortinez LI, Anderson BJ, Holford NH, Puga V, de la Fuente N, Auad H, et al. Dexmedetomidine pharmacokinetics in the obese. Eur J Clin Pharmacol. 2015;71(12):1501–8.
La Colla L, Albertin A, La Colla G, Porta A, Aldegheri G, Di Candia D, et al. Predictive performance of the ‘Minto’ remifentanil pharmacokinetic parameter set in morbidly obese patients ensuing from a new method for calculating lean body mass. Clin Pharmacokinet. 2010;49(2):131–9.
Morgan DJ, Bray KM. Lean body mass as a predictor of drug dosage. Clin Pharmacokinet. 1994;26(4):292–307.
McLeay SC, Morrish GA, Kirkpatrick CM, Green B. The relationship between drug clearance and body size. Clin Pharmacokinet. 2012;51(5):319–30.
Verbeeck RK. Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol. 2008;64(12):1147–61.
Homeida M, Roberts C, Halliwell M, Read A, Branch R. Antipyrine clearance per unit volume liver: an assessment of hepatic function in chronic liver disease. Gut. 1979;20(7):596–601.
Knibbe CA, Brill MJ, van Rongen A, Diepstraten J, van der Graaf PH, Danhof M. Drug disposition in obesity: toward evidence-based dosing. Ann Rev Pharmacol Toxicol. 2015;55:149–67.
van Rongen A, Brill MJE, Diepstraten J, Knibbe CAJ. Applied pharmacometrics in the obese population. In: Schmidt S, Derendorf H, editors. Applied pharmacometrics. New York: Springer; 2014. p. 161–87.
Riede U, Spycher M, Gitzelmann R. Glycogenosis type I (glucose 6-phosphatase deficiency): I. Ultrastructural morphometric analysis of juvenile liver cells. Pathol Res Pract. 1980;167(1):136–50.
Rohr H, Lüthy J, Gudat F, Oberholzer M, Gysin C, Bianchi L. Stereology of liver biopsies from healthy volunteers. Virchows Arch A Pathol Anat Histol. 1976;371(3):251–63.
Marceau P, Biron S, Hould F-S, Marceau S, Simard S, Thung S, et al. Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab. 1999;84(5):1513–7.
Merrell MD, Cherrington NJ. Drug metabolism alterations in nonalcoholic fatty liver disease. Drug Metab Rev. 2011;43(3):317–34.
Idilman IS, Keskin O, Celik A, Savas B, Halil Elhan A, Idilman R, et al. A comparison of liver fat content as determined by magnetic resonance imaging-proton density fat fraction and MRS versus liver histology in non-alcoholic fatty liver disease. Acta Radiol. 2016;57(3):271–8.
Noureddin M, Lam J, Peterson MR, Middleton M, Hamilton G, Le TA, et al. Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials. Hepatology. 2013;58(6):1930–40.
Szczepaniak LS, Nurenberg P, Leonard D, Browning JD, Reingold JS, Grundy S, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol Endocrinol Metab. 2005;288(2):E462–8.
McLeay S, Morrish G, Ponnuswamy T, Devanand B, Ramanathan M, Venkatakrishnan L, et al. Noninvasive quantification of hepatic steatosis: relationship between obesity status and liver fat content. Open Obesity J. 2014;6(1):16–24.
Janmahasatian S, Duffull SB, Ash S, Ward LC, Byrne NM, Green B. Quantification of lean bodyweight. Clin Pharmacokinet. 2005;44(10):1051–65.
Kulkarni B, Kuper H, Taylor A, Wells JC, Radhakrishna KV, Kinra S, et al. Development and validation of anthropometric prediction equations for estimation of lean body mass and appendicular lean soft tissue in Indian men and women. J Appl Physiol. 2013;115(8):1156–62.
Chandan Vinay S, Urooj A, Chaya Sindaghatta K, Mahesh P. Validation of fat-free mass estimation using prediction equations in male patients with chronic obstructive pulmonary disease. Int J Nutr Pharmacol Neurol Dis. 2017;7(4):94–100.
Du Bois D. A formula to estimate the approximate surface area if height and weight be known. Nutrition. 1989;5:303–13.
Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19(6):716–23.
Sinha J, Al-Sallami HS, Duffull SB. Choosing the allometric exponent in covariate model building. Clin Pharmacokinet. 2019;58(1):89–100.
Ribbing J, Jonsson EN. Power, selection bias and predictive performance of the population pharmacokinetic covariate model. J Pharmacokinet Pharmacodyn. 2004;31(2):109–34.
Krovetz LJ. The physiologic significance of body surface area. J Pediatr. 1965;67(5):841–62.
Sawyer M, Ratain MJ. Body surface area as a determinant of pharmacokinetics and drug dosing. Invest New Drugs. 2001;19(2):171–7.
Holliday MA, Potter D, Jarrah A, Bearg S. The relation of metabolic rate to body weight and organ size. Pediatr Res. 1967;1:185–95.
Johnson TN, Tucker GT, Tanner MS, Rostami-Hodjegan A. Changes in liver volume from birth to adulthood: a meta-analysis. Liver Transpl. 2005;11(12):1481–93.
Johnstone AM, Murison SD, Duncan JS, Rance KA, Speakman JR. Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine. Am J Clin Nutr. 2005;82(5):941–8.
Weinsier RL, Schutz Y, Bracco D. Reexamination of the relationship of resting metabolic rate to fat-free mass and to the metabolically active components of fat-free mass in humans. Am J Clin Nutr. 1992;55(4):790–4.
Holliday MA. Body composition and energy needs during growth. In: Falkner F, Tanner JM, editors. Postnatal growth neurobiology. Boston: Springer; 1986. p. 101–17.
West GB, Brown JH, Enquist BJ. A general model for the origin of allometric scaling laws in biology. Science. 1997;276(5309):122–6.
Howgate EM, Rowland Yeo K, Proctor NJ, Tucker GT, Rostami-Hodjegan A. Prediction of in vivo drug clearance from in vitro data. I: Impact of inter-individual variability. Xenobiotica. 2006;36(6):473–97.
Wilson ZE, Rostami-Hodjegan A, Burn JL, Tooley A, Boyle J, Ellis SW, et al. Inter-individual variability in levels of human microsomal protein and hepatocellularity per gram of liver. Br J Clin Pharmacol. 2003;56(4):433–40.
Zhang H, Gao N, Tian X, Liu T, Fang Y, Zhou J, et al. Content and activity of human liver microsomal protein and prediction of individual hepatic clearance in vivo. Sci Rep. 2015;5:17671.
Achour B, Barber J, Rostami-Hodjegan A. Expression of hepatic drug-metabolizing cytochrome P450 enzymes and their intercorrelations: a meta-analysis. Drug Metab Dispos. 2014;42(8):1349–56.
Chul YH, Heecheon Y, Ho L, Zhe-Wu J, Il MJ, Hwan CB. Estimation of standard liver volume for liver transplantation in the Korean population. Liver Transpl. 2004;10(6):779–83.
Vauthey JN, Abdalla EK, Doherty DA, Gertsch P, Fenstermacher MJ, Loyer EM, et al. Body surface area and body weight predict total liver volume in Western adults. Liver Transpl. 2002;8(3):233–40.
Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Sun Q, et al. Development and validation of anthropometric prediction equations for lean body mass, fat mass and percent fat in adults using the National Health and Nutrition Examination Survey (NHANES) 1999–2006. Br J Nutr. 2017;118(10):858–66.
Kwo PY, Ramchandani VA, O’Connor S, Amann D, Carr LG, Sandrasegaran K, et al. Gender differences in alcohol metabolism: relationship to liver volume and effect of adjusting for body mass. Gastroenterology. 1998;115(6):1552–7.
Jones HM, Rowland-Yeo K. Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development. CPT Pharmacomet Syst Pharmacol. 2013;2(8):e63.
Marsousi N, Desmeules JA, Rudaz S, Daali Y. Usefulness of PBPK modeling in incorporation of clinical conditions in personalized medicine. J Pharm Sci. 2017;106(9):2380–91.
Ghobadi C, Johnson TN, Aarabi M, Almond LM, Allabi AC, Rowland-Yeo K, et al. Application of a systems approach to the bottom-up assessment of pharmacokinetics in obese patients. Clin Pharmacokinet. 2011;50(12):809–22.
Cassidy S, Syed BA. Nonalcoholic steatohepatitis (NASH) drugs market. Nat Rev Drug Discov. 2016;15(11):745–6.
Konerman MA, Jones JC, Harrison SA. Pharmacotherapy for NASH: current and emerging. J Hepatol. 2018;68(2):362–75.
Acknowledgements
The authors acknowledge the contribution of T.K. Ponnuswamy, B. Devanand, M. Ramanathan and S. Ramalingam for generating the LLV data. T.K. Ponnuswamy, B. Devanand and S. Ramalingam were from the PSG Institute of Medical Sciences and Research, Coimbatore, India, and M. Ramanathan was from the PSG College of Pharmacy, Coimbatore, India during the conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work required no specific funding. Jaydeep Sinha received a doctoral scholarship from the School of Pharmacy, University of Otago, New Zealand during this work.
Conflict of interest
Jaydeep Sinha, Stephen B. Duffull, Bruce Green and Hesham S. Al-Sallami have no conflicts of interest that are directly relevant to the content of this study.
Ethics approval
No ethics approval was required for this analysis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sinha, J., Duffull, S.B., Green, B. et al. Evaluating the Relationship Between Lean Liver Volume and Fat-Free Mass. Clin Pharmacokinet 59, 475–483 (2020). https://doi.org/10.1007/s40262-019-00824-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-019-00824-7