Abstract
Background and Objective
The number of hospitalizations due to opioid use disorders in the USA increased steadily from 62,010 in 1998–2000 to 136,240 in 2015–2016; however, no health care utilization of lung cancer patients with opioid use disorder has been reported. The purpose of this paper is to investigate health care utilization due to opioid use disorder among lung cancer patients and to investigate additional charge status due to this disorder.
Methods
The National Inpatient Sample of the USA was used to identify lung cancer patients (n = 11,418, weighted n = 557,090) from 2016 to 2020. The characteristics of patient samples, temporal trend of opioid use disorder, and its association with health care utilization measured by hospital charges were thoroughly examined by the multivariate survey linear regression model.
Results
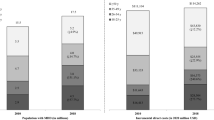
Among 557,090 lung cancer patients, 2.4% had opioid use disorder. The proportion of opioid use disorder among lung cancer patients during the study periods had continuously grown. Hospital charges also continued to increase during the study period and were higher among lung cancer patients with opioid use disorder. Survey linear results showed that opioid use disorder was associated with 12.6% higher hospital charges. Analysis of subgroups revealed that this trend was similar across p < the majority of social groups; however, it was significantly higher among Caucasian individuals (0.001) and self-pay groups (p = 0.035) than among others.
Conclusions
Research conducted has identified gaps in care in rural and suburban areas and a lack of equal care given to minority and low-income patients. These vulnerable groups access health care less often, are charged more for the care they receive, and often face multiple barriers to treatment. Unless these issues are addressed with a focus on socioeconomic factors, race, and region, the opioid epidemic will continue to negatively decimate these populations.

Similar content being viewed by others
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. Ca Cancer J Clin. 2023;73(1):17–48.
Mercadante S, Vitrano V. Pain in patients with lung cancer: pathophysiology and treatment. Lung Cancer. 2010;68(1):10–5.
Tomaszewski KA, Püsküllüoğlu M, Biesiada K, Bochenek J, Nieckula J, Krzemieniecki K. Validation of the polish version of the eortc QLQ-C30 and the QLQ-OG25 for the assessment of health-related quality of life in patients with esophagi-gastric cancer. J Psychosoc Oncol. 2013;31(2):191–203.
Polanski J, Jankowska-Polanska B, Rosinczuk J, Chabowski M, Szymanska-Chabowska A. Quality of life of patients with lung cancer. OncoTargets Ther. 2016;9:1023–28.
Schofield P, Ugalde A, Carey M, Mileshkin L, Duffy M, Ball D, et al. Lung cancer: challenges and solutions for supportive care intervention research. Palliat Support Care. 2008;6(3):281–7.
Potter J, Higginson IJ. Pain experienced by lung cancer patients: a review of prevalence, causes and pathophysiology. Lung Cancer. 2004;43(3):247–57.
Mystakidou K, Parpa E, Tsilika E, Pathiaki M, Galanos A, Vlahos L. Comparison of pain quality descriptors in cancer patients with nociceptive and neuropathic pain. In Vivo. 2007;21(1):93–7.
WHO Guidelines for the Pharmacological and Radiotherapeutic Management of Cancer Pain in Adults and Adolescents. Geneva: World Health Organization; 2018.
Schuckit MA. Treatment of opioid-use disorders. N Engl J Med. 2016;375(4):357–68.
Blanco C, Volkow ND. Management of opioid use disorder in the USA: present status and future directions. The Lancet. 2019;393(10182):1760–72.
Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286–93.
Barnett ML, Olenski AR, Jena AB. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. 2017;376(7):663–73.
Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293–301.
Jones CM. The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence—An assessment of demographic and substance use trends, United States, 2003–2014. Addict Behav. 2017;65:229–35.
Schiff DM, Work EC, Foley B, Applewhite R, Diop H, Goullaud L, et al. Perinatal opioid use disorder research, race, and racism: a scoping review. Pediatrics. 2022;149(3):e2021052368.
Arthur J, Bruera E. Balancing opioid analgesia with the risk of nonmedical opioid use in patients with cancer. Nat Rev Clin Oncol. 2019;16(4):213–26.
Lipari RN, Hughes A. How people obtain the prescription pain relievers they misuse. In: The CBHSQ Report. Substance Abuse and Mental Health Services Administration (US), Rockville (MD); 2013.
Florence C, Luo F, Xu L, Zhou C. The economic burden of prescription opioid overdose, abuse and dependence in the United States, 2013. Med Care. 2016;54(10):901.
Kirson NY, Scarpati LM, Enloe CJ, Dincer AP, Birnbaum HG, Mayne TJ. The economic burden of opioid abuse: updated findings. J Manag Care Spec Pharm. 2017;23(4):427–45.
Starr TD, Rogak LJ, Passik SD. Substance abuse in cancer pain. Curr Pain Headache Rep. 2010;14:268–75.
Kwon JH, Tanco K, Park JC, Wong A, Seo L, Liu D, et al. Frequency, predictors, and medical record documentation of chemical coping among advanced cancer patients. Oncologist. 2015;20(6):692–7.
Peterson C, Xu L, Mikosz CA, Florence C, Mack KA. US hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011–2015. J Subst Abuse Treat. 2018;92:35–9.
Singh JA, Cleveland JD. National US time-trends in opioid use disorder hospitalizations and associated health care utilization and mortality. PLoS ONE. 2020;15(2): e0229174.
Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. Elsevier; 2018. p. 1556–68.
Administration DE. National drug threat assessment. US Department of Justice; 2018.
Kim SJ, Medina M, Chang J. Health care utilization of patients with opioid use disorder in US hospitals from 2016 to 2019: focusing on racial and regional variances. Clin Drug Investig. 2022;42(10):853–63.
Knox-Rice T, Xuan L, Wadsworth H, Halm EA, Rhodes RL. Examining the association between health care utilization and clinical characteristics among cancer patients in a safety net health system. J Palliat Med. 2019;22(1):80–3.
Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: a systematic review and meta-analysis. PLoS ONE. 2017;12(12): e0189900.
Miron O, Barda N, Balicer R, Kor A, Lev-Ran S. Association of opioid use disorder with health care utilization and cost in a public health system. Addiction. 2022;117(11):2880–6.
Van Draanen J, Tsang C, Mitra S, Karamouzian M, Richardson L. Socioeconomic marginalization and opioid-related overdose: a systematic review. Drug Alcohol Depend. 2020;214: 108127.
Lee D-C, Liang H, Shi L. The convergence of racial and income disparities in health insurance coverage in the United States. Int J Equity Health. 2021;20(1):1–8.
Qudah B, Maurer MA, Mott DA, Chui MA. Discordance in addressing opioid crisis in rural communities: patient and provider perspectives. Pharmacy. 2022;10(4):91.
Saloner B, McGinty EE, Beletsky L, Bluthenthal R, Beyrer C, Botticelli M, et al. A public health strategy for the opioid crisis. Public Health Rep. 2018;133(1_suppl):24S-34S.
Williams AR, Nunes EV, Bisaga A, Pincus HA, Johnson KA, Campbell AN, et al. Developing an opioid use disorder treatment cascade: a review of quality measures. J Subst Abuse Treat. 2018;91:57–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This paper was supported by Soonchunhyang University Research Fund, BK21 FOUR(Fostering Outstanding Universities for Research, No.:5199990914048, Korean Ministry of Education. The funding sources did not have interventions such as study design and data interpretation.
Conflicts of Interest/Competing Interests
The authors declare that they have no competing interests.
Informed Consent Statement
All participants realized enough for the study's purpose and signed written informed consent before participation.
Consent for Publication
Not applicable
Availability of Data and Material (data transparency)
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code Availability (software application or custom code)
Not applicable.
Authors' Contributions
JHP and JWC led the design and conception of the study, performed the data analysis, and wrote/reviewed the manuscript. SJK and LG contributed by writing the first draft of the manuscript. SJK and AR was reviewing and editing it. All authors read and approved the final manuscript.
Ethics Approval
The data we use are secondary data and all of the patient’s personal data are encrypted and unable to identify. This study was approved for waiver from the Institutional Review Board, Soonchunhyang University (202203-SB-027).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, JH., Kim, S.J., Grajeda, L. et al. Does Opioid Use Disorder Matter for Health Care Utilization Among Lung Cancer Patients? Evidence from U.S. Hospitals During 2016–2020. Clin Drug Investig 43, 635–642 (2023). https://doi.org/10.1007/s40261-023-01297-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01297-0