Abstract
Background
Sodium–glucose cotransporter-2 (SGLT2) inhibitors have been recently used as therapeutic agents for type 2 diabetes mellitus. Recent clinical trials have shown that they are beneficial for reducing the risk of cardiovascular mortality and hospitalization in patients with heart failure (HF). A comprehensive review regarding the cost-effectiveness of different SGLT2 inhibitors for HF treatment may be necessary to help clinicians and decision-makers select the most cost-effective HF treatment option.
Objective
This study conducted a systematic review of economic evaluation studies of SGLT2 inhibitors for the treatment of patients with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF).
Method
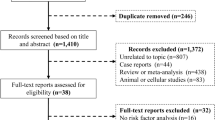
We searched PubMed, Cochrane, Embase, and EBSCOhost to identify published economic evaluation studies on SGLT2 inhibitors for HF treatment until May 2023. Studies on the economic evaluation of SGLT2 inhibitors in the treatment of HF were included. We extracted information such as country, population, intervention, type of model, health status, and conclusion of cost-effectiveness.
Result
Of the 410 studies, 27 were finally selected. All economic evaluation studies used the Markov model, and commonly included health status as stable HF, hospitalization due to HF, and death. All dapagliflozin studies focused on patients with HFrEF (n = 13), and dapagliflozin was cost-effective in 14 countries, but not in the Philippines. All empagliflozin studies focused on the patients with HFrEF also showed the cost-effectiveness of empagliflozin (n = 11). However, empagliflozin use in patients with HFpEF was determined to be cost-effective in studies in Finland, China, and Australia studies but not in studies in Thailand and the USA.
Conclusions
Most of the studies reported the cost-effectiveness of dapagliflozin and empagliflozin in patients with HFrEF. However, the cost-effectiveness of empagliflozin differed from country to country regarding patients with HFpEF. We suggest that further economic evaluation of SGLT2 inhibitors should focus on patients with HFpEF in more countries.

Similar content being viewed by others
References
Chen Z, Li G. Sodium–glucose co-transporter 2 inhibitors compared with sulfonylureas in patients with type 2 diabetes inadequately controlled on metformin: a meta-analysis of randomized controlled trials. Clin Drug Investig. 2019;39(6):521–31.
American Diabetes Association Professional Practice C. Addendum. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2022. Diabetes Care 2022;45(Suppl. 1):S144–S174. Diabetes Care. 2022;45(9):2178–81.
American DA. Introduction: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S1–2.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Correale M, Mazzeo P, Tricarico L, Croella F, Fortunato M, Magnesa M, et al. Pharmacological anti-remodelling effects of disease-modifying drugs in heart failure with reduced ejection fraction. Clin Drug Investig. 2022;42(7):567–79.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Solomon SD, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, et al. Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial. Eur J Heart Fail. 2021;23(7):1217–25.
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383(15):1413–24.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Curtis JP, Sokol SI, Wang Y, Rathore SS, Ko DT, Jadbabaie F, et al. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J Am Coll Cardiol. 2003;42(4):736–42.
Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021;384(2):117–28.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Elserafy AS, Reda A, Farag E, Mostafa T, Farag N, Elbahry A, et al. Egyptian atherosclerosis and vascular biology association consensus on the use of sodium glucose cotransporter-2 inhibitors in heart failure with reduced ejection fraction. Clin Drug Investig. 2021;41(12):1027–36.
Association AH. 2022 AHA/ACC/HFSA guideline for the management of heart failure. J Card Fail. 2022;28(5):e1–167.
Tsutsui H, Ide T, Ito H, Kihara Y, Kinugawa K, Kinugawa S, et al. JCS/JHFS 2021 guideline focused update on diagnosis and treatment of acute and chronic heart failure. Circ J. 2021;85(12):2252–91.
failure TKsoh. KSHF 2022 guideline for the management of heart failure. 2022 ed. Seoul: The Korean Society of Heart Failure; 2022.
Piette JD, Heisler M, Krein S, Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165(15):1749–55.
Heisler M, Wagner TH, Piette JD. Clinician identification of chronically ill patients who have problems paying for prescription medications. Am J Med. 2004;116(11):753–8.
Piette JD, Heisler M, Horne R, Caleb AG. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med. 2006;62(4):846–57.
Wahlster P, Scahill S, Lu CY, Babar Z-U-D. Barriers to access and use of high cost medicines: a review. Health Policy Technol. 2015;4(3):191–214.
Taylor C, Jan S. Economic evaluation of medicines. Aust Prescr. 2017;40(2):76–8.
Hoyle M. Future drug prices and cost-effectiveness analyses. Pharmacoeconomics. 2008;26(7):589–602.
Platz E, Jhund PS, Claggett BL, Pfeffer MA, Swedberg K, Granger CB, et al. Prevalence and prognostic importance of precipitating factors leading to heart failure hospitalization: recurrent hospitalizations and mortality. Eur J Heart Fail. 2018;20(2):295–303.
Yoshida Y, Cheng X, Shao H, Fonseca VA, Shi L. A systematic review of cost-effectiveness of sodium–glucose cotransporter inhibitors for type 2 diabetes. Curr Diabetes Rep. 2020;20(4):12.
Hong D, Si L, Jiang M, Shao H, Ming WK, Zhao Y, et al. Cost effectiveness of sodium–glucose cotransporter-2 (SGLT2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and dipeptidyl peptidase-4 (DPP-4) inhibitors: a systematic review. Pharmacoeconomics. 2019;37(6):777–818.
Wu M, Qin S, Wang L, Tan C, Peng Y, Zeng X, et al. Economic evaluation of dapagliflozin in the treatment of patients with heart failure: a systematic review. Front Pharmacol. 2022;13: 860109.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372): n71.
Ofman JJ, Sullivan SD, Neumann PJ, Chiou CF, Henning JM, Wade SW, et al. Examining the value and quality of health economic analyses: implications of utilizing the QHES. J Manag Care Pharm. 2003;9(1):53–61.
Jiang Y, Zheng R, Sang H. Cost-effectiveness of adding SGLT2 inhibitors to standard treatment for heart failure with reduced ejection fraction patients in China. Front Pharmacol. 2021;12:733681.
Nguyen BN, Mital S, Bugden S, Nguyen HV. Cost-effectiveness of dapagliflozin and empagliflozin for treatment of heart failure with reduced ejection fraction. Int J Cardiol. 2023;1(376):83–9.
Cohen LP, Isaza N, Hernandez I, Lewis GD, Ho JE, Fonarow GC, et al. Cost-effectiveness of sodium-glucose cotransporter-2 inhibitors for the treatment of heart failure with preserved ejection fraction. JAMA Cardiol. 20231;8(5):419–28.
Abdelhamid M, Elsisi GH, Seyam A, Shafie A, Kirollos M, Emad S, et al. Dapagliflozin cost-effectiveness analysis in heart failure patients in Egypt. J Med Econ. 2022;25(1):450–6.
Gil-Rojas Y, Lasalvia P, García Á. Cost-utility of dapagliflozin plus standard treatment compared to standard treatment for the management of heart failure with reduced ejection fraction in Colombia. Expert Rev Pharmacoecon Outcomes Res. 2022;22(4):655–63.
Isaza N, Calvachi P, Raber I, Liu CL, Bellows BK, Hernandez I, et al. Cost-effectiveness of dapagliflozin for the treatment of heart failure with reduced ejection fraction. JAMA Netw Open. 2021;4(7): e2114501.
Krittayaphong R, Permsuwan U. Cost-utility analysis of add-on dapagliflozin treatment in heart failure with reduced ejection fraction. Int J Cardiol. 2021;322:183–90.
Liao CT, Yang CT, Toh HS, Chang WT, Chang HY, Kuo FH, et al. Cost-effectiveness evaluation of add-on dapagliflozin for heart failure with reduced ejection fraction from perspective of healthcare systems in Asia-Pacific region. Cardiovasc Diabetol. 2021;20(1):204.
McEwan P, Darlington O, McMurray JJV, Jhund PS, Docherty KF, Böhm M, et al. Cost-effectiveness of dapagliflozin as a treatment for heart failure with reduced ejection fraction: a multinational health-economic analysis of DAPA-HF. Eur J. 2020;22(11):2147–56.
Mendoza VL, Tumanan-Mendoza BA, Punzalan FER. Cost-utility analysis of add-on dapagliflozin in heart failure with reduced ejection fraction in the Philippines. ESC. 2021;8(6):5132–41.
Miller RJH, Chew DS, Qin L, Fine NM, Chen J, McMurray JJV, et al. Cost-effectiveness of immediate initiation of dapagliflozin in patients with a history of heart failure. Eur J Heart Fail. 2023;25(2):238–47.
Parizo JT, Goldhaber-Fiebert JD, Salomon JA, Khush KK, Spertus JA, Heidenreich PA, et al. Cost-effectiveness of dapagliflozin for treatment of patients with heart failure with reduced ejection fraction. JAMA Cardiol. 2021;6(8):926–35.
Savira F, Wang BH, Kompa AR, Ademi Z, Owen AJ, Zoungas S, et al. Cost-effectiveness of dapagliflozin in chronic heart failure: an analysis from the Australian healthcare perspective. Eur J Prev Cardiol. 2021;28(9):975–82.
Yao Y, Zhang R, An T, Zhao X, Zhang J. Cost-effectiveness of adding dapagliflozin to standard treatment for heart failure with reduced ejection fraction patients in China. ESC. 2020;7(6):3582–92.
Hallinen T, Kivela S, Soini E, Harjola VP, Pesonen M. Cost-effectiveness of empagliflozin in combination with standard care versus standard care only in the treatment of heart failure patients in Finland. ClinicoEcono Outcomes Res. 2023;15:1–13.
Jiang Y, Xie J. Cost-effectiveness of adding empagliflozin to the standard therapy for heart failure with preserved ejection fraction from the perspective of healthcare systems in China. Front Cardiovasc Med. 2022;9:946399.
Krittayaphong R, Permsuwan U. Cost-utility analysis of combination empagliflozin and standard treatment versus standard treatment alone in thai heart failure patients with reduced or preserved ejection fraction. Am J Cardiovasc Drugs. 2022;22(5):577–90.
Liao CT, Yang CT, Kuo FH, Lee MC, Chang WT, Tang HJ, et al. Cost-effectiveness evaluation of add-on empagliflozin in patients with heart failure and a reduced ejection fraction from the healthcare system’s perspective in the Asia-Pacific Region. Front Cardiovasc Med. 2021;8: 750381.
Lin X, Lin M, Liu M, Huang W, Nie X, Chen Z, et al. Cost-effectiveness of empagliflozin as a treatment for heart failure with reduced ejection fraction: an analysis from the Chinese healthcare perspective. J Thorac Dis. 2022;14(5):1588–97.
Lou Y, Hu T, Huang J. Cost-effectiveness of adding empagliflozin to standard treatment for heart failure with preserved ejection fraction patients in China. Am J Cardiovasc Drugs. 2023;23(1):47–57.
Sang H, Wan Y, Ma Z, Zhang S, Zhao Q. Cost-effectiveness of empagliflozin for the treatment of heart failure with reduced ejection fraction in China. Front Cardiovasc Med. 2022;9:1022020.
Tafazzoli A, Reifsnider OS, Bellanca L, Ishak J, Carrasco M, Rakonczai P, et al. A European multinational cost-effectiveness analysis of empagliflozin in heart failure with reduced ejection fraction. Eur J Health Econ. 2022 Dec 4.
Tang Y, Sang H. Cost-utility analysis of empagliflozin in heart failure patients with reduced and preserved ejection fraction in China. Front Pharmacol. 2022;13:1030642.
Tsutsui H, Sakamaki H, Momomura SI, Sakata Y, Kotobuki Y, Linden S, et al. Cost-effectiveness analysis of empagliflozin in patients with heart failure with reduced ejection fraction in Japan based on the EMPEROR-reduced trial. J Cardiol. 2023;81(6):522–30.
Varghese L, Lin W, Linden S, Lum AL, Sim D. Cost-effectiveness of empagliflozin on top of standard of care for heart failure with reduced ejection fraction in Singapore. Value Health Reg Issues. 2023;34:108–17.
Zheng J, Parizo JT, Spertus JA, Heidenreich PA, Sandhu AT. Cost-effectiveness of empagliflozin in patients with heart failure with preserved ejection fraction. JAMA Intern Med. 2022;182(12):1278–88.
Zhou J, Liew D, Kaye DM, Zoungas S, Stub D. Cost-effectiveness of empagliflozin in patients with heart failure and preserved ejection fraction. Circ Cardiovasc Qual Outcomes. 2022;15(10): e008638.
Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337(8746):867–72.
Reifsnider OS, Kansal AR, Gandhi PK, Cragin L, Brand SB, Pfarr E, et al. Cost-effectiveness of empagliflozin versus canagliflozin, dapagliflozin, or standard of care in patients with type 2 diabetes and established cardiovascular disease. BMJ Open Diabetes Res Care. 2021;9(1).
Coles AH, Fisher K, Darling C, Yarzebski J, McManus DD, Gore JM, et al. Long-term survival for patients with acute decompensated heart failure according to ejection fraction findings. Am J Cardiol. 2014;114(6):862–8.
Liu XQ, He LS, Huang JQ, Xiong LJ, Xia C, Lao HY. Cost-effectiveness analyses of sacubitril-valsartan for heart failure. Heart Fail Rev. 2021;26(5):1119–30.
Arbel R, Aboalhasan E, Hammerman A, Azuri J. Dapagliflozin vs. sacubitril-valsartan for prevention of heart failure events in non-diabetic patients with reduced ejection fraction: a cost per outcome analysis. Eur J Prev Cardiol. 2021;28(15):1665–9.
Hammerman A, Azuri J, Aboalhasan E, Arbel R. Dapagliflozin versus sacubitril-valsartan to improve outcomes of patients with reduced ejection fraction and diabetes mellitus. Am J Cardiovasc Drugs. 2022;22(3):325–31.
Xie F, Zhou T. Industry sponsorship bias in cost effectiveness analysis: registry based analysis. BMJ. 2022;22(377): e069573.
Acknowledgements
We would like to thank Editage (http://www.editage.co.kr) for English-language editing and reviewing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the Research Fund, 2020 of The Catholic University of Korea. However, the sponsor had no role in the study design; collection, analysis, and interpretation of the data; in the writing of the report; or in the decision to submit the paper for publication.
Conflict of interest
All authors have no conflict of interest to declare.
Ethics approval, consent to participate and consent for publication
Not applicable.
Availability of data and material
All articles included in the study can be found and accessed in their respective journals according to their bibliographic information.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nam, K., Cho, D.SH., Kim, H. et al. Systematic Review of the Economic Evaluation of Sodium–Glucose Cotransporter-2 Inhibitors Used as Treatment in Patients with Heart Failure. Clin Drug Investig 43, 463–474 (2023). https://doi.org/10.1007/s40261-023-01283-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01283-6