Abstract
Background and Objective
Evidence of the effectiveness of statins compared with fibrates for primary prevention of cardiovascular events is limited. Therefore, we assessed the comparative effectiveness of simvastatin versus gemfibrozil for primary prevention of major adverse cardiovascular events (MACE) and mortality.
Methods
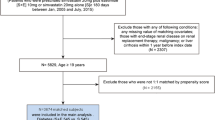
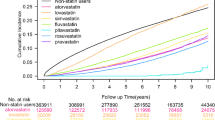
This territory-wide cohort study used electronic health records of simvastatin and gemfibrozil prescriptions from the Hong Kong Hospital Authority and compared simvastatin or gemfibrozil initiation. The primary outcome was MACE, defined as the composite of the first diagnosis of cardiovascular mortality, coronary heart disease, or stroke. Secondary outcomes were the individual components of MACE, all-cause mortality, and non-cardiovascular mortality. Inverse probability of treatment weighting on the propensity score was used to estimate hazard ratios (HRs).
Results
A total of 223,699 individuals (120,207 [53.7%] women; median follow-up 7.0 years [interquartile range 5.7–9.1]) who were prescribed simvastatin (n = 168,630) or gemfibrozil (n = 55,069) were included. Simvastatin was associated with a reduced risk of MACE (HR 0.90, 95% confidence interval [CI] 0.88–0.93), all-cause mortality (HR 0.88, 95% CI 0.86–0.90), cardiovascular mortality (HR 0.71, 95% CI 0.67–0.76), and non-cardiovascular mortality (HR 0.92, 95% CI 0.89–0.95). Associations for MACE varied according to baseline characteristics with gemfibrozil being associated with a reduced risk of MACE in men and patients with low baseline high-density lipoprotein (HDL) cholesterol (< 1.0 mmol/L).
Conclusion
The results of this study showed better population-level effectiveness of simvastatin compared with gemfibrozil for the primary prevention of MACE; however, a definitive randomized controlled trial is required to compare simvastatin with gemfibrozil among patients with low HDL cholesterol, as they appear to obtain benefit with gemfibrozil.



Similar content being viewed by others
References
Blais JE, Wei Y, Yap KK, Alwafi H, Ma TT, Brauer R, et al. Trends in lipid-modifying agent use in 83 countries. Atherosclerosis. 2021;328:44–51. https://doi.org/10.1016/j.atherosclerosis.2021.05.016.
Blais JE, Tong GKY, Pathadka S, Mok M, Wong ICK, Chan EW. Comparative efficacy and safety of statin and fibrate monotherapy: a systematic review and meta-analysis of head-to-head randomized controlled trials. PLoS One. 2021;16(2): e0246480. https://doi.org/10.1371/journal.pone.0246480.
Fisman EZ, Adler Y, Tenenbaum A. Statins research unfinished saga: desirability versus feasibility. Cardiovasc Diabetol. 2005;4(1):8. https://doi.org/10.1186/1475-2840-4-8.
Manninen KV, Tenkanen PL, Koskinen HP, Huttunen HJ, Mänttäri HM, Heinonen HO, et al. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study: implications for treatment. Circulation. 1992;85(1):37–45. https://doi.org/10.1161/01.CIR.85.1.37.
Goldfine AB, Kaul S, Hiatt WR. Fibrates in the treatment of dyslipidemias—time for a reassessment. N Engl J Med. 2011;365(6):481–4. https://doi.org/10.1056/NEJMp1106688.
Bruckert E, Labreuche J, Deplanque D, Touboul P-J, Amarenco P. Fibrates effect on cardiovascular risk is greater in patients with high triglyceride levels or atherogenic dyslipidemia profile: a systematic review and meta-analysis. J Cardiovasc Pharmacol. 2011;57(2):267–72. https://doi.org/10.1097/FJC.0b013e318202709f.
Lee M, Saver JL, Towfighi A, Chow J, Ovbiagele B. Efficacy of fibrates for cardiovascular risk reduction in persons with atherogenic dyslipidemia: a meta-analysis. Atherosclerosis. 2011;217(2):492–8. https://doi.org/10.1016/j.atherosclerosis.2011.04.020.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010.
Adams C, Singh K. Geographic variation in the statin trials: underrepresentation of Asian populations. Int J Cardiol. 2020;316:249–51. https://doi.org/10.1016/j.ijcard.2020.07.015.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. N Engl J Med. 1987;317(20):1237. https://doi.org/10.1056/NEJM198711123172001.
Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. N Engl J Med. 1999;341(6):410. https://doi.org/10.1056/NEJM199908053410604.
Ginsberg HN, Elam MB, Lovato LC, Crouse JR III, Leiter LA, Linz P, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1563–74. https://doi.org/10.1056/NEJMoa1001282.
Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, et al. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010;375(9729):1875–84. https://doi.org/10.1016/S0140-6736(10)60656-3.
Vogel B, Acevedo M, Appelman Y, Bairey Merz CN, Chieffo A, Figtree GA, et al. The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet. 2021;397(10292):2385–438. https://doi.org/10.1016/S0140-6736(21)00684-X.
Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316(12):1289–97. https://doi.org/10.1001/jama.2016.13985.
Marston NA, Giugliano RP, Im K, Silverman MG, O’Donoghue ML, Wiviott SD, et al. Association between triglyceride lowering and reduction of cardiovascular risk across multiple lipid-lowering therapeutic classes. Circulation. 2019;140(16):1308–17. https://doi.org/10.1161/CIRCULATIONAHA.119.041998.
Ference BA, Kastelein JJP, Ray KK, Ginsberg HN, Chapman MJ, Packard CJ, et al. Association of triglyceride-lowering LPL variants and LDL-C-lowering LDLR variants with risk of coronary heart disease. JAMA. 2019;321(4):364–73. https://doi.org/10.1001/jama.2018.20045.
Richardson TG, Sanderson E, Palmer TM, Ala-Korpela M, Ference BA, Davey Smith G, et al. Evaluating the relationship between circulating lipoprotein lipids and apolipoproteins with risk of coronary heart disease: a multivariable Mendelian randomisation analysis. PLoS Med. 2020;17(3): e1003062. https://doi.org/10.1371/journal.pmed.1003062.
Sniderman AD, Thanassoulis G, Glavinovic T, Navar AM, Pencina M, Catapano A, et al. Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol. 2019;4(12):1287–95. https://doi.org/10.1001/jamacardio.2019.3780.
Sniderman AD, Couture P, Martin SS, DeGraaf J, Lawler PR, Cromwell WC, et al. Hypertriglyceridemia and cardiovascular risk: a cautionary note about metabolic confounding. J Lipid Res. 2018;59(7):1266–75. https://doi.org/10.1194/jlr.R082271.
Fleurence R, Naci H, Jansen JP. The critical role of observational evidence in comparative effectiveness research. Health Aff. 2010;29(10):1826–33. https://doi.org/10.1377/hlthaff.2010.0630.
Kung K, Lam A, Li P. A retrospective analysis on the use of gemfibrozil in general outpatient clinics. Hong Kong Practitioner. 2005;27(11):404.
Wong AY, Root A, Douglas IJ, Chui CS, Chan EW, Ghebremichael-Weldeselassie Y, et al. Cardiovascular outcomes associated with use of clarithromycin: population based study. BMJ. 2016;352: h6926. https://doi.org/10.1136/bmj.h6926.
Lund JL, Richardson DB, Stürmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep. 2015;2(4):221–8. https://doi.org/10.1007/s40471-015-0053-5.
White IR, Royston P. Imputing missing covariate values for the Cox model. Stat Med. 2009;28(15):1982–98. https://doi.org/10.1002/sim.3618.
van Buuren S, Groothuis-Oudshoorn CGM. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67. https://doi.org/10.18637/jss.v045.i03.
Burgette LF, Reiter JP. Multiple imputation for missing data via sequential regression trees. Am J Epidemiol. 2010;172(9):1070–6. https://doi.org/10.1093/aje/kwq260.
Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–64. https://doi.org/10.1093/aje/kwn164.
Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Gu X, Yang X, Li Y, Cao J, Li J, Liu X, et al. Usefulness of low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol as predictors of cardiovascular disease in Chinese. Am J Cardiol. 2015;116(7):1063–70. https://doi.org/10.1016/j.amjcard.2015.06.040.
Leyrat C, Seaman SR, White IR, Douglas I, Smeeth L, Kim J, et al. Propensity score analysis with partially observed covariates: how should multiple imputation be used? Stat Methods Med Res. 2019;28(1):3–19. https://doi.org/10.1177/0962280217713032.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987.
Roussel R, Chaignot C, Weill A, Travert F, Hansel B, Marre M, et al. Use of fibrates monotherapy in people with diabetes and high cardiovascular risk in primary care: a French nationwide cohort study based on national administrative databases. PLoS One. 2015;10(9): e0137733. https://doi.org/10.1371/journal.pone.0137733.
Rubins HB, Robins SJ, Collins D, Nelson DB, Elam MB, Schaefer EJ, et al. Diabetes, plasma insulin, and cardiovascular disease: subgroup analysis from the Department of Veterans Affairs High-Density Lipoprotein Intervention Trial (VA-HIT). Arch Intern Med. 2002;162(22):2597–604. https://doi.org/10.1001/archinte.162.22.2597.
Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2021–31. https://doi.org/10.1056/NEJMoa1600176.
Acknowledgements
The computations were performed using research computing facilities offered by Information Technology Services, the University of Hong Kong. Joseph E. Blais was supported by the Hong Kong Research Grants Council as a recipient of the Hong Kong PhD Fellowship Scheme. The authors thank Dr Stephen Weng for his feedback on an earlier draft of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded.
Conflict of interest
Joseph E. Blais, Xuxiao Ye, Eric Y.F. Wan, William C.W. Wong, Ian C.K. Wong, Brian Tomlinson, and Esther W. Chan have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (reference number: UW17-135).
Consent to participate
This is an observational study and informed consent was waived by the Institutional Review Board.
Consent for publication
Not applicable.
Data availability
The data used for this study are confidential and are not available for sharing.
Code availability
Not applicable.
Author contributions
JEB and XY had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Conceptualization: JEB, EWC, BT. Formal analysis: JEB, XY. Validation: XY. Resources: EWC, ICKW. Software: EYFW. Visualization: JEB. Supervision: EWC, ICKW. Writing—original draft: JEB. Writing—review and editing of the manuscript for important intellectual content: All authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Blais, J.E., Ye, X., Wan, E.Y.F. et al. Effectiveness of Simvastatin Versus Gemfibrozil for Primary Prevention of Cardiovascular Events: A Retrospective Cohort Study of 223,699 Primary Care Patients. Clin Drug Investig 42, 987–997 (2022). https://doi.org/10.1007/s40261-022-01208-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01208-9