Abstract
Background
Alcohol dependence remains a major health problem from both a public health and clinical perspective. Harm reduction strategies have been increasingly recognized as suitable treatment goals. Nalmefene has been recently approved for this precise therapeutic indication after completion of phase III trials. However, more data from routine practice settings are needed in order to obtain evidence with high external validity. The aim of this study was to conduct a single-arm, phase IV study with alcohol-dependent outpatients starting nalmefene for the first time.
Methods
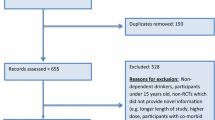
An observational, multisite, single-arm, phase IV study was conducted among adult alcohol-dependent outpatients who received nalmefene for the first time. The study consisted of four visits: baseline, 4 weeks (referred to as 1 month hereafter), 6 and 12 months. At each visit, drinking variables were obtained from the Timeline Followback regarding the previous month. Satisfaction with medication was also assessed for both patients and professionals, with the Medication Satisfaction Questionnaire. A repeated measures mixed model was performed for effectiveness analysis regarding drinking outcomes (reduction in total alcohol consumption and number of heavy drinking days). Regression analyses were performed in order to find predictors of response to nalmefene.
Results
A total of 110 patients were included, with 88 reporting data at the 1-month visit. On average, patients took nalmefene 68% of the days. The number of heavy drinking days decreased from 13.5 to 6.8 days/month, and total alcohol consumption decreased from 169 to 79 units. For both outcomes, significant reductions at 1 month were found, with no other significant variables reaching significance. Thirty-seven patients were considered medication responders, but given the high presence of low-risk drinkers in our sample, no significant predictors could be found. Satisfaction was globally high for both professionals and patients, and overall nalmefene was well tolerated, with no serious adverse events reported.
Conclusion
The data provided by this phase IV study suggest nalmefene is an effective, well-tolerated treatment for alcohol dependence in real-world, clinical settings.


Similar content being viewed by others
References
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–79.
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–66.
Merkx MJM, Schippers GM, Koeter MWJ, Vuijk PJ, Oudejans SCC, Stam RK, et al. Guidelines for allocating outpatient alcohol abusers to levels of care: predictive validity. Addict Behav. 2011;36(6):570–5.
Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62(2):211–20.
Agency EM. Guideline on the development of medicinal products for the treatment of alcohol dependence. European Medicines Agency 2010. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/03/WC500074898.pdf. Accessed 1 Sept 2017.
Gastfriend DR, Garbutt JC, Pettinati HM, Forman RF. Reduction in heavy drinking as a treatment outcome in alcohol dependence. J Subst Abuse Treat. 2007;33(1):71–80.
Heilig M, Goldman D, Berrettini W, O’Brien CP. Pharmacogenetic approaches to the treatment of alcohol addiction. Nat Rev Neurosci. 2011;12(11):670–84.
Luquiens A, Reynaud M, Aubin HJ. Is controlled drinking an acceptable goal in the treatment of alcohol dependence? A survey of French alcohol specialists. Alcohol Alcohol. 2011;46(5):586–91.
Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Res Health. 2011;34(2):135–43.
Dixon R, Gentile J, Hsu HB, Hsiao J, Howes J, Garg D, et al. Nalmefene: safety and kinetics after single and multiple oral doses of a new opioid antagonist. J Clin Pharmacol. 1987;27(3):233–9.
Gal TJ, DiFazio CA, Dixon R. Prolonged blockade of opioid effect with oral nalmefene. Clin Pharmacol Ther. 1986;40(5):537–42.
Emmerson PJ, Liu MR, Woods JH, Medzihradsky F. Binding affinity and selectivity of opioids at mu, delta and kappa receptors in monkey brain membranes. J Pharmacol Exp Ther. 1994;271(3):1630–7.
Ingman K, Hagelberg N, Aalto S, Någren K, Juhakoski A, Karhuvaara S, et al. Prolonged central mu-opioid receptor occupancy after single and repeated nalmefene dosing. Neuropsychopharmacology. 2005;30(12):2245–53.
Bruijnzeel AW. kappa-Opioid receptor signaling and brain reward function. Brain Res Rev. 2009;62(1):127–46.
Garbutt JC. Efficacy and tolerability of naltrexone in the management of alcohol dependence. Curr Pharm Des. 2010;16(19):2091–7.
Swift RM. Naltrexone and nalmefene: any meaningful difference? Biol Psychiatry. 2013;73(8):700–1.
Mason BJ, Salvato FR, Williams LD, Ritvo EC, Cutler RB. A double-blind, placebo-controlled study of oral nalmefene for alcohol dependence. Arch Gen Psychiatry. 1999;56(8):719–24.
Mason BJ, Ritvo EC, Morgan RO, Salvato FR, Goldberg G, Welch B, et al. A double-blind, placebo-controlled pilot study to evaluate the efficacy and safety of oral nalmefene HCl for alcohol dependence. Alcohol Clin Exp Res. 1994;18(5):1162–7.
Anton RF, Pettinati H, Zweben A, Kranzler HR, Johnson B, Bohn MJ, et al. A multi-site dose ranging study of nalmefene in the treatment of alcohol dependence. J Clin Psychopharmacol. 2004;24(4):421–8.
Karhuvaara S, Simojoki K, Virta A, Rosberg M, Loyttyniemi E, Nurminen T, et al. Targeted nalmefene with simple medical management in the treatment of heavy drinkers: a randomized double-blind placebo-controlled multicenter study. Alcohol Clin Exp Res. 2007;31(7):1179–87.
Gual A, He Y, Torup L, van den Brink W, Mann K. A randomised, double-blind, placebo-controlled, efficacy study of nalmefene, as-needed use, in patients with alcohol dependence. Eur Neuropsychopharmacol. 2013;23(11):1432–42.
Mann K, Bladström A, Torup L, Gual A, van den Brink W. Extending the treatment options in alcohol dependence: a randomized controlled study of as-needed nalmefene. Biol Psychiatry. 2013;73(8):706–13.
van den Brink W, Aubin HJ, Bladstrom A, Torup L, Gual A, Mann K. Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies. Alcohol Alcohol. 2013;48(5):570–8.
van den Brink W, Sørensen P, Torup L, Mann K, Gual A, SENSE Study Group. Long-term efficacy, tolerability and safety of nalmefene as-needed in patients with alcohol dependence: a 1-year, randomised controlled study. J Psychopharmacol. 2014;28(8):733–44.
Pearson M, Coomber R. The challenge of external validity in policy-relevant systematic reviews: a case study from the field of substance misuse. Addiction. 2010;105(1):136–45.
Dekkers OM, von Elm E, Algra A, Romijn JA, Vandenbroucke JP. How to assess the external validity of therapeutic trials: a conceptual approach. Int J Epidemiol. 2010;39(1):89–94.
Rothwell PM. External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet. 2005;365(9453):82–93.
Hoertel N, de Maricourt P, Katz J, Doukhan R, Lavaud P, Peyre H, et al. Are participants in pharmacological and psychotherapy treatment trials for social anxiety disorder representative of patients in real-life settings? J Clin Psychopharmacol. 2014;34(6):697–703.
Uijen AA, Bakx JC, Mokkink HGA, van Weel C. Hypertension patients participating in trials differ in many aspects from patients treated in general practices. J Clin Epidemiol. 2007;60(4):330–5.
Persaud N, Mamdani MM. External validity: the neglected dimension in evidence ranking. J Eval Clin Pract. 2006;12(4):450–3.
Farahani P, Levine M, Gaebel K, Thabane L. Clinical data gap between phase III clinical trials [pre-marketing] and phase IV [post-marketing] studies: evaluation of etanercept in rheumatoid arthritis. Can J Clin Pharmacol. 2005;12(3):e254–63.
Linden M. Phase-IV research: specifics, objectives and methodology. Pharmacopsychiatry. 1984;17(5):140–2.
Naudet F, Granger B, Braillon A. Cost-effectiveness of nalmefene: exaggerated expectations or fallacy? Alcohol Alcohol. 2016;51(5):623–4.
Soyka M, Friede M, Schnitker J. Comparing nalmefene and naltrexone in alcohol dependence: are there any differences? Results from an indirect meta-analysis—comment to Naudet. Pharmacopsychiatry. 2016;49(6):261–2.
Naudet F, Fitzgerald N, Braillon A. Nalmefene for alcohol dependence: a NICE decision? Lancet Psychiatry. 2016;3(12):1104–5.
Fitzgerald N, Angus K, Elders A, de Andrade M, Raistrick D, Heather N, et al. Weak evidence on nalmefene creates dilemmas for clinicians and poses questions for regulators and researchers. Addiction. 2016;111(8):1477–87.
Barrio P, Ortega L, Bona X, Gual A. Development, validation, and implementation of an innovative mobile app for alcohol dependence management: protocol for the SIDEAL trial. JMIR Res Protoc. 2016;5(1):e27.
Barrio P, Ortega L, López H, Gual A. Self-management and shared decision-making in alcohol dependence via a mobile app: a pilot study. Int J Behav Med. 2017;24(5):722–727.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported ethanol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: psychosocial and biological methods. Totowa: Humana Press; 1992. p. 41–72.
Kalali A. Patient satisfaction with, and acceptability of, atypical antipsychotics. Curr Med Res Opin. 1999;15(2):135–7.
Vernon MK, Revicki DA, Awad AG, Dirani R, Panish J, Canuso CM, et al. Psychometric evaluation of the Medication Satisfaction Questionnaire [MSQ] to assess satisfaction with antipsychotic medication among schizophrenia patients. Schizophr Res. 2010;118(1–3):271–8.
Flensborg-Madsen T, Mortensen EL, Knop J, Becker U, Sher L, Grønbæk M. Comorbidity and temporal ordering of alcohol use disorders and other psychiatric disorders: results from a Danish register-based study. Compr Psychiatry. 2009;50(4):307–14.
Fein G. Psychiatric comorbidity in alcohol dependence. Neuropsychol Rev. 2015;25(4):456–75.
Monterosso JR, Flannery BA, Pettinati HM, Oslin DW, Rukstalis M, O’Brien CP, et al. Predicting treatment response to naltrexone: the influence of craving and family history. Am J Addict. 2001;10(3):258–68.
Garbutt JC, Greenblatt AM, West SL, Morgan LC, Kampov-Polevoy A, Jordan HS, et al. Clinical and biological moderators of response to naltrexone in alcohol dependence: a systematic review of the evidence. Addiction. 2014;109(8):1274–84.
Dundon WD, Pettinati HM, Lynch KG, Xie H, Varillo KM, Makadon C, et al. The therapeutic alliance in medical-based interventions impacts outcome in treating alcohol dependence. Drug Alcohol Depend. 2008;95(3):230–6.
Öjehagen A, Berglund M, Hansson L. The relationship between helping alliance and outcome in outpatient treatment of alcoholics: a comparative study of psychiatric treatment and multimodal behavioural therapy. Alcohol Alcohol. 1997;32(3):241–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Lundbeck. The sponsor was involved in the study design, but not in data collection, analysis, manuscript writing, or the decision to submit the article for publication.
Conflict of interest
Dr. Barrio, Dr. Roncero, Dr. Guardia and Dr. Gual have received honoraria from Lundbeck. Dr. Barrio has also received honoraria from Pfizer. Dr. Roncero has also received honoraria from Janssen-Cilag, Otsuka, Server, GSK, Rovi, Astra, MSD and Sanofi. Dr. Yuguero and Dr. Ortega have no conflict of interest to declare.
Ethics approval
The study protocol, final approved informed consent document, and all supporting information were submitted to and approved by the institutional review boards of all participating centers.
Consent to participate
All participants provided written informed consent before taking part in study procedures. The study was conducted in accordance with the International Conference on Harmonisation and Good Clinical Practice and the principles of the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Barrio, P., Ortega, L., Guardia, J. et al. Who Receives Nalmefene and How Does It Work in the Real World? A Single-Arm, Phase IV Study of Nalmefene in Alcohol Dependent Outpatients: Baseline and 1-Month Results. Clin Drug Investig 38, 147–155 (2018). https://doi.org/10.1007/s40261-017-0590-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0590-4