Abstract
Background
Oral and intravenous formulations of ciprofloxacin have established efficacy and safety profiles in respiratory infections. A dry powder for inhalation (DPI) that uses Novartis’ PulmoSphere™ technology has been developed to deliver high concentrations of ciprofloxacin to the lung with low systemic exposure using a portable and convenient passive dry powder inhaler (Novartis’ T-326 inhaler).
Objectives
The primary objective was to investigate the safety and tolerability of ciprofloxacin DPI in healthy male subjects, with a secondary objective to investigate the pharmacokinetics of ciprofloxacin after ciprofloxacin DPI administration.
Methods
This was a phase I, single-dose, single-site, randomized, single-blind, placebo-controlled, crossover study conducted in the hospital setting. Subjects were followed up for safety for approximately 2 weeks. Six healthy male subjects, aged 27–42 years with no history of pulmonary disease, repeated bronchitis or respiratory allergies were enrolled. In randomized order and separated by a 1-week washout period, subjects inhaled a single dose of ciprofloxacin DPI 32.5 mg or placebo from the T-326 inhaler. Primary safety parameters included vital signs, electrocardiogram, laboratory tests, adverse events and lung function (total specific resistance, thoracic gas volume and forced expiratory volume in 1 s). Plasma concentration–time data were used to calculate pharmacokinetic parameters.
Results
Ciprofloxacin DPI was well tolerated with no clinically relevant adverse effects on lung function. Estimates of lung deposition derived from physiology-based pharmacokinetic modelling suggest that approximately 40 % of the total dose of ciprofloxacin DPI reached the trachea/bronchi and alveolar space. Systemic ciprofloxacin was detected soon after inhalation [peak concentration in plasma (C max) 56.42 μg/L, median time to C max 0.625 h], but total systemic exposure was minimal (area under the plasma concentration–time curve 354.4 μg·h/L). Terminal elimination half-life (9.5 h), apparent total clearance from plasma after non-intravenous administration (91.7 L/h) and apparent volume of distribution (1,262 L) data suggest that elimination from the respiratory tract was prolonged.
Conclusions
In healthy subjects, ciprofloxacin DPI was well tolerated, delivered ciprofloxacin to the lungs and resulted in minimal systemic exposure, allowing further investigation of its clinical use for the management of specific, chronic infections in pulmonary diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Pulmonary infections are a frequent and recurrent problem for patients with chronic respiratory conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis (CF) and non-CF bronchiectasis (BE) [1–3]. Chronic infection with Gram-negative bacteria, such as Haemophilus influenzae, Moraxella catarrhalis and Pseudomonas aeruginosa, and the Gram-positive bacterium Streptococcus pneumoniae is common and is associated with an increased rate of progressive deterioration of lung function [1, 3, 4]. The presence of P. aeruginosa is a significant predictor of morbidity in all three diseases [5, 6].
For more than 30 years, inhaled antibacterials have been effective in ameliorating chronic pulmonary infections associated with CF and have contributed to improve patient survival rates greatly [7]. At present, the options for inhaled antibacterial treatment for chronic Pseudomonas infections in patients with CF are nebulized tobramycin, aztreonam or colistin. In a study of patients with CF, intermittent tobramycin delivered by a jet nebulizer was well tolerated, decreased the risk of hospitalization compared with placebo and, after three treatment cycles, improved pulmonary function and decreased the density of P. aeruginosa in sputum relative to baseline [8]. In addition, regular, long-term, nebulized gentamicin has been shown to be of significant benefit in patients with BE [9] and has been proposed as a possible treatment option for exacerbations of COPD [10]; however, at present, no long-term intermittent antibacterial treatments have been approved for non-CF BE and COPD.
Use of a nebulizer, although of great value to patients with chronic infections, requires extended administration time and bulky equipment that must be maintained, cleaned and sterilized for infection control, as well as being expensive and of only limited efficiency [11]. Nebulized tobramycin or colistin for CF is used in repeated cycles of 28 days on drug and 28 days off drug, and loss of at least some of the gains in lung function is frequently observed during the drug-free break [8, 12, 13]. In contrast, intermittent pulsed antibacterial therapy in patients with COPD has been shown to reduce the likelihood of an exacerbation with no evidence of the development of resistance [14]. Alternative treatments are, therefore, being investigated that comprise both different antibacterials and formulations that can be delivered more conveniently.
Ciprofloxacin dry powder for inhalation (DPI) has been developed to combine the convenience of dry powder inhalation with the advantages of an established fluoroquinolone antibacterial with proven bactericidal activity against the most frequent bacterial respiratory pathogens, including H. influenzae, S. pneumoniae, M. catarrhalis and P. aeruginosa [15, 16]. The objective has been to achieve high concentrations of ciprofloxacin in the lung while keeping systemic drug exposure low. It is hypothesized that long-term intermittent therapy with ciprofloxacin DPI could reduce the bacterial load in pulmonary diseases associated with chronic airway infections and contribute to an improved quality of life for these patients.
Ciprofloxacin DPI uses the zwitterionic salt ciprofloxacin betaine, which has a prolonged terminal elimination half-life (t ½) when instilled intratracheally as a micronized suspension compared with ciprofloxacin hydrochloride, the formulation for oral ciprofloxacin (t ½ 13.5 vs <1 h, respectively, in preclinical studies) [17]. The formulation utilizes Novartis’ PulmoSphere™ technology, in which an emulsion-based, spray-drying process creates ultra-low-density sponge-like particles with controlled size, density and morphology, optimized for pulmonary delivery (mass median aerodynamic diameters <5 μm) [18–20].
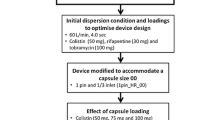
Benchtop studies were conducted to test the efficiency of product delivery to specific patient populations, including an assessment of emitted dose of ciprofloxacin at various flow rates (ranging from 25 to 85 L/min at a constant inhaled volume of 2.0 L) representative of those achievable by the target patient population [21, 22]. For each flow rate, 25 replicates were analysed using five different T-326 inhalers with five capsules per inhaler (Fig. 1). A ciprofloxacin-specific high-performance liquid chromatography (HPLC) assay determined the amount of ciprofloxacin discharged from the T-326 inhaler and the amount retained in the device and capsule. Visual inspection of the capsules was also performed to confirm that a minimal amount of powder remained in the capsules after inhalation. The predefined threshold for emitted dose was met at flow rates as low as 30 L/min after one inhalation and as low as 25 L/min after two inhalations [23]. These inspiratory flow rates can be achieved by both paediatric and adult patients who have significant decreases in lung function [24].
The primary objective of this study was to determine the safety and tolerability of ciprofloxacin DPI given as a single dose to healthy male subjects. The secondary objective was to investigate the pharmacokinetic properties of ciprofloxacin delivered by this route, to determine its appropriateness for use in managing chronic infections in pulmonary conditions.
2 Subjects and Methods
This phase I, randomized, single-blinded, placebo-controlled, two-fold crossover study in healthy male subjects was conducted at the CRS Clinical Research Services Mannheim, Germany (CRS-Mannheim; European clinical trials database reference: 2006-001594-26).
2.1 Study Population
Eligible subjects were aged 18–45 years, with a body mass index of 18–32 kg/m2, and provided written informed consent. Study approval was obtained from the Ethics Committee of the Baden-Württemberg Medical Council, Stuttgart, Germany. The study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation/Good Clinical Practice, the European Union Directive 2001/20/EC and German drug law [Arzneimittelgesetz (AMG)].
Main exclusion criteria included history of relevant organ disease; febrile illness within 1 week prior to study start; history of pulmonary disease, repeated bronchitis or allergic reactions of the bronchial/pulmonary system; history of severe allergies, non-allergic drug reactions or multiple drug allergies; regular daily consumption of xanthine-containing drinks (>1 L) or more than 10 cigarettes; use of medication within 2 weeks of study start that could interfere with the investigational product; and relevant deviation from the normal range in the clinical examination or in clinical chemistry, haematology, urinalysis, electrocardiogram (ECG), blood pressure or heart rate.
2.2 Study Drug
Ciprofloxacin DPI (Bayer Pharma AG, Wuppertal, Germany) was administered using Novartis’ T-326 inhalers. Capsules were filled with ciprofloxacin DPI 32.5 mg (corresponding to 50 mg dry powder); placebo was formulated as a 50-mg dry powder for inhalation in identical capsules (40 mg fill weight).
After randomization, each subject received, under fasting conditions, a single dose of ciprofloxacin DPI and a corresponding dose of placebo (or vice versa) after a washout period of at least 1 week (to allow elimination of study drug and a safety follow-up after the first dose). Inhalation instructions were to inhale deeply and comfortably for each capsule. Immediately after inhalation, subjects drank 240 mL of non-sparkling water at room temperature to wash into the gastrointestinal tract any powder that did not pass through the glottis during inhalation and facilitate its absorption there.
2.3 Assessments
Medical history, physical examination and clinical laboratory tests were performed at screening. Safety assessments (vital signs, ECG and lung function) were performed on the day before study start, on the day of study start prior to inhalation and periodically throughout each 48-h study period. Physical examination, clinical laboratory tests and safety assessments were also performed during the post-study examination. Lung function parameters were measured by whole-body plethysmography. Total specific resistance and thoracic gas volume for an individual at any time point were each taken to be the mean value from at least three acceptable manoeuvres. The value of forced expiratory volumes in 1 s (FEV1), however, was taken to be the maximum of all the individual’s readings at that time point because of the dependence of this parameter upon the cooperation of the subject and the fact that, in healthy subjects, lung function is not affected by any pathophysiological effects. Clinical laboratory parameters (serology, haematology, clinical chemistry, urinalysis, urine drug screen and alcohol breath test) were evaluated at the start of the study and at 48 h post dose. Safety and tolerability were evaluated throughout the study by the incidence of abnormal findings in safety assessments, laboratory parameters and by assessment of treatment-emergent adverse events (AEs), which were summarized using MedDRA version 9.0.
2.4 Pharmacokinetic Analysis
Blood samples were collected pre-dose and at 0.25, 0.5, 0.75, 1.0, 1.5, 2.0, 2.5, 3.0, 4.0, 6.0, 8.0, 12, 16, 24, 36 and 48 h after study drug administration for assessment of ciprofloxacin concentrations. Plasma ciprofloxacin concentrations were determined by HPLC coupled with a tandem mass spectrometer. Grepafloxacin was used as the internal standard and the calibration range of the procedure was 0.500–200 μg/L. Quality control samples in the concentration range of 1.50–150 μg/L were determined, with an accuracy of 96.4–105 % and a precision of 3.52–6.57 % (n = 7).
Urine samples were collected pre-dose and over 0–4, 4–8, 8–12, 12–24 and 24–48 h post dose for measurement of ciprofloxacin concentrations. Concentrations of ciprofloxacin in urine were determined by HPLC coupled with a fluorescence detector. Ofloxacin was used as the internal standard. The calibration range of the procedure was 10.0–1,000 μg/L. Quality control samples in the concentration range 1,000–75,000 μg/L related to non-diluted urine were determined, with an accuracy of 89.3–92.4 % and a precision of 1.02–3.56 % (n = 4–5).
Derived primary pharmacokinetic parameters were area under the plasma concentration–time curve from time zero to infinity (AUC∞), area under the plasma concentration–time curve from time zero to the time of last measurable concentration (AUClast), area under the plasma concentration–time curve from time zero to 24 h (AUC24), maximum plasma concentration (C max), time to reach C max (t max), terminal t ½, cumulative amount of unchanged drug excreted into the urine (Ae) and mean residence time (MRT). Secondary pharmacokinetic parameters were apparent total body clearance of ciprofloxacin from plasma after non-intravenous administration (CL/F), apparent volume of distribution during terminal phase after non-intravenous administration (V z/F), drug concentration in plasma 24 h post dose, AUC divided by dose (AUC/D) and AUC divided by dose per kg body weight (AUCnorm). Pharmacokinetic analysis of plasma drug concentration–time data was performed by model-independent (compartment-free) analysis using WinNonlin® 4.1a software (Pharsight Corporation, Mountain View, CA, USA).
2.5 Physiologically Based Pharmacokinetic Model of Inhaled Administration
A physiologically based pharmacokinetic (PBPK) model of inhaled administration was developed in-house using the PKSim® software (Bayer Technology Services GmbH, Leverkusen, Germany) and was used to estimate total and regional ciprofloxacin DPI deposition [25]. Physiology-based, whole-body PBPK models have been developed and are well suited to assess the influence of individual physiological variability on the pharmacokinetics of drugs [26]. Such a model was therefore chosen to describe the fractions of ciprofloxacin deposited in the oral cavity, trachea and bronchi, and the deep alveolar space.
Mathematically, the model is described by the following equation:
where C(t)inhalation is the modelled time–concentration curve for inhaled drug; f OC is the fraction of the dose that is deposited in the oral cavity and ingested as an oral dose; f TB is the fraction deposited in the trachea and bronchi, where there is a lack of effective systemic absorption and mucociliary clearance removes the drug to the oral cavity so that it is in effect a delayed oral dose; t is time; T MC is the half-life of mucociliary clearance modelled as a first-order process; f ALV is the fraction of the dose that is deposited in the deep alveolar space of the lung, which is modelled as an intravenous (iv) bolus on the assumption of rapid dissolution and absorption; and C(t)oral and C(t)iv are the previously validated simulated concentration–time profiles of ciprofloxacin after oral and iv administration, respectively, normalized to dose (1 mg). DOSE was set to the dose used in the clinical study (32.5 mg). The term \( \exp \left( { - \ln (2)\frac{t}{{T_{\text{MC}} }}} \right) \otimes C(t)_{\text{oral}} \) denotes the convolution (⊗) of the mucociliary clearance process with the oral absorption profile.
The equation was used to individually fit PBPK simulation to the observed plasma concentration–time course of ciprofloxacin for each subject after inhalation of ciprofloxacin DPI (corrected for body weight in the iv-based and oral-based simulations). The fit parameters were the three deposition fractions (f OC, f TB, f ALV) and T MC. The resulting fit factors were calculated per individual, both for each region separately and for the sum of the three fractions.
2.6 Statistical Analysis
Descriptive statistics were calculated using the SAS® software package, version 8.2 (SAS Institute Inc., Cary, NC, USA).
3 Results
Six healthy male subjects aged 27–42 years were recruited into the study, which took place over the 15-day period from 31 July to 14 August 2006, with screening on day 0, dosing on day 3 and day 10, and follow-up on day 14. All six subjects took a single dose of ciprofloxacin DPI 32.5 mg (corresponding to 50 mg dry powder) and a single dose of matching placebo, according to the randomly assigned treatment sequence. Baseline demographic characteristics are shown in Table 1. None of the subjects received any concomitant medication during the study, and study medication was correctly administered in hospital under the supervision of study personnel. All subjects completed the study and were included in the safety and pharmacokinetic analyses.
3.1 Safety and Tolerability
Transient mild dysgeusia was the only AE reported after any of the two single inhalational doses of study treatment, occurring in five subjects (four subjects with ciprofloxacin DPI, one subject with placebo). These were considered related to the study drug and this resolved within 30 min in all cases. No deaths or serious AEs were reported.
There were no laboratory values above the upper limit of normal that were clinically relevant after administration of ciprofloxacin DPI and there were no clinically relevant changes in blood pressure, heart rate or ECG parameters, including QT and QT interval corrected for heart rate in any subject.
Lung function parameters remained unchanged in five of six subjects. One subject experienced a transient marked reduction in FEV1 values after ciprofloxacin DPI treatment (FEV1 4.37 L pre-dose, 2.22 L 15 min post dose and 3.27 L 1 h post dose), without reporting bronchopulmonary clinical symptoms.
3.2 Pharmacokinetics
After a single dose of ciprofloxacin DPI, systemic ciprofloxacin was detected, with the plasma concentration of ciprofloxacin rising to 30–65 μg/L 15 min after inhalation, then stabilizing before starting to decline 1–1.5 h post inhalation (Fig. 2) with a terminal t ½ of 9.5 h (Fig. 3).
Non-compartmental pharmacokinetic parameters were calculated from the concentration–time curve (Table 2). Complete urine collection data sets that allowed measurement of the amount of ciprofloxacin excreted in urine were available in two subjects, for whom the percentage of urinary excretion (%Ae) within 48 h after inhalation was 21.4 and 26.9 % of the dose, respectively.
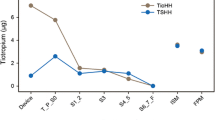
The modelled regional clearance data (PBPK) suggested that clearance of ciprofloxacin from the bronchotracheal tract was slower compared with that from the oral cavity or alveolar space (Fig. 4). The mean t ½ for mucociliary clearance fitted to the PBPK model was 10.8 h. According to the PBPK data, plasma ciprofloxacin was derived solely from ciprofloxacin deposited in the bronchotracheal tract by approximately 28 h post dosing (Fig. 4). Parameters fitted to the model for the regional deposition of ciprofloxacin are shown as mean percentages per individual in Fig. 5. The mean deposition of ciprofloxacin in the trachea/bronchi and alveolar space was 22.3 and 17.2 % of the total dose, respectively, with moderate inter-subject variability being observed (Fig. 5). Total ciprofloxacin deposition was 71.3 % of the dose.
Physiological pharmacokinetic modelling of the relative contributions of ciprofloxacin deposited in the oral cavity, alveolar space and trachea/bronchi to the total plasma concentration after a single dose of ciprofloxacin dry powder for inhalation 32.5 mg (n = 6). Lines represent the geometric means of the individual simulated curves for regional deposition and their summation. The filled circles show the geometric means of observed concentrations of ciprofloxacin in plasma
4 Discussion
Ciprofloxacin DPI was well tolerated in healthy subjects. This phase I trial raised no safety issues related to the mode of administration of the DPI relative to the safety profile of systemic ciprofloxacin treatment. AEs due to systemic ciprofloxacin did not occur nor would be expected from the low levels of systemic exposure to ciprofloxacin. Lung function parameters in healthy subjects remained in general unchanged, with no evidence of clinically relevant bronchopulmonary symptoms. The transient decrease in lung function observed in one study subject did not correlate with clinical symptoms. Overall, no evidence of local lung irritation or lung function deterioration was observed with ciprofloxacin DPI in healthy subjects, a major prerequisite for its long-term use.
Ciprofloxacin DPI is administered rapidly (<1 min) in a single inhalation using a low-resistance, capsule-based, portable, passive, dry powder inhaler (Novartis’ T-326 inhaler; Fig. 2). The resistance of the T-326 inhaler is approximately 0.08 cmH2O0.5·L/min, which is similar to other low-resistance devices such as the Aerolizer® (Merck), Diskus® (GlaxoSmithKline) or Turbuhaler® (AstraZeneca) [20]. The T-326 inhaler relies on the patient’s inspiratory effort to fluidize and disperse the powder [23], and data from other clinical studies have demonstrated that a minimal residue of ciprofloxacin remains after inhalation [27]. The rationale for studying therapy with an inhaled form of ciprofloxacin in patients with chronic respiratory diseases is to target the delivery of the drug directly to endobronchial infection areas while minimizing systemic exposure, which arises from either absorption across the alveolar epithelium or absorption from the gastrointestinal tract. Systemic exposure to ciprofloxacin was substantially lower than that previously observed with an oral dose of 750 mg ciprofloxacin (C max 56.42 μg/L, t max 0.625 h and AUC 354.4 μg·h/L compared with C max 2,690 μg/L 2 h after administration and AUC approximately 15,000 μg·h/L) [28].
In summary, the single dose of ciprofloxacin DPI was nominally 20 times lower than this oral therapeutic dose of ciprofloxacin, but the consequent systemic exposure was nominally 40 times lower [28]. Sputum concentrations of ciprofloxacin, specifically in the alveoli, were not measured in this study owing to the invasive nature of the procedure required to obtain induced sputum from healthy individuals and which would have interfered with the objective to assess lung tolerability of ciprofloxacin DPI without potential bias. However, high concentrations of ciprofloxacin were recorded in induced sputum from adult patients with CF who received ciprofloxacin DPI 32.5 mg compared with patients with CF who received oral ciprofloxacin 500 mg three times daily (C max 33 mg/L and geometric mean AUC 72.5 mg·h/L compared with C max 1.01 mg/L 2 h after administration and AUC from time zero to 8 h (AUC8) 4.86 mg·h/L) [29, 30]. This demonstrates the potential of ciprofloxacin DPI to deliver the target drug more efficiently for the treatment of respiratory infections than orally administered ciprofloxacin [28]. In addition, the PBPK evaluation of the results of this study provided further evidence of efficient lung targeting with ciprofloxacin DPI.
The observed t ½ of approximately 9.5 h was higher than the published values for oral or iv ciprofloxacin (4.11, 5.19 and 4.20 h for 250 mg oral, 750 mg oral and 200 mg iv doses of ciprofloxacin, respectively, in healthy subjects) [31, 32], suggesting that rate of absorption is the rate-limiting step that determines the terminal t ½ of the drug in plasma. The values calculated for CL/F and V z/F of 91.71 L/h and 1,262 L, respectively, were also higher than those reported in the literature for oral ciprofloxacin (Table 3). The results of the PBPK modelling are consistent with the possible explanation for this type of pharmacokinetic profile (i.e. slow and constant mucociliary clearance of the fraction of ciprofloxacin deposited in the trachea and bronchi of these healthy subjects—and its subsequent uptake via the gastrointestinal tract—prolonged the t ½). The mean mucociliary clearance t ½ that we fitted to the PBPK model is slightly greater than the terminal t ½ calculated from non-compartmental, model-independent analysis, but similar to that reported in the literature by Bondesson et al. who demonstrated a pulmonary elimination t ½ of 8 h 45 min for (99m)Tc-Nanocoll [35].
Several clinical studies have investigated the pharmacokinetic and pharmacodynamic benefits of dry powder antibacterials for inhalation because these may be more practical than nebulized liquid antibacterials and the very short time period required for dosing may improve patient compliance [19, 36–40]. Dry powder inhalation of colistin sulfomethate using a Twincer® inhaler (University of Groningen, Groningen, The Netherlands) was well tolerated but did not attain equivalent pulmonary deposition to liquid nebulization and required optimization of particle size and internal resistance [37, 38]. Inhalation of dry powder colistin sulfate proved an attractive alternative to nebulized colistin, although decreases in pulmonary function and moderate-to-severe coughing in some patients after inhalation indicates the need for further improvements in delivery [41]. Sputum concentrations of gentamicin were found to be similar after inhalation of dry powder gentamicin [39, 40] compared with gentamicin inhaled from a small-volume nebulizer.
A dry powder PulmoSphere™ formulation of tobramycin delivered by the same device as ciprofloxacin DPI has been well tolerated both in healthy subjects and in patients with CF, reaching a mean (±SD) C max of 0.60 ± 0.18 μg/mL 1–3 h after administration [19, 36]. Radiolabelling showed that a more consistent and reproducible dose was delivered from this device compared with a nebulizer, and that a higher percentage of the given dose was delivered to the lungs per inhalation [19]. Our modelling results suggest that ciprofloxacin DPI benefits from similar lung targeting. A single dose of ciprofloxacin DPI 32.5 mg equated to a nominal dose of 7.2 mg of ciprofloxacin to the trachea/bronchi and 5.6 mg to the alveolar space. Furthermore, efficient lung targeting with ciprofloxacin DPI could potentially have therapeutic advantages over tobramycin dry powder, given the greater potency of ciprofloxacin compared with tobramycin, as indicated by clinical minimum inhibitory concentration (MIC) distribution data [42] and two-fold higher MIC50 (MIC required to inhibit the growth of 50 % of organisms) values of tobramycin against clinical P. aeruginosa isolates from patients with CF compared with ciprofloxacin [12].
5 Conclusions
A single dose of ciprofloxacin DPI 32.5 mg was safe and well tolerated in healthy male adults. Systemic exposure to ciprofloxacin after a single inhaled dose was considerably smaller, and t ½, clearance and volume of distribution were greater than values reported in the literature for oral or iv administration of a therapeutic dose, reflecting effective lung deposition. Dry powder inhalers, such as the T-326 inhaler used for dosing ciprofloxacin DPI, are small, handheld devices that offer improved patient convenience relative to nebulized antibacterials, giving reduced size, fewer maintenance requirements, reduced administration time and room temperature stability [43]. These results suggest that ciprofloxacin DPI may provide a new therapeutic option for the management of patients with chronic pulmonary infections.
References
Sapey E, Stockley RA. COPD exacerbations. 2: aetiology. Thorax. 2006;61(3):250–8.
King PT, Holdsworth SR, Freezer NJ, et al. Microbiologic follow-up study in adult bronchiectasis. Respir Med. 2007;101(8):1633–8.
Moss RB. Cystic fibrosis: pathogenesis, pulmonary infection, and treatment. Clin Infect Dis. 1995;21:839–51.
Valderrey AD, Pozuelo MJ, Jimenez PA, et al. Chronic colonization by Pseudomonas aeruginosa of patients with obstructive lung diseases: cystic fibrosis, bronchiectasis, and chronic obstructive pulmonary disease. Diagn Microbiol Infect Dis. 2010;68(1):20–7.
Henry RL, Mellis CM, Petrovic L. Mucoid Pseudomonas aeruginosa is a marker of poor survival in cystic fibrosis. Pediatr Pulmonol. 1992;12(3):158–61.
Wilson CB, Jones PW, O’Leary CJ, et al. Effect of sputum bacteriology on the quality of life of patients with bronchiectasis. Eur Respir J. 1997;10(8):1754–60.
Kulich M, Rosenfeld M, Goss CH, et al. Improved survival among young patients with cystic fibrosis. J Pediatr. 2003;142(6):631–6.
Ramsey BW, Pepe MS, Quan JM, et al. Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. Cystic Fibrosis Inhaled Tobramycin Study Group. N Engl J Med. 1999;340(1):23–30.
Murray MP, Govan JR, Doherty CJ, et al. A randomized controlled trial of nebulized gentamicin in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2011;183(4):491–9.
Miravitlles M. Do we need new antibiotics for treating exacerbations of COPD? Ther Adv Respir Dis. 2007;1(1):61–76.
Geller DE. Comparing clinical features of the nebulizer, metered-dose inhaler, and dry powder inhaler. Respir Care. 2005;50(10):1313–21.
Ciofu O, Fussing V, Bagge N, et al. Characterization of paired mucoid/non-mucoid Pseudomonas aeruginosa isolates from Danish cystic fibrosis patients: antibiotic resistance, beta-lactamase activity and RiboPrinting. J Antimicrob Chemother. 2001;48(3):391–6.
Moss RB. Long-term benefits of inhaled tobramycin in adolescent patients with cystic fibrosis. Chest. 2002;121(1):55–63.
Sethi S, Jones PW, Theron MS, et al. Pulsed moxifloxacin for the prevention of exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. Respir Res. 2010;11:10.
Piddock LJ, Johnson M, Ricci V, et al. Activities of new fluoroquinolones against fluoroquinolone-resistant pathogens of the lower respiratory tract. Antimicrob Agents Chemother. 1998;42(11):2956–60.
Alder J, Wilson R, Welte T, et al. Antimicrobial efficacy of ciprofloxacin dry powder for inhalation in patients with non-cystic fibrosis bronchiectasis. Amsterdam: European Respiratory Society; 2011.
Endermann R, Labischinski H, Ladel C, et al. Treatment of bacterial diseases of the respiratory organs. US Patent 2004/0254194 A1. 2004.
Dellamary LA, Tarara TE, Smith DJ, et al. Hollow porous particles in metered dose inhalers. Pharm Res. 2000;17(2):168–74.
Newhouse MT, Hirst PH, Duddu SP, et al. Inhalation of a dry powder tobramycin PulmoSphere formulation in healthy volunteers. Chest. 2003;124(1):360–6.
Geller DE, Weers J, Heuerding S. Development of an inhaled dry-powder formulation of tobramycin using PulmoSphere technology. J Aerosol Med Pulm Drug Deliv. 2011;24(4):175–82.
Pharmacopoeia Online. 601 Aerosols, nasal sprays, metered-dose inhalers, and dry powder inhalers (online). http://www.uspbpep.com/usp31/v31261/usp31nf26s1_c601.asp. Accessed 16 Sept 2011.
European Pharmacopoeia 6.2. https://www.pheur.org/store/images/majbdd/200710301703120.6-2%20E%20Index.pdf. Accessed 16 Sept 2011.
Gupta A, Tarara T, Miller D, et al. A novel high-payload dry powder formulation of ciprofloxacin for management of chronic lung infections (abstract no. R6156). American Association of Pharmaceutical Scientists Annual Meeting, Washington; 23–27 Oct 2011.
Tiddens HA, Geller DE, Challoner P, et al. Effect of dry powder inhaler resistance on the inspiratory flow rates and volumes of cystic fibrosis patients of 6 years and older. J Aerosol Med. 2006;19(4):456–65.
Willmann S, Hohn K, Edginton A, et al. Development of a physiology-based whole-body population model for assessing the influence of individual variability on the pharmacokinetics of drugs. J Pharmacokinet Pharmacodyn. 2007;34(3):401–31.
Willmann S, Lipworth BJ, Sevestre M, et al. PK-Sim: a physiologically based pharmacokinetic ‘whole-body’ model. Biosilico. 2003;1(4):121–4.
Wilson R, Welte T, Polverino E, et al. Ciprofloxacin DPI in non-cystic fibrosis bronchiectasis: a phase II randomised study. Eur Respir J. 2012. doi:10.1183/09031936.00071312.
Gonzalez MA, Uribe F, Moisen SD, et al. Multiple-dose pharmacokinetics and safety of ciprofloxacin in normal volunteers. Antimicrob Agents Chemother. 1984;26(5):741–4.
Stass H, Baumann-Noss S, Delesen H, et al. Pharmacokinetics of inhaled ciprofloxacin powder (abstract no. P103). In: Proceedings of 31st European Cystic Fibrosis Conference, Prague; 11–14 June 2008.
Smith MJ, White LO, Bowyer H, et al. Pharmacokinetics and sputum penetration of ciprofloxacin in patients with cystic fibrosis. Antimicrob Agents Chemother. 1986;30(4):614–6.
Plaisance KI, Drusano GL, Forrest A, et al. Effect of dose size on bioavailability of ciprofloxacin. Antimicrob Agents Chemother. 1987;31(6):956–8.
Drusano GL, Standiford HC, Plaisance K, et al. Absolute oral bioavailability of ciprofloxacin. Antimicrob Agents Chemother. 1986;30(3):444–6.
Forrest A, Weir M, Plaisance KI, et al. Relationships between renal function and disposition of oral ciprofloxacin. Antimicrob Agents Chemother. 1988;32(10):1537–40.
Wingender W, Graefe KH, Gau W, et al. Pharmacokinetics of ciprofloxacin after oral and intravenous administration in healthy volunteers. Eur J Clin Microbiol. 1984;3(4):355–9.
Bondesson E, Bengtsson T, Nilsson LE, et al. Site of deposition and absorption of an inhaled hydrophilic solute. Br J Clin Pharmacol. 2007;63(6):722–31.
Geller DE, Konstan MW, Smith J, et al. Novel tobramycin inhalation powder in cystic fibrosis subjects: pharmacokinetics and safety. Pediatr Pulmonol. 2007;42(4):307–13.
Westerman EM, de Boer AH, Le Brun PP, et al. Dry powder inhalation of colistin sulphomethate in healthy volunteers: a pilot study. Int J Pharm. 2007;335(1–2):41–5.
Westerman EM, de Boer AH, Le Brun PP, et al. Dry powder inhalation of colistin in cystic fibrosis patients: a single dose pilot study. J Cyst Fibros. 2007;6(4):284–92.
Crowther Labiris NR, Holbrook AM, Chrystyn H, et al. Dry powder versus intravenous and nebulized gentamicin in cystic fibrosis and bronchiectasis. A pilot study. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1711–6.
Goldman JM, Bayston SM, O’Connor S, et al. Inhaled micronised gentamicin powder: a new delivery system. Thorax. 1990;45(12):939–40.
Le Brun PP, de Boer AH, Mannes GP, et al. Dry powder inhalation of antibiotics in cystic fibrosis therapy: part 2. Inhalation of a novel colistin dry powder formulation: a feasibility study in healthy volunteers and patients. Eur J Pharm Biopharm. 2002;54(1):25–32.
EUCAST. European Committee on Antimicrobial Susceptibility Testing. MIC distribution (online). http://www.eucast.org. Accessed 1 Jan 2011.
Weers J, Clark A, Challoner P. High dose inhaled powder delivery: challenges and techniques. In: Respiratory Drug Delivery IX: River Grove: Amy Davis Biggs 2004; pp 281–8.
Acknowledgments
Bayer Pharma AG funded this study and was responsible directly or through appointed agents for its design, conduct, data collection, statistical analysis and preparation of a clinical study report, which was verified by the Principal Investigator, S. Baumann. Sponsor review of the manuscript was agreed by the authors who retained full control over the content. H. Delesen, J. Nagelschmitz and H. Stass are employees of Bayer Pharma AG. S. Willmann is an employee of Bayer Technology Services GmbH, A. Gupta is an employee of Novartis Pharmaceuticals Corporation, and S. Baumann is an employee of CRS Clinical Research Services Mannheim GmbH. The authors wish to acknowledge Sarah Birch of Chameleon Communications International, who provided medical writing services with funding from Bayer Pharma AG.
Author information
Authors and Affiliations
Corresponding author
Additional information
European clinical trials database reference: 2006-001594-26.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited. The exclusive right to any commercial use of the article is with Springer.
About this article
Cite this article
Stass, H., Nagelschmitz, J., Willmann, S. et al. Inhalation of a Dry Powder Ciprofloxacin Formulation in Healthy Subjects: A Phase I Study. Clin Drug Investig 33, 419–427 (2013). https://doi.org/10.1007/s40261-013-0082-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-013-0082-0