Abstract
Background
In India, more than two-thirds of the total health expenditure is incurred through out-of-pocket expenditure (OOPE) by households. Morbidity events thus impose excessive financial risk on households. The Sustainable Development Goals Target 3.8 specifies financial risk protection for achieving universal health coverage (UHC) in developing countries. This study aimed to estimate the impact of OOPE on catastrophic health expenditure (CHE) and impoverishment effects by types of morbidity in India.
Methods
Data came from the 75th round of the National Sample Survey (NSS) on the theme ‘Social consumption in India: Health’, which was conducted during the period from July 2017 to June 2018. For the present study, 56,722 households for hospitalisation, 29,580 households for outpatient department (OPD) care and 6285 households for both (OPD care and hospitalisation) were analysed. Indices, namely health care burden, CHE, poverty head count ratio and poverty gap ratio using standard definitions were analysed.
Results
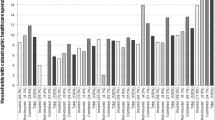
Households with members who underwent treatment for cancers, cardiovascular diseases, psychiatric conditions, injuries, musculoskeletal and genitourinary conditions spent a relatively high amount of their income on health care. Overall, 41.4% of the households spent > 10% of the total household consumption expenditure (HCE) and 24.6% of households spent > 20% of HCE for hospitalisation. A total of 20.4% and 10.0% of households faced CHE for hospitalisation based on the average per capita and average two capita consumption expenditure, respectively. Health care burden, CHE and impoverishment was higher in households who sought treatment in private health facilities than in public health facilities.
Conclusion
Our study suggests that there is an urgent need for political players and policymakers to design health system financing policies and strict implementation that will provide financial risk protection to households in India.

Similar content being viewed by others
References
India State-Level Disease Burden Initiative Collaboration. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease study. Lancet. 2017;390(10111):2437–60.
Dhara VR, Schramm PJ, Luber G. Climate change and infectious diseases in India: implications for healthcare providers. Indian J Med Res. 2013;138(6):847–52.
Menon GRM, Singh L, Sharma P, Yadav P, Sharma S, Kalaskar S, et al. National burden estimates of healthy lives lost in India, 2017: an analysis using direct mortality data and indirect disability data. Lancet Global Health. 2019;7(12):E1675–84.
National Health Systems Resource Centre. National Health Accounts Estimates for India (2016–17). New Delhi: Ministry of Health and Family Welfare, Government of India; 2019.
Kastor A, Mohanty SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PloS One. 2018;13(5):e0196106.
Sangar S, Dutt V, Thakur R. Comparative assessment of economic burden of disease in relation to out of pocket expenditure. Front Public Health. 2019. https://doi.org/10.3389/fpubh.2019.00009.
Bonu S, Bhushan I, Rani M, Anderson I. Incidence and correlates of “catastrophic” maternal health care expenditure in India. Health Policy Plan. 2009;24:445–56.
Garg CC, Karan AK. Reducing out-of-pocket expenditures to reduce poverty: a disaggregated analysis at rural-urban and state level in India. Health Policy Plan. 2009;24:116–28.
Berman P, Ahuja R, Bhandari L. The impoverishing effect of healthcare payments in India: new methodology and findings. Econ Political Wkly. 2010;45:65–71.
Mohanty SK, Kastor A. Out-of-pocket expenditure and catastrophic health spending on maternal care in public and private health centres in India: a comparative study of pre and post national health mission period. Health Econ Rev. 2017;31(7):1–15.
Tripathy JP, Prasad BM, Shewade HD, Kumar AMV, Zachariah R, Chadha S, et al. Cost of hospitalisation for non-communicable diseases in India: are we pro-poor? Trop Med Int Health. 2016;21:1019–28.
Karan A, Engelgau M, Mahal A. The economic implications of non-communicable disease for India: Health, Nutrition and Population (HNP) discussion paper. Washington: World Bank; 2010.
Rajpal S, Kumar A, Joe W. Economic burden of cancer in India: evidence from cross-sectional nationally representative household survey, 2014. PloS One. 2018;13(2):e0193320.
Mitra S, Findley PA, Rd EF, Hall D. Healthcare expenditures of living with a disability: total expenditures, out of pocket expenses and burden, 1996–2004. In: Discussion Paper No: 2008–18 September 2008. Fordham University, New York
Sahoo AK, Madheswaran S. Socio-economic disparities in health care seeking behaviour, health expenditure and its source of financing in Orissa. J Health Manag. 2014;16:397–414.
Government of India. Key indicators of social consumption in India: Health. New Delhi: National Sample Survey Organisation; 2019.
Kwesiga B, Zikusooka CM, Ataguba JE. Assessing catastrophic and impoverishing effects of health care payments in Uganda. BMC Health Serv Res. 2015;15:30.
Aregbeshola BS, Khan SM. Out-of-pocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010. Int J Health Policy Manag. 2018;7:798–806.
O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington: The World Bank; 2007.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–7.
Wagstaff A, Flores G, Smitz MF, Hsu J, Chepynoga K, Eozenou P. Progress on impoverishing health spending in 122 countries: a retrospective observational study. Lancet Global Health. 2018;6:e180–92.
Berki SE. A look at catastrophic medical expenses and the poor. Health Aff. 1986;5:138–45.
Russell S. The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. Am J Tropic Med Hygiene. 2004;71(2_suppl):147–155.
Mataria A, Raad F, Abu-Zaineh M, Donaldson C. Catastrophic healthcare payments and impoverishment in the occupied palestinian territory. Appl Health Econ Health Policy. 2010;8:393–405.
Somkotra T, Lagrada LP. Which households are at risk of catastrophic health spending: experience in Thailand after universal coverage: exploring the reasons why some households still incur high levels of spending—even under universal coverage—can help policymakers devise solutions. Health Affairs. 2009;28(Suppl1):w467–78.
Van Doorslaer E, O’Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16:1159–84.
Kumar K, Singh A, Kumar S, Ram F, Singh A, Ram U, et al. Socio-economic differentials in impoverishment effects of out-of-pocket health expenditure in China and India: evidence from WHO SAGE. PLoS ONE. 2015;10:e0135051.
Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health Econ. 2003;12:921–33.
Joe W, Rajpal S. Unravelling the socioeconomic gradient in the incidence of catastrophic health care expenditure: a comment. Health Policy Plan. 2018;33:699–701.
Ravendran G. A review of Rangarajan committee report on poverty estimation. Indian J Hum Dev. 2016;10(1):85–96.
State Level Consumer Price Index (Rural/Urban) upto August 2018. Open Government Data (OGD) Platform India 2020, Apr 29. https://data.gov.in/resources/state-level-consumer-price-index-ruralurban-upto-august-2018. Accessed 20 May 2020.
Bajwala VR, John D, Rajasekar TD, Murhekar MV. Severity and costs associated with hospitalization for dengue in public and private hospitals of Surat city, Gujarat, India, 2017–2018. Trans R Soc Trop Med Hyg. 2019;113:661–9.
Appleton S, Emwanu T, Kagugube J, Muwonge J. Changes in poverty in Uganda, 1992–1997: No. 1999–22. Oxford: Centre for the Study of African Economies; 1999.
Levine S. Exploring differences in national and international poverty estimates: is Uganda on track to halve poverty by 2015? Soc Indic Res. 2012;107(2):331–49.
Van Minh H, Xuan TB. Assessing the household financial burden associated with the chronic non-communicable diseases in a rural district of Vietnam. Global Health Act. 2012;5:1–7.
Deaton A, Zaidi S. Directrices para construir agregados de consumo para analizar el bienestar. Washington: Banco Mundial; 2002.
World Health Organization. Impact of out-of-pocket payments for treatment of non-communicable diseases in developing countries: a review of literature. Geneva: World Health Organization; 2011.
Wesson HKH, Boikhutso N, Bachani AM, Hofman KJ, Hyder AA. The cost of injury and trauma care in low- and middle-income countries: review of economic evidence. Health Policy Plan. 2014;29:795–808.
Joe W. Distressed financing of household out-of-pocket health care payments in India: incidence and correlates. Health Policy Plan. 2015;30:728–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
The present study utilised household-level data from current NSS 75th round survey on the theme ‘Social consumption in India: Health’. The NSS is a countrywide large-scale population-based survey organisation under the Ministry of Statistics and Programme Implementation (MoSPI), Government of India. The NSS obtained ethical consensus from the review committee of the project while in the second stage, consent was taken from the respondents and duly undersigned, and only once he/she had agreed to participate in the study was any data collected. This study utilised secondary data that is accessible in the public domain and this dataset does not include any personal information of respondents.
Conflict of interest
None declared.
Consent
The study results presented here do not involve human subject research, hence consent was not required.
Funding
Our study did not use any funding for conducting data acquisition and analysis.
Data availability statement
Our study utilised the NSS 75th round survey data, which is publicly accessible to individuals both countrywide and worldwide on http://www.mospi.gov.in/.
Author Contributions
JY conceived the idea for the study and developed the analysis plan. JY led the analysis and organised the first draft of manuscript. JY, DJ and GRM conducted data interpretation and manuscript writing. GRM, DJ and JY read and approved the preliminary manuscript. All authors approved the final version of the manuscript.
Acknowledgements
The author acknowledges the National Sample Survey Organisation (SSSO), MOSPI, India, for data collection and providing data for analysis.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yadav, J., Menon, G.R. & John, D. Disease-Specific Out-of-Pocket Payments, Catastrophic Health Expenditure and Impoverishment Effects in India: An Analysis of National Health Survey Data. Appl Health Econ Health Policy 19, 769–782 (2021). https://doi.org/10.1007/s40258-021-00641-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-021-00641-9