Abstract
Background
The introduction of efficiency-oriented provider payment systems in inpatient mental healthcare in various Western countries may lead to the use of less healthcare resources in the treatment of patients. To avoid unintended effects on quality of care that may result from reductions in resource utilization, it is essential for decision and policy makers to know whether there is a trade-off between costs and quality of care.
Aim of the Study
The aim of this study was to investigate and quantify the relationship between costs and outcomes in psychosomatic inpatients with somatoform pain disorder.
Methods
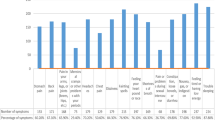
The inclusion criteria for patient selection (n = 101) were (i) a main diagnosis of somatoform pain disorder according to International Classification of Diseases-10 (ICD-10) [F45.4, F45.40, F45.41]; (ii) complete data on the mental component summary reflecting overall functioning of mental health (MCS-8) measured with the Short Form-8 Health Survey (SF-8) within 3 days of the admission and discharge dates; and (iii) treatment at Charité Universitaetsmedizin (Berlin, Germany) during the period January 2006–June 2010. The change in the MCS-8 score incurred over the treatment period was used as an indicator of quality of care. Treatment costs were calculated from the provider’s perspective, mainly using bottom-up micro-costing. The year of valuation for cost calculation was 2008 (with no inflation adjustment); for costs provided by the accounting department for services consumed by the patient, the valuation year was based on the year of service provision. We hypothesized that the outcome ‘change in MCS-8 score’ was a function of the independent variable costs, patient characteristics, socio-demographic variables, pain-related variables, co-morbidities and subjective illness attribution, i.e. whether patients attributed the origin of pain mainly to a somatic cause or not. An interaction term between costs and illness attribution was included to control for the hypothesized differing effects of resource input or costs on the outcome variable conditional on patients’ illness attribution. Hausman tests indicated that endogeneity was not present, thus, ordinary least squares regression (OLS) was conducted. We assessed whether the change in the MCS-8 score was clinically meaningful and perceptible by the patient, using the minimal clinical important difference (MCID). For Short Form Health Surveys, the MCID for changes in the mental component summary is typically around 3 points.
Results
We found a trade-off between costs and outcome for patients without or with only minor somatic illness attribution (77 % of the sample). This patient group improved 0.4 points in outcome after every 100 € increase in total costs per case (F 1,77 = 13.836, t(77) = 3.72, p = 0.0004). For patients with mainly somatic illness beliefs (23 % of the sample), we did not find a trade-off between costs and outcome.
Conclusion
For the majority of patients, we found a trade-off between costs and health outcome, thus, it seems advisable to carefully monitor outcome parameters when applying cost containment measures.

Similar content being viewed by others
References
Drozd EM, Cromwell J, Gage B, et al. Patient casemix classification for medicare psychiatric prospective payment. Am J Psychiatry. 2006;163:724–32.
Geissler A, Quentin W. Prospective payment for inpatient psychiatric care. Health Policy Monitor, 2010. http://www.hpm.org/en/Surveys/TU_Berlin_-_D/15/Prospective_payment_for_inpatient_psychiatric_care.html. Accessed 2012 Oct 15.
Mason A, Goddard M. Payment by results in mental health: a review of the international literature and an economic assessment of the approach in the English NHS. University of York, 2009. http://www.york.ac.uk/che/pdf/rp50.pdf. Accessed 2012 Oct 15.
Schreyoegg J, Stargardt T. The trade-off between costs and outcomes: the case of acute myocardial infarction. Health Serv Res. 2010;45:1585–601.
Cots F, Chiarello P, Salvador X, et al. DRG-based hospital payment: intended and unintended consequences. In: Busse R, Geissler A, Quentin W, et al., editors. Diagnosis-related groups in Europe. Berkshire: McGraw-Hill Open University Press; 2011. p. 75–92.
Fleming ST. The relationship between quality and cost: pure and simple? Inquiry. 1991;28:29–387.
Carey K, Burgess JF Jr. On measuring the hospital cost/quality trade-off. Health Econ. 1999;8:509–20.
Mukamel DB, Spector WD. Nursing home costs and risk-adjusted outcome measures of quality. Med Care. 2000;38:78–89.
Stargardt T, Schreyoegg J, Kondofersky I. Measuring the relationship between costs and outcomes: the example of acute myocardial infarction in German hospitals. Health Econ. 2013. doi:10.1002/hec.2941
Romley JA, Jena AB, Goldman DP. Hospital spending and inpatient mortality: evidence from California: an observational study. Ann Intern Med. 2011;154:160–7.
Stukel TA, Fisher ES, Alter DA, et al. Association of hospital spending intensity with mortality and readmission rates in Ontario hospitals. J Am Med Assoc. 2012;307:1037–45.
Jha AK, Orav EJ, Dobson A, et al. Measuring efficiency: the association of hospital costs and quality of care. Health Aff. 2009;28:897–906.
Lagu T, Rothberg MB, Nathanson BH, et al. The relationship between hospital spending and mortality in patients with sepsis. Arch Intern Med. 2011;171:292–9.
Chen LM, Jha AK, Guterman S, et al. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med. 2010;170:340–6.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization, 1993. http://www.who.int/classifications/icd/en/GRNBOOK.pdf. Accessed 2013 Jun 25.
Froehlich C, Jacobi F, Wittchen HU. DSM-IV pain disorder in the general population. Eur Arch Psychiatry Clin Neurosci. 2006;256:187–96.
Grabe HJ, Meyer C, Hapke U, et al. Somatoform pain disorder in the general population. Psychother Psychosom. 2003;72:88–94.
Hiller W, Fichter MM, Rief W. A controlled treatment study of somatoform disorders including analysis of healthcare utilization and cost-effectiveness. J Psychosom Res. 2003;54:369–80.
Rost K, Kashner TM, Smith GR. Effectiveness of psychiatric intervention with somatization disorder patients: improved outcomes at reduced costs. Gen Hosp Psychiatry. 1994;16:381–7.
Escobar JI, Golding JM, Hough RL, et al. Somatization in the community: relationship to disability and use of services. Am J Pub Health. 1987;77:837–40.
Shaw J, Creed F. The cost of somatization. J Psychosom Res. 1991;35:307–12.
Treurniet HF, Essink-Bot ML, Mackenbach JP, et al. Health-related quality of life: an indicator of quality of care? Qual Life Res. 1997;6:363–9.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. J Am Med Assoc. 1995;273:59–65.
Tan SS, Rutten FF, van Ineveld BM, et al. Comparing methodologies for the cost estimation of hospital services. Eur J Health Econ. 2009;10:39–45.
Donabedian A. Basic approaches to assessment: structure, process and outcome. Explorations in Quality Assessment and Monitoring. 1980;1:75–125.
Donabedian A. Evaluating the quality of medical care. Milbank Quart. 2005;83:691–729.
Patrick DL, Bergner M. Measurement of health status in the 1990s. Annu Rev Public Health. 1990;11:165–83.
Ebrahim S. Clinical and public health perspectives and applications of health-related quality of life measurement. Soc Sci Med. 1995;41:1383–94.
Ware JE Jr. The status of health assessment 1994. Annu Rev Public Health. 1995;16:327–54.
Kilbourne AM, Keyser D, Pincus HA. Challenges and opportunities in measuring the quality of mental health care. Can J Psychiatry. 2010;55:549–57.
Martin M, Blaisdell-Gross B, Fortin EW, et al. Health-related quality of life of heart failure and congestive artery disease patients improved during participation in disease management programs: a longitudinal observational study. Dis Manag. 2007;10:164–78.
Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15:523–30.
Ware JE, Kosinski M, Dewey JE, et al. How to score and interpret single-item health status measures: a manual for users of the of the SF-8 Health Survey. Lincoln: Qual Metr; 2001.
Turner-Bowker DM, Bayliss MS, Ware JE, et al. Usefulness of the SF-8 Health Survey for comparing the impact of migraine and other conditions. Qual Life Res. 2003;12:1003–12.
Walker DR, Landis DL, Stern PM, et al. Disease management positively affects patient quality of life. Manag Care Interface. 2003;16:56–60.
Lefante JJ, Harmon GN, Ashby KM, et al. Use of the SF-8 to assess health-related quality of life for a chronically ill, low-income population participating in the Central Louisiana Medication Access Program (CMAP). Qual Life Res. 2005;14:665–73.
Wooldridge JM. Econometric analysis of cross section and panel data. Cambridge: MIT Press; 2002.
Hausman JA. Specification tests in econometrics. Econometrica. 1978;46:1251–71.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum; 1988.
Samsa G, Edelman D, Rothman ML, et al. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15:141–55.
Ware JE. User’s manual for the SF-36v2 Health Survey. Lincoln: Qual Metr; 2007.
Huber D, Albrecht C, Hautum A, et al. Effectiveness of inpatient psychodynamic psychotherapy: a follow-up study. Z Psychosom Med Psyc. 2009;55:189.
Haase M, Frommer J, Franke GH, et al. From symptom relief to interpersonal change: treatment outcome and effectiveness in inpatient psychotherapy. Psychother Res. 2008;18:615–24.
Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007;69:881–8.
Sattel H, Lahmann C, Guendel H, et al. Brief psychodynamic interpersonal psychotherapy for patients with multisomatoform disorder: randomised controlled trial. Br J Psychiatry. 2012;200:60–7.
Duddu V, Isaac MK, Chaturvedi SK. Somatization, somatosensory amplification, attribution styles and illness behaviour: a review. Int Rev Psychiatry. 2006;18:25–33.
Rief W, Nanke A, Emmerich J, et al. Causal illness attributions in somatoform disorders: associations with comorbidity and illness behavior. J Psychosom Res. 2004;57:367–71.
Groben S, Hausteiner C. Somatoform disorders and causal attributions in patients with suspected allergies: do somatic causal attributions matter? J Psychosom Res. 2011;70:229–38.
Wise TN, Mann LS. The attribution of somatic symptoms in psychiatric outpatients. Compr Psychiatry. 1995;36:407–10.
Kirmayer LJ, Robbins JM. Patients who somatize in primary care: a longitudinal study of cognitive and social characteristics. Psychol Med. 1996;26:937–51.
Mant J. Process versus outcome indicators in the assessment of quality of health care. Int J Qual Health Care. 2001;13(6):475–80.
Zeeck A, Wietersheim J, Hartmann, et al. Inpatient or day clinic treatment? Results of a multi-site-study. GMS Psycho Soc Med. 2009. doi:10.3205/psm000059.
Acknowledgments
This work was planned and written up by Laura Haas, Tom Stargardt, Jonas Schreyoegg, Rico Schlösser, Gerhard Danzer and Burghard F. Klapp, and the final version of the manuscript was approved by all the authors. The conceptual work was mainly done by Tom Stargardt, Jonas Schreyoegg and Laura Haas. Rico Schlösser was responsible for the data collection process, and Gerhard Danzer and Burghard F. Klapp provided all of the medical information. Rico Schlösser calculated part of the costs. Laura Haas was responsible for the data analysis and for drafting the manuscript, supported by Tom Stargardt and Jonas Schreyoegg. The results were interpreted by all authors. The guarantor for the overall content is Laura Haas. There was no external funding for this study, and none of the authors has any potential conflicts of interests that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haas, L., Stargardt, T., Schreyoegg, J. et al. The Trade-off Between Costs and Quality of Care in the Treatment of Psychosomatic Patients with Somatoform Pain Disorder. Appl Health Econ Health Policy 11, 359–368 (2013). https://doi.org/10.1007/s40258-013-0042-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-013-0042-0