Abstract
Background and Objectives
Prior research has documented that Alzheimer’s disease (AD) is associated with increased costs from comorbid conditions. However, little is known about medical resource utilization and costs among AD patients prior to the onset of cognitive symptoms. This study estimates excess acute care costs among Medicaid AD patients in the year prior to diagnosis.
Study Design
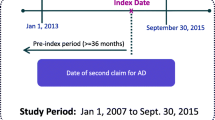
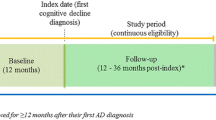
Administrative claims data for New Jersey Medicaid patients over the period 1997–2010 were retrospectively analyzed. The study focused on non-institutionalized AD patients and examined their medical costs compared with matched controls with no dementia over the 12 months prior to their preliminary diagnosis. Costs reflect amounts reimbursed by Medicaid to medical service providers, reported in 2010 US dollars.
Results
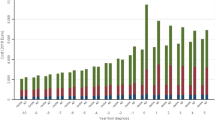
The study sample included 11,536 AD patients who were matched to controls. Average age was 76 years, and 76.2 % were female. Compared with matched controls, total medical costs over the 12-month pre-index period were US$ 5,549 higher among AD patients (US$ 14,977 vs. US$ 9,428, p < 0.001), of which US$ 3,321 (p < 0.001) was due to outpatient services. Home care and medical daycare services accounted for US $1,442 (p < 0.001) of the difference. Emergency department visits and inpatient care accounted for only a small fraction of the excess costs.
Conclusions
Compared with controls, Medicaid AD patients incurred higher acute care costs in the 12 months prior to their preliminary diagnosis, suggesting room for beneficial interventions and better disease management should earlier diagnosis become possible. These findings may be especially relevant in light of new criteria facilitating earlier diagnosis of AD.

Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev., Washington: American Psychiatric Association; 2000.
Jack CR Jr, Albert MS, Knopman DS, et al. Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):257–62 (Epub 2011 Apr 21).
United States Preventive Services Task Force. The guide to clinical preventive services. Rockville: Agency for Healthcare Research and Quality; 2005.
Valcour VG, Masaki KH, Curb JD, et al. The detection of dementia in the primary care setting. Arch Intern Med. 2000;160(19):2964–8.
Boise L, Neal MB, Kaye J. Dementia assessment in primary care: results from a study in three managed care systems. J Gerontol A Biol Sci Med Sci. 2004;59(6):M621–6.
Magsi H, Malloy T. Underrecognition of cognitive impairment in assisted living facilities. J Am Geriatr Soc. 2005;53(2):295–8.
Sternberg SA, Wolfson C, Baumgarten M. Undetected dementia in community-dwelling older people: the Canadian Study of Health and Aging. J Am Geriatr Soc. 2000;48(11):1430–4.
Liu-Ambrose TY, Ashe MC, Graf P, et al. Increased risk of falling in older community-dwelling women with mild cognitive impairment. Phys Ther. 2008;88(12):1482–91. doi:10.2522/ptj.20080117 (Epub 2008.Sep.26).
Kiecolt-Glaser JK, Glaser R, Shuttleworth EC, et al. Chronic stress and immunity in family caregivers of Alzheimer’s disease victims. Psychosom Med. 1987;49(5):523–35.
Zarit S. The hidden victims of Alzheimer’s disease: families under stress. New York: NYU Press; 1985.
Mega MS, Cummings JL, Fiorello T, et al. The spectrum of behavioral changes in Alzheimer’s disease. Neurology. 1996;46(1):130–5.
Hill JW, Futterman R, Duttagupta S, et al. Alzheimer’s disease and related dementias increase costs of comorbidities in managed Medicare. Neurology. 2002;58(1):62–70.
McCarten JR, Anderson P, Kuskowski MA, et al. Changes in outpatient costs following screening and diagnosis of cognitive impairment. Alzheimers Dement. 2010;6(4 Supplement):e19.
Knopman D, Schneider L, Davis K, Talwalker S, Smith F, Hoover T, et al. Long-term tacrine (Cognex) treatment: effects on nursing home placement and mortality. Neurology. 1996;47:166–77.
Geldmacher DS, Provenzano G, McRae T, Mastey V, Ieni JR. Donepezil is associated with delayed nursing home placement in patients with Alzheimer’s disease. J Am Geriatr Soc. 2003;51(7):937–44.
Lopez OL, Becker JT, Saxton J, Sweet RA, Klunk W, DeKosky ST. Alteration of a clinically meaningful outcome in the natural history of Alzheimer’s disease by cholinesterase inhibition. J Am Geriatr Soc. 2005;53(1):83–7.
Feldman HH, Pirttila T, Dartigues JF, Everitt B, Van Baelen B, Schwalen S, et al. Treatment with galantamine and time to nursing home placement in Alzheimer’s disease patients with and without cerebrovascular disease. Int J Geriatr Psychiatry. 2009;24(5):479–88.
Courtney C, Farrell D, Gray R, Hills R, Lynch L, Sellwood E, et al. Long-term donepezil treatment in 565 patients with Alzheimer’s disease (AD2000): randomised double-blind trial. Lancet. 2004;363:2105–15.
Rascati KL, Smith MJ, Neilands T. Dealing with skewed data: an example using asthma-related costs of Medicaid clients. Clin Ther. 2001;23:481–98.
Efron B, Tibshirani RJ. An introduction to the bootstrap. New York: Chapman and Hall; 1993.
Taylor DH Jr, Sloan FA. How much do persons with Alzheimer’s disease cost Medicare? J Am Geriatr Soc. 2000;48(6):639–46.
Harriet M, Lamb HM, Goa KL. Rivastigmine: a pharmacoeconomic review of its use in Alzheimer’s disease. Pharmacoeconomics. 2001;19(3):303–18.
Steele C, Rovner B, Chase GA, Folstein M. Psychiatric symptoms and nursing home placement of patients with Alzheimer’s disease. Am J Psychiatry. 1990;147(8):1049–51.
Geldmacher DS, Kirson NY, Birnbaum HG, et al. Implications of early treatment among Medicaid patients with Alzheimer’s disease. Alzheimers Dement. 2013. doi:10.1016/j.jalz.2013.01.015
Iliffe S, Robinson L, Brayne C, et al. Primary care and dementia: 1. diagnosis, screening and disclosure. Int J Geriatr Psychiatry. 2009;24(9):895–901. doi:10.1002/gps.2204.
Vandenberghe R, Van Laere K, Ivanoiu A, et al. 18F-flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: a phase 2 trial. Ann Neurol. 2010;68(3):319–29.
Clark CM, Schneider JA, Bedell BJ, et al. Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA. 2011;305(3):275–83.
Barthel H, Gertz HJ, Dresel S, et al. Cerebral amyloid-β PET with florbetaben (18F) in patients with Alzheimer’s disease and healthy controls: a multicentre phase 2 diagnostic study. Lancet Neurol. 2011;10(5):424–35.
Acknowledgments
Research funding provided to Analysis Group, Inc., by Bayer HealthCare Pharmaceuticals. Dr. Geldmacher received support from Bayer HealthCare Pharmaceuticals through contractual agreement with the University of Alabama-Birmingham. Ms. Cummings and Drs. Kirson, Birnbaum and Eapen are employees of Analysis Group, Inc. Mr. Kantor was an employee of Analysis Group, Inc., at the time of conducting the analysis. Dr. Joish is an employee of Bayer HealthCare Pharmaceuticals. Drs. Geldmacher, Kirson, Birnbaum and Eapen, Mr. Kantor and Ms. Cummings were involved in the design, conduct, execution, analysis, review of the study and manuscript preparation. Dr. Joish contributed to the design, review of the study and manuscript preparation. Dr. Kirson is the guarantor for the overall content.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Geldmacher, D.S., Kirson, N.Y., Birnbaum, H.G. et al. Pre-Diagnosis Excess Acute Care Costs in Alzheimer’s Patients among a US Medicaid Population. Appl Health Econ Health Policy 11, 407–413 (2013). https://doi.org/10.1007/s40258-013-0038-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-013-0038-9