Abstract
Background
Alopecia areata (AA) is a complex autoimmune condition resulting in nonscarring hair loss. In recent years, many studies have provided new evidence on comorbid diseases present in patients with AA. However, some studies have conflicting results, and analyses conducting a comprehensive approach are lacking.
Objective
The aim of our study was to provide an updated systematic review and meta-analysis of medical comorbidities associated with AA.
Methods
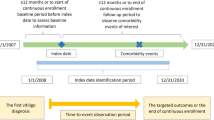
We searched PubMed, Embase, and Web of Science for case-control, cross-sectional, and cohort studies investigating medical comorbidities in AA published from inception through 1 February 2023.
Results
We screened 3428 abstracts and titles and reviewed 345 full text articles for eligibility. Ultimately, 102 studies were analyzed, comprising 680,823 patients with AA and 72,011,041 healthy controls. Almost all included studies (100 of 102 studies) were of satisfactory to high quality (Newcastle–Ottawa scale score ≥ 4). Among patients with AA, comorbidities with the highest odds ratios (OR) compared with healthy controls and data available from more than one study included vitamin D deficiency (OR 10.13, 95% CI 4.24–24.20), systemic lupus erythematous (OR 5.53, 95% CI 3.31–9.23), vitiligo (OR 5.30, 95% CI 1.86–15.10), metabolic syndrome (OR 5.03, 95% CI 4.18–6.06), and Hashimoto’s thyroiditis (OR 4.31, 95% CI 2.51–7.40). AA may be a protective factor for certain disorders, for which the AA group had lower odds compared with healthy controls, such as irritable bowel syndrome (OR 0.38, 95% CI 0.14–0.99) and colorectal cancer (OR 0.61, 95% CI 0.42–0.89).
Conclusion
These findings corroborate and contextualize the risks across comorbidities for patients with AA. Further work should be done to identify the underlying pathophysiology and understand appropriate screening criteria.



Similar content being viewed by others
References
Strazzulla LC, Wang EHC, Avila L, Lo Sicco K, Brinster N, Christiano AM, et al. Alopecia areata: disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78:1–12. https://doi.org/10.1016/J.JAAD.2017.04.1141.
Benigno M, Anastassopoulos KP, Mostaghimi A, Udall M, Daniel SR, Cappelleri JC, et al. A large cross-sectional survey study of the prevalence of alopecia areata in the United States. Clin Cosmet Investig Dermatol. 2020;13:259. https://doi.org/10.2147/CCID.S245649.
Lee HH, Gwillim E, Patel KR, Hua T, Rastogi S, Ibler E, et al. Epidemiology of alopecia areata, ophiasis, totalis, and universalis: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82:675–82.
Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1 percent by Rochester Epidemiology Project, 1990–2009. J Invest Dermatol. 2014;134:1141–2.
Safavi KH, Muller SA, Suman VJ, Moshell AN, Melton III LJ. Incidence of alopecia areata in Olmsted County, Minnesota, 1975 through 1989. In: Mayo Clin Proc. 1995. p. 628–33.
Gandhi K, Shy ME, Ray M, Fridman M, Vaghela S, Mostaghimi A. The association of alopecia areata-related emotional symptoms with work productivity and daily activity among patients with alopecia areata. Dermatol Ther. 2023;13:285–98. https://doi.org/10.1007/s13555-022-00864-1.
Mostaghimi A, Gao W, Ray M, Bartolome L, Wang T, Carley C, et al. Trends in prevalence and incidence of alopecia areata, alopecia totalis, and alopecia universalis among adults and children in a US employer-sponsored insured population. JAMA Dermatol. 2023;159:411–8. https://doi.org/10.1001/jamadermatol.2023.0002.
Colón EA, Popkin MK, Callies AL, Dessert NJ, Hordinsky MK. Lifetime prevalence of psychiatric disorders in patients with alopecia areata. Compr Psychiatry. 1991;32:245–51.
Ghanizadeh A. Comorbidity of psychiatric disorders in children and adolescents with alopecia areata in a child and adolescent psychiatry clinical sample. Int J Dermatol. 2008;47:1118–20.
Hussain ST, Mostaghimi A, Barr PJ, Brown JR, Joyce C, Huang KP. Utilization of mental health resources and complementary and alternative therapies for alopecia areata: a U.S. Survey. Int J Trichol. 2017;9:160–4. https://doi.org/10.4103/ijt.ijt_53_17.
Li SJ, Huang KP, Joyce C, Mostaghimi A. The impact of alopecia areata on sexual quality of life. Int J Trichol. 2018;10:271–4. https://doi.org/10.4103/ijt.ijt_93_18.
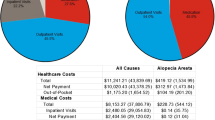
Mostaghimi A, Xenakis J, Meche A, Smith TW, Gruben D, Sikirica V. Economic burden and healthcare resource use of alopecia areata in an insured population in the USA. Dermatol Ther. 2022;12:1027–40.
Huang KP, Mullangi S, Guo Y, Qureshi AA. Autoimmune, atopic, and mental health comorbid conditions associated with alopecia areata in the United States. JAMA Dermatol. 2013;149:789–94. https://doi.org/10.1001/jamadermatol.2013.3049.
Villasante Fricke AC, Miteva M. Epidemiology and burden of alopecia areata: a systematic review. Clin Cosmet Investig Dermatol. 2015. p. 397–403.
Chu SY, Chen YJ, Tseng WC, Lin MW, Chen TJ, Hwang CY, et al. Comorbidity profiles among patients with alopecia areata: the importance of onset age, a nationwide population-based study. J Am Acad Dermatol. 2011;65:949–56. https://doi.org/10.1016/j.jaad.2010.08.032.
Goh C, Finkel M, Christos PJ, Sinha AA. Profile of 513 patients with alopecia areata: associations of disease subtypes with atopy, autoimmune disease and positive family history. J Eur Acad Dermatology Venereol. 2006;20:1055–60. https://doi.org/10.1111/j.1468-3083.2006.01676.x.
Lee S, Lee H, Lee CH, Lee W-S. Comorbidities in alopecia areata: A systematic review and meta-analysis. J Am Acad Dermatol. 2019;80:466-477.e16. https://doi.org/10.1016/j.jaad.2018.07.013.
Xing L, Dai Z, Jabbari A, Cerise JE, Higgins CA, Gong W, et al. Alopecia areata is driven by cytotoxic T lymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20:1043–9.
Petukhova L, Duvic M, Hordinsky M, Norris D, Price V, Shimomura Y, et al. Genome-wide association study in alopecia areata implicates both innate and adaptive immunity. Nature. 2010;466:113–7.
Betz RC, Petukhova L, Ripke S, Huang H, Menelaou A, Redler S, et al. Genome-wide meta-analysis in alopecia areata resolves HLA associations and reveals two new susceptibility loci. Nat Commun. 2015;6:5966.
McElwee KJ, Hoffmann R. Alopecia areata—animal models. Clin Exp Dermatol. 2002;27:410–7. https://doi.org/10.1046/j.1365-2230.2002.01075.x.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. https://doi.org/10.1136/BMJ.N71.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. https://doi.org/10.1136/bmj.j4008.
Ly S, Kamal K, Manjaly P, Mostaghimi A. Systematic review of comorbidities in alopecia areata. PROSPERO Int Prospect Regist Syst Rev. 2022;CRD4202235.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford; 2000.
Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS ONE. 2016;11: e0147601.
RStudio Team. RStudio: integrated development for R. Boston: RStudio, PBC; 2020.
Serarslan G, Savaş N, Yenin JZ. Is atopy and autoimmunity more prevalent in patients with alopecia areata? A comparative study. J Eur Acad Dermatol Venereol. 2012;26:720–3. https://doi.org/10.1111/j.1468-3083.2011.04152.x.
Wang S, Shohat T, Vadheim C, Shellow W, Edwards J, Rotter JI. Increased risk for type I (insulin-dependent) diabetes in relatives of patients with alopecia areata (AA). Am J Med Genet. 1994;51:234–9.
Huang KP, Joyce CJ, Topaz M, Guo Y, Mostaghimi A. Cardiovascular risk in patients with alopecia areata (AA): a propensity-matched retrospective analysis. J Am Acad Dermatol. 2016;75:151–4. https://doi.org/10.1016/j.jaad.2016.02.1234.
Garzorz N, Alsisi M, Todorova A, Atenhan A, Thomas J, Lauffer F, et al. Dissecting susceptibility from exogenous triggers: the model of alopecia areata and associated inflammatory skin diseases. J Eur Acad Dermatol Venereol. 2015;29:2429–35.
Kridin K, Renert-Yuval Y, Guttman-Yassky E, Cohen AD. Alopecia areata is associated with atopic diathesis: results from a population-based study of 51,561 patients. J Allergy Clin Immunol Pr. 2020;8:1323-1328.e1. https://doi.org/10.1016/j.jaip.2020.01.052.
Jagielska D, Redler S, Brockschmidt FF, Herold C, Pasternack SM, Bartels NG, et al. Follow-up study of the first genome-wide association scan in alopecia areata: IL13 and KIAA0350 as susceptibility loci supported with genome-wide significance. J Invest Dermatol. 2012;132:2192–7.
Harris JE, Harris TH, Weninger W, Wherry EJ, Hunter CA, Turka LA. A mouse model of vitiligo with focused epidermal depigmentation requires IFN-γ for autoreactive CD8+ T-cell accumulation in the skin. J Invest Dermatol. 2012;132:1869–76.
Bertolini M, McElwee K, Gilhar A, Bulfone-Paus S, Paus R. Hair follicle immune privilege and its collapse in alopecia areata. Exp Dermatol. 2020;29:703–25.
Paus R, Bulfone-Paus S, Bertolini M. Hair follicle immune privilege revisited: the key to alopecia areata management. In: J Investig Dermatology Symp Proc. 2018. p. S12–7.
Rajabi F, Drake LA, Senna MM, Rezaei N. Alopecia areata: a review of disease pathogenesis. Br J Dermatol. 2018;179:1033–48.
Song T, Pavel AB, Wen H-C, Malik K, Estrada Y, Gonzalez J, et al. An integrated model of alopecia areata biomarkers highlights both TH1 and TH2 upregulation. J Allergy Clin Immunol. 2018;142:1631–4.
Gilhar A. Alopecia areata induced in C3H/HeJ mice by interferon-gamma: evidence for loss of immune privilege. J Invest Dermatol. 2005;124:288–9.
Guttman-Yassky E, Renert-Yuval Y, Bares J, Chima M, Hawkes JE, Gilleaudeau P, et al. Phase 2a randomized clinical trial of dupilumab (anti-IL-4Rα) for alopecia areata patients. Allergy. 2022;77:897–906.
King B, Mostaghimi A, Shimomura Y, Zlotogorski A, Choi G-S, Blume-Peytavi U, et al. Integrated safety analysis of baricitinib in adults with severe alopecia areata from two randomized clinical trials. Br J Dermatol. 2022;ljac059.
King B, Ohyama M, Kwon O, Zlotogorski A, Ko J, Mesinkovska NA, et al. Two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386:1687–99.
Betz RC, Pforr J, Flaquer A, Redler S, Hanneken S, Eigelshoven S, et al. Loss-of-function mutations in the filaggrin gene and alopecia areata: strong risk factor for a severe course of disease in patients comorbid for atopic disease. J Invest Dermatol. 2007;127:2539–43.
Li SF, Zhang XT, Qi SL, Ye YT, Cao H, Yang YQ, et al. Allergy to dust mites may contribute to early onset and severity of alopecia areata. Clin Exp Dermatol. 2015;40:171–6.
Ito T, Kageyama R, Nakazawa S, Honda T. Understanding the significance of cytokines and chemokines in the pathogenesis of alopecia areata. Exp Dermatol. 2020;29(8):726–32. https://doi.org/10.1111/exd.14129.
Wei YH, Tai YH, Dai YX, Chang YT, Chen TJ, Chen MH. Bidirectional association between alopecia areata and atopic dermatitis: a population-based cohort study in Taiwan. Clin Exp Allergy. 2020;50:1406–14. https://doi.org/10.1111/cea.13729.
Thatiparthi A, Martin A, Suh S, Yale K, Atanaskova MN. Inflammatory ocular comorbidities in alopecia areata: a retrospective cohort study of a single academic center. J Am Acad Dermatol. 2022. https://doi.org/10.1016/j.jaad.2022.06.018.
Magen E, Chikovani T, Waitman DA, Kahan NR. Association of alopecia areata with atopic dermatitis and chronic spontaneous urticaria. Allergy Asthma Proc. 2018;39:96–102. https://doi.org/10.2500/aap.2018.39.4114.
Thomas EA, Kadyan RS. Alopecia areata and autoimmunity: a clinical study. Indian J Dermatol. 2008;53(2):70–4. https://doi.org/10.4103/0019-5154.41650.
Conic RZ, Miller R, Piliang M, Bergfeld W, Atanaskova MN. Comorbidities in patients with alopecia areata. J Am Acad Dermatol. 2017;76:755–7. https://doi.org/10.1016/j.jaad.2016.12.007.
Barahmani N, Schabath MB, Duvic M. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581–91. https://doi.org/10.1016/J.JAAD.2009.04.031.
Ali NS, Tollefson MM, Lohse CM, Torgerson RR. Incidence and comorbidities of pediatric alopecia areata: a retrospective matched cohort study using the Rochester Epidemiology Project. J Am Acad Dermatol. 2022;87:427–9. https://doi.org/10.1016/j.jaad.2021.08.050.
Holmes S, Harries M, Macbeth AE, Chiu WS, de Lusignan S, Messenger AG, et al. Alopecia areata and risk of atopic and autoimmune conditions: population-based cohort study. Clin Exp Dermatol. 2022. https://doi.org/10.1093/ced/llac104.
Egeberg A, Anderson S, Edson-Heredia E, Burge R. Comorbidities of alopecia areata: a population-based cohort study. Clin Exp Dermatol. 2021;46:651–6. https://doi.org/10.1111/ced.14507.
Yale K, Nourmohammadi N, Casale F, Ghigi A, Zheng K, Mesinkovska NA. A year in review: a cross-sectional study of alopecia areata and risk of COVID-19 infection, hospitalization, and mortality from March 2020–February 2021. Int J Dermatol. 2022;61:e81–3. https://doi.org/10.1111/ijd.15970.
Conic RZ, Tamashunas NL, Damiani G, Fabbrocini G, Cantelli M, Bergfeld WF. Comorbidities in pediatric alopecia areata. J Eur Acad Dermatol Venereol. 2020;34:2898–901. https://doi.org/10.1111/jdv.16727.
Campos-Alberto E, Hirose T, Napatalung L, Ohyama M. Prevalence, comorbidities, and treatment patterns of Japanese patients with alopecia areata: a descriptive study using Japan medical data center claims database. J Dermatol. 2023;50:37–45. https://doi.org/10.1111/1346-8138.16615.
Goksin S. Retrospective evaluation of clinical profile and comorbidities in patients with alopecia areata. North Clin Istanbul. 2022;9:451–8. https://doi.org/10.14744/nci.2022.78790.
Phong CH, McMichael AJ, Mesinkovska NA. Epidemiology of alopecia areata in Hispanic/Latinx patients. J Am Acad Dermatol. 2022. https://doi.org/10.1016/j.jaad.2022.10.049.
Mostaghimi A, Gandhi K, Done N, Ray M, Gao W, Carley C, et al. All-cause health care resource utilization and costs among adults with alopecia areata: a retrospective claims database study in the United States. J Manag Care Spec Pharm. 2022;28:426–34. https://doi.org/10.18553/jmcp.2022.28.4.426.
Elsherif NA, El-Dibany SA, Greiw AS. Study of total serum immunoglobulin e level and prevalence of atopy in alopecia areata patients. Iran J Dermatol. 2021;24:80–4. https://doi.org/10.22034/ijd.2021.132451.
Lee H, Kim YC, Choi JW. Alopecia areata is not a risk factor for heart diseases: a 10-year retrospective cohort study. PLoS ONE. 2021;16: e0250216.
Conic RRZ, Chu S, Tamashunas NL, Damiani G, Bergfeld W. Prevalence of cardiac and metabolic diseases among patients with alopecia areata. J Eur Acad Dermatol Venereol. 2021;35:e128–9. https://doi.org/10.1111/jdv.16864.
Karadag AS, Ertugrul DT, Bilgili SG, Takci Z, Tutal E, Yilmaz H. Insulin resistance is increased in alopecia areata patients. Cutan Ocul Toxicol. 2013;32:102–6. https://doi.org/10.3109/15569527.2012.713418.
Dai YX, Tai YH, Chen CC, Chang YT, Chen TJ, Chen MH. Bidirectional association between alopecia areata and sleep disorders: a population-based cohort study in Taiwan. Sleep Med. 2020;75:112–6. https://doi.org/10.1016/j.sleep.2020.06.015.
Cho SI, Yu DA, Kim SI, Lee SM, Kwon O. Pregnancy outcomes in female patients with alopecia areata: a nationwide population-based study. J Invest Dermatol. 2021;141:1844-1847.e4. https://doi.org/10.1016/j.jid.2020.12.014.
Sharma VK, Kumar B, Dawn G. A clinical study of childhood alopecia areata in Chandigarh, India. Pediatr Dermatol. 1996;13:372–7. https://doi.org/10.1111/j.1525-1470.1996.tb00703.x.
Abdollahimajd F, Niknezhad N, Bahreini N, Younespour S, Namazi N. Metabolic syndrome in patients with Alopecia Areata: a case-control study. Dermatol Ther. 2021;34: e14979. https://doi.org/10.1111/dth.14979.
Shin JW, Kang T, Lee JS, Kang MJ, Huh CH, Kim MS, et al. Time-dependent risk of acute myocardial infarction in patients with alopecia areata in Korea. JAMA Dermatol. 2020;156:763–71. https://doi.org/10.1001/jamadermatol.2020.1133.
Chen CH, Wang KH, Lin HC, Chung SD. Follow-up study on the relationship between alopecia areata and risk of autoimmune diseases. J Dermatol. 2016;43:228–9. https://doi.org/10.1111/1346-8138.13165.
Chung PI, Hwang CY, Chen YJ, Lin MW, Chen TJ, Hua TC, et al. Autoimmune comorbid diseases associated with lichen planus: a nationwide case-control study. J Eur Acad Dermatol Venereol. 2015;29:1570–5. https://doi.org/10.1111/jdv.12939.
Kridin K, Shalom G, Comaneshter D, Cohen AD. Is there an association between alopecia areata and systemic lupus erythematosus? A population-based study. Immunol Res. 2020;68:1–6. https://doi.org/10.1007/s12026-020-09115-x.
Kridin K, Tzur Bitan D, Comaneshter D, Cohen AD. The prevalence of systemic sclerosis is increased among patients with alopecia areata: a population-based study. Immunol Res. 2019;67:368–72. https://doi.org/10.1007/s12026-019-09104-9.
Schneeweiss MC, Kirchgesner J, Wyss R, Jin Y, York C, Merola JF, et al. Occurrence of inflammatory bowel disease in patients with chronic inflammatory skin diseases: a cohort study: classification: epidemiology. Br J Dermatol. 2022;187:692–703. https://doi.org/10.1111/bjd.21704.
Messenger AG, Harries M, Macbeth AE, Chiu WS, Holmes S, Tziotzios C, et al. Alopecia areata and risk of common infections: a population-based cohort study. Clin Exp Dermatol. 2022. https://doi.org/10.1093/ced/llac106.
Mostaghimi A, Qureshi S, Joyce C, Guo Y, Huang KP. Reduced incidence of skin cancer in patients with alopecia areata: a retrospective cohort study. Cancer Epidemiol. 2016;41:129–31. https://doi.org/10.1016/j.canep.2016.02.009.
Sharma VK, Dawn G, Kumar B. Profile of alopecia areata in Northern India. Int J Dermatol. 1996;35:22–7. https://doi.org/10.1111/j.1365-4362.1996.tb01610.x.
Saniee S, Zare AG, Radmehr A. Thyroid dysfunction in alopecia areata. Turk J Endocrinol Metab. 2019;23:92–6. https://doi.org/10.25179/tjem.2018-63547.
Seo HM, Han SS, Kim JS. Cancer risks among patients with alopecia areata: a population-based case-control study in Korea. J Am Acad Dermatol. 2018;78:209–11. https://doi.org/10.1016/j.jaad.2017.08.011.
Dai YX, Tai YH, Chang YT, Chen TJ, Chen MH. Bidirectional association between alopecia areata and thyroid diseases: a nationwide population-based cohort study. Arch Dermatol Res. 2021;313:339–46. https://doi.org/10.1007/s00403-020-02109-7.
Grandolfo M, Biscazzi AM, Pipoli M. Alopecia areata and autoimmunity. G Ital di Dermatol Venereol. 2008;143:277–81.
Díaz-Angulo S, López-Hoyos M, Muñoz-Cacho P, López-Escobar M, González-López MA. High prevalence of thyroid autoimmunity in patients with alopecia areata and vitiligo: a controlled study. Australas J Dermatol. 2015;56:142–3. https://doi.org/10.1111/ajd.12321.
Pandhi D, Singal A, Gupta R, Das G. Ocular alterations in patients of alopecia areata. J Dermatol. 2009;36:262–8. https://doi.org/10.1111/j.1346-8138.2009.00636.x.
Bin Saif GA. Severe subtype of alopecia areata is highly associated with thyroid autoimmunity. Saudi Med J. 2016;37:656–61. https://doi.org/10.15537/Smj.2016.6.13777.
Marahatta S, Agrawal S, Mehata KD. Alopecia areata and thyroid dysfunction association—a study from Eastern Nepal. Kathmandu Univ Med J (KUMJ). 2018;16:161–5.
Lewinski A, Broniarczyk-Dyla G, Sewerynek E, Zerek-Melen G, Szkudlinski M. Abnormalities in structure and function of the thyroid gland in patients with alopecia areata. J Am Acad Dermatol. 1990;23:768–9.
Wang H, Gan H, Mei L, Yang G, Fang F. The association between alopecia areata and thyroid autoimmunity in Chinese adult patients: a controlled study. Biomed Res. 2017;28:3517–21.
Abdel-Hafez HZ, Mahran AM, Hofny ER, Attallah DA, Sayed DS, Rashed HA. Is Helicobacter pylori infection associated with alopecia areata? J Cosmet Dermatol. 2009;8:52–5. https://doi.org/10.1111/j.1473-2165.2009.00424.x.
Conic RZ, Rambhia P, Atanaskova-Mesinkovska N, Piliang M, Bergfeld W. Lack of an association between alopecia areata and visceral or hematopoietic cancers. J Am Acad Dermatol. 2017;77:981–2. https://doi.org/10.1016/j.jaad.2017.06.045.
Li CY, Tai YH, Dai YX, Chang YT, Bai YM, Tsai SJ, et al. Association of alopecia areata and the risk of dementia: a nationwide cohort study. J Clin Psychiatry. 2021. https://doi.org/10.4088/JCP.21m13931.
Schneeweiss MC, Kirchgesner J, Wyss R, Jin Y, York C, Merola JF, et al. Occurrence of inflammatory bowel disease in patients with chronic inflammatory skin diseases: a cohort study. Br J Dermatol. 2022. https://doi.org/10.1111/bjd.21704.
Shakoei S, Torabimirzaee A, Saffarian Z, Abedini R. Sleep disturbance in alopecia areata: a cross-sectional study. Health Sci Rep. 2022. https://doi.org/10.1002/hsr2.576.
Erdoğan HK, Acer E, Hakkı A, Bulur I, İncesulu A, Pınarbaşlı Ö, et al. Evaluation of hearing with pure-tone audiometry in alopecia areata patients. Turkderm Turk Arch Dermatol Venereol. 2019;53:19–23.
Ucak H, Soylu E, Ozturk S, Demir B, Cicek D, Erden I, et al. Audiological abnormalities in patients with alopecia areata. J Eur Acad Dermatol Venereol. 2014;28:1045–8. https://doi.org/10.1111/jdv.12259.
Aksu Cerman A, Sarikaya Solak S, Kivanc AI. Vitamin D deficiency in alopecia areata. Br J Dermatol. 2014;170:1299–304. https://doi.org/10.1111/bjd.12980.
Thatiparthi A, Martin A, Suh S, Yale K, Mesinkovska NA. Inflammatory ocular comorbidities in alopecia areata: a retrospective cohort study of a single academic center. J Am Acad Dermatol. 2023;88:221–3.
Noso S, Park C, Babaya N, Hiromine Y, Harada T, Ito H, et al. Organ specificity in autoimmune diseases: thyroid and islet autoimmunity in alopecia areata. J Clin Endocrinol Metab. 2015;100:1976–83. https://doi.org/10.1210/jc.2014-3985.
Arousse A, Boussofara L, Mokni S, Gammoudi R, Saidi W, Aounallah A, et al. Alopecia areata in Tunisia: epidemio-clinical aspects and comorbid conditions. A prospective study of 204 cases. Int J Dermatol. 2019;58:811–5. https://doi.org/10.1111/ijd.14381.
Senna M, Ko J, Tosti A, Edson-Heredia E, Fenske DC, Ellinwood AK, et al. Alopecia areata treatment patterns, healthcare resource utilization, and comorbidities in the US population using insurance claims. Adv Ther. 2021;38:4646–58. https://doi.org/10.1007/s12325-021-01845-0.
Shellow WV, Edwards JE, Koo JY. Profile of alopecia areata: a questionnaire analysis of patient and family. Int J Dermatol. 1992;31:186–9. https://doi.org/10.1111/j.1365-4362.1992.tb03932.x.
Mahjoub TT. The clinico-epidemiological profile of alopecia areata: a hospital-based study in Jeddah, Saudi Arabia. J Dermatol Dermatol Surg. 2020;24:122–4. https://doi.org/10.4103/jdds.jdds_77_19.
Lee HJ, Hong NS, Kim SH, Jang YH. Association between alopecia areata and comorbid allergies: implications for its clinical course. Ann Dermatol. 2020;32:523–5. https://doi.org/10.5021/ad.2020.32.6.523.
Farajzadeh S, Rahnama Z, Esfandiarpour I, Tardast A, Hasheminasab S, Damavandi FD, et al. Clinical and demographic profile of childhood alopecia areata in Iran. J Pak Assoc Dermatol. 2013;23:20–7.
Cho HH, Jo SJ, Paik SH, Jeon HC, Kim KH, Eun HC, et al. Clinical characteristics and prognostic factors in early-onset alopecia totalis and alopecia universalis. J Korean Med Sci. 2012;27:799–802. https://doi.org/10.3346/jkms.2012.27.7.799.
Wohlmuth-Wieser I, Osei JS, Norris D, Price V, Hordinsky MK, Christiano A, et al. Childhood alopecia areata—data from the National Alopecia Areata Registry. Pediatr Dermatol. 2018;35:164–9. https://doi.org/10.1111/pde.13387.
Saceda-Corralo D, Grimalt R, Fernández-Crehuet P, Clemente A, Bernárdez C, García-Hernandez MJ, et al. Beard alopecia areata: a multicentre review of 55 patients. J Eur Acad Dermatol Venereol. 2017;31:187–92. https://doi.org/10.1111/jdv.13896.
Achar A, Rathi SK, Kumrah L, Biswas R, Bisai S. Clinico-epidemiological study of alopecia areata. J Pak Assoc Dermatol. 2018;28:168–74.
Legiawati L, Suseno LS, Sitohang IBS, Pratama AI. Hair disorder in dr. Cipto Mangunkusumo cosmetic dermatology and venereology outpatient clinic of Jakarta, Indonesia: a socio-demographic and clinical evaluation. Dermatol Rep. 2022;14:9341. https://doi.org/10.4081/dr.2022.9341.
You HR, Kim SJ. Factors associated with severity of alopecia areata. Ann Dermatol. 2017;29:565–70. https://doi.org/10.5021/ad.2017.29.5.565.
Vañó-Galván S, Fernández-Crehuet P, Grimalt R, Garcia-Hernandez MJ, Rodrigues-Barata R, Arias-Santiago S, et al. Alopecia areata totalis and universalis: a multicenter review of 132 patients in Spain. J Eur Acad Dermatol Venereol. 2017;31:550–6. https://doi.org/10.1111/jdv.13959.
Sorrell J, Petukhova L, Reingold R, Christiano A, Garzon M. Shedding light on alopecia areata in pediatrics: a retrospective analysis of comorbidities in children in the National Alopecia Areata Registry. Pediatr Dermatol. 2017;34:e271–2. https://doi.org/10.1111/pde.13238.
Shahzadi N, Pal SS, Asad F, Rani Z, Khurshid K. Frequency of autoimmune disorders in patients of alopecia areata. J Pak Assoc Dermatol. 2016;26:112–7.
Ro BI. Alopecia areata in Korea (1982–1994). J Dermatol. 1995;22:858–64. https://doi.org/10.1111/j.1346-8138.1995.tb03936.x.
Rangu S, Rogers R, Castelo-Soccio L. Understanding alopecia areata characteristics in children under the age of 4 years. Pediatr Dermatol. 2019;36:854–8. https://doi.org/10.1111/pde.13990.
Lee NR, Kim BK, Yoon NY, Lee SY, Ahn SY, Lee WS. Differences in comorbidity profiles between early-onset and late-onset alopecia areata patients: a retrospective study of 871 Korean patients. Ann Dermatol. 2014;26:722–6. https://doi.org/10.5021/ad.2014.26.6.722.
Wang S, Ratnaparkhi R, Piliang M, Bergfeld WF. Role of family history in patchy alopecia areata. Dermatol Online J. 2018;24(10):13030/qt0n19r7ps.
Tan E, Tay YK, Goh CL, Giam YC. The pattern and profile of alopecia areata in Singapore—a study of 219 Asians. Int J Dermatol. 2002;41:748–53. https://doi.org/10.1046/j.1365-4362.2002.01357.x.
Ranawaka RR. An observational study of alopecia areata in Sri Lankan adult patients. Ceylon Med J. 2014;59:128–31. https://doi.org/10.4038/cmj.v59i4.7865.
Puavilai S, Puavilai G, Charuwichitratana S, Sakuntabhai A, Sriprachya-Anunt S. Prevalence of thyroid diseases in patients with alopecia areata. Int J Dermatol. 1994;33:632–3. https://doi.org/10.1111/j.1365-4362.1994.tb02921.x.
Lyakhovitsky A, Aronovich A, Gilboa S, Baum S, Barzilai A. Alopecia areata: a long-term follow-up study of 104 patients. J Eur Acad Dermatol Venereol. 2019;33:1602–9. https://doi.org/10.1111/jdv.15582.
Lyakhovitsky A, Gilboa S, Eshkol A, Barzilai A, Baum S. Late-onset alopecia areata: a retrospective cohort study. Dermatology. 2018;233:289–94. https://doi.org/10.1159/000481881.
Ejaz A, Jameel K, Suhail M. Pattern and profile of alopecia areata in Pakistan. J Pak Assoc Dermatol. 2009;19:136–40.
De Weert J, Temmerman L, Kint A. Alopecia areata: a clinical study. Dermatologica. 1984;168:224–9. https://doi.org/10.1159/000249708.
Lopes ASA, Santos LDN, Razé MC, Lazzarini R. Alopecia areata: descriptive analysis in a Brazilian sample. An Bras Dermatol. 2022;97:654–6. https://doi.org/10.1016/j.abd.2021.04.016.
Kumar B, Sharma VK, Sehgal S. Antismooth muscle and antiparietal cell antibodies in Indians with alopecia areata. Int J Dermatol. 1995;34:542–5. https://doi.org/10.1111/j.1365-4362.1995.tb02949.x.
Park SM, Oh YJ, Lew BL, Sim WY. The association among thyroid dysfunction, thyroid autoimmunity, and clinical features of alopecia areata: a retrospective study. J Am Acad Dermatol. 2019;81:602–5. https://doi.org/10.1016/j.jaad.2018.04.051.
Schepis C, Barone C, Danzuso GCL, Romano C. Alopecia areata in Down syndrome: a clinical evaluation [5]. J Eur Acad Dermatol Venereol. 2005;19:769–70. https://doi.org/10.1111/j.1468-3083.2005.01259.x.
Thomas EA, Kadyan RS. Alopecia areata and autoimmunity: a clinical study. Indian J Dermatol. 2008;53:70–4. https://doi.org/10.4103/0019-5154.41650.
Sharma MK, Gupta S, Kumar R, Singhal AK, Jain SK, Sharma M. A clinico-epidemiological study of scalp hair loss in children (0–18 years) in Kota Region South-East Rajasthan. Indian J Dermatol. 2019;64:285–91.
Friedmann PS. Alopecia areata and auto-immunity. Br J Dermatol. 1981;105:153–7. https://doi.org/10.1111/j.1365-2133.1981.tb01200.x.
Ertekin V, Selimoglu MA, Altinkaynak S. Celiac disease in childhood: evaluation of 140 patients. Eurasian J Med. 2009;41:154–7.
Ertekin V, Tosun MS, Erdem T. Screening of celiac disease in children with alopecia areata. Indian J Dermatol. 2014;59:317. https://doi.org/10.4103/0019-5154.131468.
Rigopoulos D, Katsambas A, Karalexis A, Papatheodorou G, Rokkas T. No increased prevalence of Helicobacter pylori in patients with alopecia areata. J Am Acad Dermatol. 2002;46:141. https://doi.org/10.1067/mjd.2002.117255.
Sharma VK, Sialy R, Kumar B, Gupta S. Evaluation of thyroid function in north Indians with alopecia areata: response to intravenous injection of 100 micrograms thyrotropin releasing hormone (TRH). J Dermatol. 1999;26:339–42. https://doi.org/10.1111/j.1346-8138.1999.tb03484.x.
Kurtev A, Iliev E. Thyroid autoimmunity in children and adolescents with alopecia areata. Int J Dermatol. 2005;44:457–61. https://doi.org/10.1111/j.1365-4632.2005.01971.x.
Lyakhovitsky A, Shemer A, Amichai B. Increased prevalence of thyroid disorders in patients with new onset alopecia areata. Australas J Dermatol. 2015;56:103–6. https://doi.org/10.1111/ajd.12178.
Nanda A, Alsaleh QA, Al-Hasawi F, Al-Muzairai I. Thyroid function, autoantibodies, and HLA tissue typing in children with alopecia areata. Pediatr Dermatol. 2002;19:486–91. https://doi.org/10.1046/j.1525-1470.2002.00216.x.
Ahmed I, Nasreen S, Jehangir U, Wahid Z. Clinical spectrum of alopecia areata and its association with thyroid dysfunction. J Pak Assoc Dermatol. 2012;22:207–12.
Seyrafi H, Akhiani M, Abbasi H, Mirpour S, Gholamrezanezhad A. Evaluation of the profile of alopecia areata and the prevalence of thyroid function test abnormalities and serum autoantibodies in Iranian patients. BMC Dermatol. 2005;5:11. https://doi.org/10.1186/1471-5945-5-11.
Lo Sicco K, McGuire S, English Iii JC. A retrospective study of thyroid structural abnormalities in alopecia patients. Dermatoendocrinol. 2011;3:251–4.
Cunliffe WJ, Hall R, Stevenson CJ, Weightman D. Alopecia areata, thyroid disease and autoimmunity. Br J Dermatol. 1969;81:877–81. https://doi.org/10.1111/j.1365-2133.1969.tb15967.x.
Baars MP, Greebe RJ, Pop VJ. High prevalence of thyroid peroxidase antibodies in patients with alopecia areata. J Eur Acad Dermatol Venereol. 2013;27:e137–9. https://doi.org/10.1111/j.1468-3083.2011.04420.x.
Asgher R, Luqman N, Almas U, Akhlaq F, Khalid M, Shaheen JA. Alopecia aeata: clinical spectrum and its association with thyroid dysfunction in Bahawalpur. J Pak Assoc Dermatol. 2020;30:9–12.
Rodriguez TA, Duvic M. Onset of alopecia areata after Epstein-Barr virus infectious mononucleosis. J Am Acad Dermatol. 2008;59:137–9. https://doi.org/10.1016/j.jaad.2008.02.005.
Inui S, Hamasaki T, Itami S. Sleep quality in patients with alopecia areata: questionnaire-based study. Int J Dermatol. 2014;53:e39-41. https://doi.org/10.1111/j.1365-4632.2012.05570.x.
Siddiqui Z, Rashid RM, Mirmirani P. Vitamin D deficiency in an alopecia referral clinic during a 3-month period: the need to pursue systemic screening. Skinmed. 2017;15:339–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study did not receive any funding.
Conflict of interest
AM declares financial interest and a position on the advisory board of Fig. 1 Beauty, Inc., Eli Lilly and Company, Pfizer Inc., and Hims. AM receives fees as a consultant from AbbVie, Concert Pharmaceuticals, Pfizer Inc., and 3Derm Systems. AM is the founder of Lucid, Inc. and receives research funding from Incyte Corporation, Aclaris Therapeutics Inc., Eli Lilly and Company and Concert Pharmaceuticals. All other authors declare no conflict of interest.
Ethics approval
Not applicable.
Consent to participate/publish
Not applicable.
Availability of data and material
No datasets were generated or analyzed for the current study.
Code availability
Not applicable.
Author contributions
All authors contributed to the study design. The search strategy development and literature search were performed by S.L., C.M, and A.M. Data collection and interpretation were conducted by S.L., P.M., K.K., A.S., B.W., N.A., L.D., K.S., S.G., and A.M. Statistical analysis was performed by S.L. and G.Z. The manuscript was drafted by S.L. and critically revised by all other authors. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ly, S., Manjaly, P., Kamal, K. et al. Comorbid Conditions Associated with Alopecia Areata: A Systematic Review and Meta-analysis. Am J Clin Dermatol 24, 875–893 (2023). https://doi.org/10.1007/s40257-023-00805-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-023-00805-4