Abstract
Atopic dermatitis is a common, chronic, immune-mediated disease associated with several comorbidities. Elevated levels of T helper (Th)2, Th22, and also some Th1 and Th17 cytokines are found in atopic dermatitis skin lesions. Similar to psoriasis, there is a tendency towards increased use of more targeted therapies. However, there are still several unmet needs in the treatment of atopic dermatitis concerning long-term efficacy, tolerability, safety, route of administration, and cost. The increased knowledge of atopic dermatitis pathogenesis and the role of Janus kinase/signal transducer and activator of transcription (JAK/STAT) pathways has allowed the development of new compounds to inhibit this intracellular signaling pathway implicated in atopic dermatitis-related immune responses. Currently, JAK inhibitors are an important focus of therapeutic research for atopic dermatitis. Upadacitinib and abrocitinib are oral small molecules that inhibit the JAK/STAT pathway by selectively blocking JAK1. Data from phase II and III trials are encouraging, revealing that JAK1 inhibitors are effective and well-tolerated agents for moderate-to-severe atopic dermatitis. Selective JAK1 inhibitors may represent an important therapeutic option to be included in the treatment algorithm of atopic dermatitis, owing to oral administration and a favorable safety and tolerability profile. In this article, we review the current evidence on the efficacy and safety of oral selective JAK1 inhibitors for the treatment of atopic dermatitis.
Similar content being viewed by others
References
Deckers IAG, McLean S, Linssen S, et al. Investigating international time trends in the incidence and prevalence of atopic eczema 1990–2010: a systematic review of epidemiological studies. PLoS One. 2012;7:e39803.
Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Investig Dermatol. 2014;134:1527–34.
Ronnstad ATM, Halling-Overgaard AS, Hamann CR, et al. Association of atopic dermatitis with depression, anxiety, and suicidal ideation in children and adults: a systematic review and meta-analysis. J Am Acad Dermatol. 2018;79(3):448–56.e30.
Ferreira S, Torres T. Dupilumab for the treatment of atopic dermatitis. Actas Dermosifiliogr. 2018;109(3):230–40.
Guttman-Yassky E, Thaçi D, Pangan AL, et al. Upadacitinib in adults with moderate-to-severe atopic dermatitis: 16-week results from a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2020;145(3):877–84. https://doi.org/10.1016/j.jaci.2019.11.025.
Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of atopic eczema (atopic dermatitis) part 1. J Eur Acad Dermatol Venereol. 2012;26(8):1045–60.
Roekevisch E, Spuls PI, Kuester D, Limpens J, Schmitt J. Efficacy and safety of systemic treatments for moderate-to-severe atopic dermatitis: a systematic review. J Allergy Clin Immunol. 2014;133(2):429–38.
Baghoomian W, Na C, Simpson EL. New and emerging biologics for atopic dermatitis. Am J Clin Dermatol. 2020;21:457–65. https://doi.org/10.1007/s40257-020-00515-1.
Silverberg JI, Hanifin JM. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population-based study. J Allergy Clin Immunol. 2013;132:1132–8.
Simpson EL, Bieber T, Guttman-Yassky E, SOLO 1 and SOLO 2 Investigators, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375(24):2335–48.
Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet. 2017;389(10086):2287–303.
Thaçi D, Simpson EL, Beck LA, et al. Efficacy and safety of dupilumab in adults with moderate-to-severe atopic dermatitis (AD) inadequately controlled by topical treatments: a randomised, placebo-controlled, dose-ranging phase 2b trial. Lancet. 2016;387(10013):40–52.
He H, Guttman-Yassky E. JAK inhibitors for atopic dermatitis: an update. Am J Clin Dermatol. 2019;20(2):181–92.
Weidinger S, Beck LA, Bieber T, et al. Atopic dermatitis. Nat Rev Dis Primer. 2018;4:1.
Spergel JM. From atopic dermatitis to asthma: the atopic march. Ann Allergy Asthma Immunol. 2010;105(2):99–106.
Silverberg JI, Simpson EL. Association between severe eczema in children and multiple comorbid conditions and increased healthcare utilization. Pediatr Allergy Immunol. 2013;24(5):476–86.
Gittler JK, Shemer A, Suárez-Fariñas M, et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis. J Allergy Clin Immunol. 2012;130(6):1344–54.
Kou K, Aihara M, Matsunaga T, et al. Association of serum interleukin-18 and other biomarkers with disease severity in adults with atopic dermatitis. Arch Dermatol Res. 2012;304(4):305–12.
Kim BS, Wang K, Siracusa MC, et al. Basophils promote innate lymphoid cell responses in inflamed skin. J Immunol. 2014;193(7):3717–25.
Seltmann J, Roesner LM, von Hesler F-W, et al. IL-33 impacts on the skin barrier by downregulating the expression of filaggrin. J Allergy Clin Immunol. 2015;135:1659–1661.e4.
Cole C, Kroboth K, Schurch NJ, et al. Filaggrin-stratified transcriptomic analysis of pediatric skin identifies mechanistic pathways in patients with atopic dermatitis. J Allergy Clin Immunol. 2014;134:82–91.
Palmer CN, Irvine AD, Terron-Kwiatkowski A, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006;38(4):441–6.
Fallon PG, Sasaki T, Sandilands A, et al. A homozygous frameshift mutation in the mouse Flg gene facilitates enhanced percutaneous allergen priming. Nat Genet. 2009;41:602–8.
Czarnowicki T, Malajian D, Shemer A, et al. Skin-homing and systemic T-cell subsets show higher activation in atopic dermatitis versus psoriasis. J Allergy Clin Immunol. 2015;136:208–11.
Malajian D, Guttman-Yassky E. New pathogenic and therapeutic paradigms in atopic dermatitis. Cytokine. 2015;73(2):311–8.
Park HY, Kim CR, Huh IS, et al. Staphylococcus aureus colonization in acute and chronic skin lesions of patients with atopic dermatitis. Ann Dermatol. 2013;25(4):410–6.
Renert-Yuval Y, Guttman-Yassky E. What is new in atopic dermatitis. Dermatol Clin. 2019;37(2):205–13. https://doi.org/10.1016/j.det.2018.12.007.
Thepen T, Langeveld-Wildschut EG, Bihari IC, et al. Biphasic response against aeroallergen in atopic dermatitis showing a switch from an initial TH2 response to a TH1 response in situ: an immunocytochemical study. J Allergy Clin Immunol. 1996;97(3):828–37.
Suarez-Farinas M, Dhingra N, Gittler J, et al. Intrinsic atopic dermatitis shows similar TH2 and higher TH17 immune activation compared with extrinsic atopic dermatitis. J Allergy Clin Immunol. 2013;132(2):361–70.
Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study. J Am Acad Dermatol. 2019;80(4):913–921.e9. https://doi.org/10.1016/j.jaad.2018.01.018.
Wolk K, Witte E, Witte K, et al. Biology of interleukin-22. Semin Immunopathol. 2010;32:17–31.
Boniface K, Bernard FX, Garcia M, Gurney AL, Lecron JC, Morel F. IL-22 inhibits epidermal differentiation and induces proinflammatory gene expression and migration of human keratinocytes. J Immunol. 2005;174:3695–702.
Noda S, Suárez-Fariñas M, Ungar B, et al. The Asian atopic dermatitis phenotype combines features of atopic dermatitis and psoriasis with increased TH17 polarization. J Allergy Clin Immunol. 2015;136:1254–64.
Albanesi C, Fairchild HR, Madonna S, et al. IL-4 and IL-13 negatively regulate TNF-alpha and IFN-gamma-induced beta-defensin expression through STAT-6, suppressor of cytokine signaling (SOCS)-1, and SOCS-3. J Immunol. 2007;179:984–92.
Sehra S, Yao Y, Howell MD, et al. IL-4 regulates skin homeostasis and the predisposition toward allergic skin inflammation. J Immunol. 2010;184:3186–90.
Ong PY, Ohtake T, Brandt C, et al. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002;347:1151–60.
Brauweiler AM, Goleva E, Leung DYM. Th2 cytokines increase Staphylococcus aureus alpha toxin-induced keratinocyte death through the signal transducer and activator of transcription 6 (STAT6). J Investig Dermatol. 2014;134:2114–21.
Howell M, Wollenberg A, Garro R, et al. Cathelicidin deficiency predisposes to eczema herpeticum. J Allergy Clin Immunol. 2006;117:836–41.
van der Schaft J, Politiek K, van den Reek JMPA, et al. Drug survival for ciclosporin A in a long-term daily practice cohort of adult patients with atopic dermatitis. Br J Dermatol. 2015;172:1621–7.
Bao L, Zhang H, Chan LS. The involvement of the JAK-STAT signaling pathway in chronic inflammatory skin disease atopic dermatitis. JAKSTAT. 2013;2:e24137. https://doi.org/10.4161/jkst.24137.
Howell MD, Fitzsimons C, Smith PA. JAK/STAT inhibitors and other small molecule cytokine antagonists for the treatment of allergic disease. Ann Allergy Asthma Immunol. 2018;120:367–75. https://doi.org/10.1016/j.anai.2018.02.012.
O’Shea JJ, Holland SM, Staudt LM. JAKs and STATs in immunity, immunodeficiency, and cancer. N Engl J Med. 2013;368:161–70.
Pesu M, Laurence A, Kishore N, et al. Therapeutic targeting of Janus kinases. Immunol Rev. 2008;223:132–42.
Hirahara K, Schwartz D, Gadina M, et al. Targeting cytokine signaling in autoimmunity: back to the future and beyond. Curr Opin Immunol. 2016;43:89–97.
Alves de Medeiros AK, Speeckaert R, Desmet E, et al. JAK3 as an emerging target for topical treatment of inflammatory skin diseases. PLoS One. 2016;11:e0164080.
Shreberk-Hassidim R, Ramot Y, Zlotogorski A. Janus kinase inhibitors in dermatology: a systematic review. J Am Acad Dermatol. 2017;76(745–53):e19.
Damsky W, King BA. JAK inhibitors in dermatology: the promise of a new drug class. J Am Acad Dermatol. 2017;76:736–44.
Hald A, Andrés RM, Salskov-Iversen ML, et al. STAT1 expression and activation is increased in lesional psoriatic skin. Br J Dermatol. 2013;168:302–10.
Oetjen LK, Mack MR, Feng J, et al. Sensory neurons co-opt classical immune signaling pathways to mediate chronic itch. Cell. 2017;171(217–28):e13.
Villarino AV, Kanno Y, O’Shea JJ. Mechanisms and consequences of Jak-STAT signaling in the immune system. Nat Immunol. 2017;18:374–84.
Ghoreschi K, Gadina M. Jakpot! New small molecules in autoimmune and inflammatory diseases. Exp Dermatol. 2014;23(1):7–11.
Ghoreschi K, Laurence A, O’Shea JJ. Janus kinases in immune cell signaling. Immunol Rev. 2009;228(1):273–87.
O’Shea JJ, Schwartz DM, Villarino AV, Gadina M, McInnes IB, Laurence A. The JAK-STAT pathway: impact on human disease and therapeutic intervention. Annu Rev Med. 2015;66:311–28.
Murray PJ. The JAK-STAT signaling pathway: input and output integration. J Immunol. 2007;178(5):2623–9.
Schindler C, Levy DE, Decker T. JAK-STAT signaling: from interferons to cytokines. J Biol Chem. 2007;282(28):20059–63.
Brandt EB, Sivaprasad E. Th2 cytokines and atopic dermatitis. J Clin Cell Immunol. 2011;2(3):110. https://doi.org/10.4172/2155-9899.1000110.
O’Shea JJ, Kontzias A, Yamaoka K, et al. Janus kinase inhibitors in autoimmune diseases. Ann Rheum Dis. 2013;72:ii111–5.
Furue K, et al. The IL-13-OVOL1-FLG axis in atopic dermatitis. Immunology. 2019;158(4):281–6. https://doi.org/10.1111/imm.13120.
Silverberg JI, Kantor R. The role of interleukins 4 and/or 13 in the pathophysiology and treatment of atopic dermatitis. Dermatol Clin. 2017;35(3):327–34.
Lou H, Lu J, Choi EB, et al. Expression of IL-22 in the skin causes Th2-biased immunity, epidermal barrier dysfunction, and pruritus via stimulating epithelial Th2 cytokines and the GRP pathway. J Immunol. 2017;198:2543–55. https://doi.org/10.4049/jimmunol.1600126.
Guttman-Yassky E, Brunner PM, Neumann AU, et al. Efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in adults with moderate-to-severe atopic dermatitis inadequately controlled by conventional treatments: a randomized, double-blind, phase 2a trial. J Am Acad Dermatol. 2018;78(872–81):e876.
Smolen J, Pangan AL, Emery P, et al. A phase 3 randomised, placebo-controlled, double-blind study of upadacitinib as monotherapy in patients with active rheumatoid arthritis and inadequate response to methotrexate (SELECT- MONOTHERAPY): a randomized, placebo-controlled, double-blind phase 3 study. Lancet. 2019;393(10188):2303–11. https://doi.org/10.1016/S0140-6736(19)30419-2.
Genovese MC, Fleischmann R, Combe B, et al. Safety and efficacy of upadacitinib in patients with active rheumatoid arthritis refractory to biologic disease-modifying anti-rheumatic drugs (SELECT-BEYOND): a double-blind, randomised controlled phase 3 trial. Lancet. 2018;391(10139):2513–24.
Sandborn W, Ghosh S, Panes J, et al. Efficacy and safety of upadacitinib as an induction therapy for patients with moderately-to-severely active ulcerative colitis: data from the phase 2b study u-achieve [OP 195]. United European Gastroenterology Week, Vienna, 20–24 October 2018.
AbbVie, A study of the efficacy and safety of upadacitinib (ABT-494) in subjects with moderately to severely active Crohn’s disease who have inadequately responded to or are intolerant to conventional therapies but have not failed biologic therapy [ClinicalTrials.gov identifier NCT03345849]. https://clinicaltrials.gov/ct2/show/NCT03345849?term=NCT03345849&draw=2&rank=1. Accessed 31 July 2020
Guttman-Yassky E, Silverberg JI, Thaci D, et al. Primary results from a phase 2b, randomized, placebo-controlled trial of upadacitinib for patients with atopic dermatitis [abstract no. 6533]. American Academy of Dermatology Annual Meeting, San Diego (CA), 16–20 February 2018.
Voss J, Graff C, Schwartz A, et al. Pharmacodynamics of a novel Jak1 selective inhibitor in rat arthritis and anemia models and in healthy human subjects. Arthritis Rheumatol. 2013;65(10):S1015.
Winthrop KL. The emerging safety profile of JAK inhibitors in rheumatic disease. Nat Rev Rheumatol. 2017;13(4):234–43.
Parmentier JM, Voss J, Graff C, et al. In vitro and in vivo characterization of the JAK1 selectivity of upadacitinib (ABT-494). BMC Rheumatol. 2018;2:23.
Klunder B, Mittapalli RK, Mohamed MF, Friedel A, Noertersheuser P, Othman AA. Population pharmacokinetics of upadacitinib using the immediate-release and extended-release formulations in healthy subjects and subjects with rheumatoid arthritis: analyses of phase I–III clinical trials. Clin Pharmacokinet. 2019;58(8):1045–58.
Klunder B, Mohamed MF, Othman AA. Population pharmacokinetics of upadacitinib in healthy subjects and subjects with rheumatoid arthritis: analyses of phase I and II clinical trials. Clin Pharmacokinet. 2018;57:977–88.
Mohamed MF, Camp HS, Jiang P, Padley RJ, Asatryan A, Othman AA. Pharmacokinetics, safety and tolerability of ABT-494, a novel selective JAK 1 inhibitor, in healthy volunteers and subjects with rheumatoid arthritis. Clin Pharmacokinet. 2016;55(12):1547–58.
AbbVie Inc. Chicago (IL): AbbVie Inc.; 2018. AbbVie’s upadacitinib granted breakthrough therapy designation from the U.S. Food and Drug Administration for atopic dermatitis; 2018 [cited 2018 October 21]. https://news.abbvie.com/news/abbvies-upadacitinib-granted-breakthrough-therapydesignation-from-us-food-and-drug-administration-for-atopic-dermatitis.htm. Accessed 31 July 2020.
Guttman-Yassky E, Thaçi D, Pangan AL, Hong HC, KA Papp, Reich K, et al. Upadacitinib in adults with moderate to severe atopic dermatitis: 16-week results from a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2019. https://doi.org/10.1016/j.jaci.2019.11.025(Epub ahead of print).
AbbVie. Evaluation of upadacitinib in adolescent and adult patients with moderate to severe atopic dermatitis (eczema) (Measure Up 1). [ClinicalTrials.gov. Identifier: NCT03569293]. https://clinicaltrials.gov/ct2/show/NCT03569293?term=NCT03569293&draw=2&rank=1. Accessed 31 July 2020
Kettle JG, Åstrand A, Catley M, et al. Inhibitors of JAK-family kinases: an update on the patent literature 2013–2015, part 2. Expert Opin Ther Pat. 2017;27(2):145–61.
Peeva E, Hodge MR, Kieras E, et al. Evaluation of a Janus kinase 1 inhibitor, PF-04965842, in healthy subjects: a phase 1, randomized, placebo-controlled, dose escalation study. Br J Clin Pharmacol. 2018;84(8):1776–88. https://doi.org/10.1111/bcp.13612.
Gooderham MJ, Forman SB, Bissonnette R, Beebe JS, Zhang W, Banfield C, et al. Efficacy and safety of oral Janus kinase 1 inhibitor abrocitinib for patients with atopic dermatitis: a phase 2 randomized clinical trial. JAMA Dermatol. 2019;155(12):1371–9. https://doi.org/10.1001/jamadermatol.2019.2855.
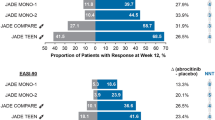
Simpson E, Sinclair R, Forman S, et al. Efficacy and safety of abrocitinib in patients with moderate-to-severe atopic dermatitis: results from the phase 3, JADE MONO-1 study. In: Oral presentation at the 28th Congress of the European Academy of Dermatology and Venereology (EADV), Madrid, 9–13 October 2019.
Silverberg JI, Simpson EL, Thyssen JP, Gooderham M, Chan G, Feeney C, et al. Efficacy and safety of abrocitinib in patients with moderate-to-severe atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2020;3:e201406. https://doi.org/10.1001/jamadermatol.2020.1406(Epub ahead of print).
Pfizer. Study evaluating efficacy and safety of PF-04965842 and dupilumab in adult subjects with moderate to severe atopic dermatitis on background topical therapy (JADE Compare) [ClinicalTrials.gov identifier NCT03720470]. https://clinicaltrials.gov/ct2/show/NCT03720470?term=JADE+COMPARE&draw=2&rank=1. Accessed 31 July 2020
Brunner PM, Guttman-Yassky E, Leung DY. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol. 2017;139:S65–76.
Papp KA, Menter MA, Raman M, et al. A randomized phase 2b trial of baricitinib, an oral Janus kinase (JAK) 1/JAK2 inhibitor, in patients with moderate-to-severe psoriasis. Br J Dermatol. 2016;174(6):1266–76.
Genovese MC, Smolen JS, Weinblatt ME, et al. Efficacy and safety of ABT-494, a selective JAK-1 inhibitor, in a phase IIb study in patients with rheumatoid arthritis and an inadequate response to methotrexate. Arthritis Rheumatol. 2016;68(12):2857–66.
Schmieder GJ, Draelos ZD, Pariser DM, et al. Efficacy and safety of the Janus kinase 1 inhibitor PF-04965842 in patients with moderate-to-severe psoriasis: phase II, randomized, double-blind, placebo-controlled study. Br J Dermatol. 2017;179(1):54–62.
van Vollenhoven RF, Fleischmann R, Cohen S, et al. Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. N Engl J Med. 2012;367(6):508–19.
Sandborn WJ, Ghosh S, Panes J, et al. Tofacitinib, an oral Janus kinase inhibitor, in active ulcerative colitis. N Engl J Med. 2012;367(7):616–24.
Verden A, Dimbil M, Kyle R, Overstreet B, Hoffman KB. Analysis of spontaneous postmarket case reports submitted to the FDA regarding thromboembolic adverse events and JAK inhibitors. Drug Saf. 2018;41(4):357–61. https://doi.org/10.1007/s40264-017-0622-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding has been received for the preparation of this article.
Conflicts of Interest
Sandra Ferreira has no conflicts of interest that are directly relevant to the content of this article. Emma Guttman declares the following conflicts of interest: AbbVie, Almirall, Amgen, AnaptysBio, Asana Biosciences, Boehringer-Ingelheim, Cara Therapeutics, Celgene, Concert, DBV, Dermira, Dermavant, DS Biopharma, Eli Lilly, EMD Serono, Escalier, Galderma, Glenmark, Innovaderm, Janssen Pharmaceuticals, Kiniksa, Kyowa Kirin, LEO Pharma, Mitsubishi Tanabe, Novan, Pfizer, Ralexar, RAPT Therapeutics, Regeneron, Sanofi, Sienna Biopharma, UCB, and Union Therapeutics. Tiago Torres declares the following conflicts of interest: AbbVie, Amgen, Almirall, Arena Pharmaceuticals, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Janssen, Biocad, LEO Pharma, Eli Lilly, MSD, Novartis, Pfizer, Samsung-Bioepis, Sanofi-Genzyme, and Sandoz.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable
Availability of data and material
Not applicable.
Code Availability
Not applicable.
Authors’ Contributions
Sandra Ferreira, Emma Guttamn, and Tiago Torres had the idea for the article, performed the literature search and data analysis, and drafted and critically revised the work.
Rights and permissions
About this article
Cite this article
Ferreira, S., Guttman-Yassky, E. & Torres, T. Selective JAK1 Inhibitors for the Treatment of Atopic Dermatitis: Focus on Upadacitinib and Abrocitinib. Am J Clin Dermatol 21, 783–798 (2020). https://doi.org/10.1007/s40257-020-00548-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-020-00548-6