Abstract
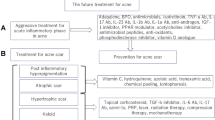
There is a high unmet clinical need for new and better treatments in acne vulgaris. Propionibacterium acnes has a strong proinflammatory activity and targets molecules involved in the innate cutaneous immunity, keratinocytes and sebaceous glands of the pilosebaceous follicle. The role of P. acnes in acne confers legitimacy on the possible benefits of immunization-based approaches, which may represent a solution for limiting the development of antibiotic-resistant P. acnes. Various immunization-based approaches have been developed over the last decades, including killed pathogen-based vaccines, vaccination against cell wall-anchored sialidase, monoclonal antibodies to the Christie, Atkins, Munch-Peterson factor of P. acnes, anti-Toll-like receptors vaccines and natural antimicrobial peptides. This review summarizes the current evidence and explores the challenges to making this a realistic treatment option for the future.

Similar content being viewed by others
References
Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379(9813):361–72.
Ghodsi SZ, Orawa H, Zouboulis CC. Prevalence, severity, and severity risk factors of acne in high school pupils: a community-based study. J Invest Dermatol. 2009;129(9):2136–41.
Dréno B. Recent data on epidemiology of acne [in French]. Ann Dermatol Venereol. 2010;137(Suppl. 2):S49–51.
Gonçalves G, Amado J, Matos M, et al. The prevalence of acne among a group of Portuguese medical students. J Eur Acad Dermatol Venereol. 2012;26(4):514–7.
Perkins AC, Maglione J, Hillebrand GG, et al. Acne vulgaris in women: prevalence across the life span. J Womens Health (Larchmt). 2012;21(2):223–30.
Golchai J, Khani SH, Heidarzadeh A, et al. Comparison of anxiety and depression in patients with acne vulgaris and healthy individuals. Indian J Dermatol. 2010;55(4):352–4.
Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, selfesteem, mood, and psychological disorders. Dermatol Online J. 2011;17(1):1.
Simonart T. Newer approaches to the treatment of acne vulgaris. Am J Clin Dermatol. 2012;13(6):357–64.
Kurokawa I, Danby FW, Ju Q, Wang X, Xiang LF, Xia L, Chen W, Nagy I, Picardo M, Suh DH, Ganceviciene R, Schagen S, Tsatsou F, Zouboulis CC. New developments in our understanding of acne pathogenesis and treatment. Exp Dermatol. 2009;18(10):821–32.
Kim J. Acne vaccines: therapeutic option for the treatment of acne vulgaris? J Invest Dermatol. 2008;128:2353–4.
Rott H. Thrombotic risks of oral contraceptives. Curr Opin Obstet Gynecol. 2012;24(4):235–40.
Leyden JJ, McGinley KJ, Mills OH, Kligman AM. Propionibacterium levels in patients with and without acne vulgaris. J Invest Dermatol. 1975;65(4):382–4.
Ross JI, Snelling AM, Carnegie E, Coates P, Cunliffe WJ, Bettoli V, Tosti G, Katsambas A, Galvan Peréz Del Pulgar JI, Rollman O, Török L, Eady EA, Cove JH. Antibiotic-resistant acne: lessons from Europe. Br J Dermatol. 2003;148(3):467–78.
Simonart T, Dramaix M. Treatment of acne with topical antibiotics: lessons from clinical studies. Br J Dermatol. 2005;153(2):395–403.
Simonart T, Dramaix M, De Maertelaer V. Efficacy of tetracyclines in the treatment of acne vulgaris: a review. Br J Dermatol. 2008;158(2):208–16.
Bruggemann H, Henne A, Hoster F, et al. The complete genome sequence of Propionibacterium acnes, a commensal of human skin. Science. 2004;305:671–3.
Sato T, Kurihara H, Akimoto N, Noguchi N, Sasatsu M, Ito A. Augmentation of gene expression and production of promatrix metalloproteinase 2 by Propionibacterium acnes-derived factors in hamster sebocytes and dermal fibroblasts: a possible mechanism for acne scarring. Biol Pharm Bull. 2011;34(2):295–9.
McDowell A, Valanne S, Ramage G, et al. Propionibacterium acnes types I and II represent phylogenetically distinct groups. J Clin Microbiol. 2005;43(1):326–34.
Lomholt HB, Kilian M. Population genetic analysis of Propionibacterium acnes identifies a subpopulation and epidemic clones associated with acne. PLoS One. 2010;5(8):e12277.
Kwon HH, Yoon JY, Park SY, Suh DH. Analysis of distribution patterns of Propionibacterium acnes phylotypes and Peptostreptococcus species from acne lesions. Br J Dermatol. 2013 Jun 25 (Epub ahead of print).
Beylot C, Auffret N, Poli F, Claudel JP, Leccia MT, Del Giudice P, Dreno B. Propionibacterium acnes: an update on its role in the pathogenesis of acne. J Eur Acad Dermatol Venereol. 2013 Aug 1 (Epub ahead of print).
Kim J, Ochoa MT, Krutzik SR, et al. Activation of toll-like receptor 2 in acne triggers inflammatory cytokine responses. J Immunol. 2002;169(3):1535–41.
Sugisaki H, Yamanaka K, Kakeda M, et al. Increased interferon-gamma, interleukin-12p40 and IL-8 production in Propionibacterium acnes-treated peripheral blood mononuclear cells from patient with acne vulgaris: host response but not bacterial species is the determinant factor of the disease. J Dermatol Sci. 2009;55(1):47–52.
Nakatsuji T, Liu Y-T, Huang C-P, Gallo RL, Huang C-M. Vaccination targeting a surface sialidase of P. acnes: implication for new treatment of acne vulgaris. PLoS One. 2008;3:e1551.
Dispenza MC, Wolpert EB, Gilliland KL, Dai JP, Cong Z, Nelson AM, Thiboutot DM. Systemic isotretinoin therapy normalizes exaggerated TLR-2-mediated innate immune responses in acne patients. J Invest Dermatol. 2012;132(9):2198–205.
Chronnell CM, Ghali LR, Ali RS, Quinn AG, Holland DB, Bull JJ, Cunliffe WJ, McKay IA, Philpott MP, Müller-Röver S. Human beta defensin-1 and -2 expression in human pilosebaceous units: upregulation in acne vulgaris lesions. J Invest Dermatol. 2001;117(5):1120–5.
Nagy I, Pivarcsi A, Kis K, Koreck A, Bodai L, McDowell A, et al. Propionibacterium acnes and lipopolysaccharide induce the expression of antimicrobial peptides and proinflammatory cytokines/chemokines in human sebocytes. Microbes Infect. 2006;8:2195–205.
Harder J, Tsuruta D, Murakami M, Kurokawa I. What is the role of antimicrobial peptides (AMP) in acne vulgaris? Exp Dermatol. 2013;22(6):386–91.
Jarrousse V, Castex-Rizzi N, Khammari A, Charveron M, Dréno B. Modulation of integrins and filaggrin expression by Propionibacterium acnes extracts on keratinocytes. Arch Dermatol Res. 2007;299(9):441–7.
Isard O, Knol AC, Ariès MF, Nguyen JM, Khammari A, Castex-Rizzi N, Dréno B. Propionibacterium acnes activates the IGF-1/IGF-1R system in the epidermis and induces keratinocyte proliferation. J Invest Dermatol. 2011;131(1):59–66.
Iinuma K, Sato T, Akimoto N, Noguchi N, Sasatsu M, Nishijima S, Kurokawa I, Ito A. Involvement of Propionibacterium acnes in the augmentation of lipogenesis in hamster sebaceous glands in vivo and in vitro. J Invest Dermatol. 2009;129(9):2113–9.
Saint-Leger D, Bague A, Cohen E, Chivot M. A possible role for squalene in the pathogenesis of acne I. In vitro study of squalene oxidation. Br J Dermatol. 1986;114:535–42.
Nakatsuji T, Kao MC, Zhang L, Zouboulis CC, Gallo RL, Huang CM. Sebum free fatty acids enhance the innate immune defense of human sebocytes by upregulating beta-defensin-2 expression. J Invest Dermatol. 2010;130(4):985–94.
Jahns AC, Lundskog B, Ganceviciene R, Palmer RH, Golovleva I, Zouboulis CC, McDowell A, Patrick S, Alexeyev OA. An increased incidence of Propionibacterium acnes biofilms in acne vulgaris: a case-control study. Br J Dermatol. 2012;167(1):50–8.
Shaheen B, Gonzalez M. Acne sans P. acnes. J Eur Acad Dermatol Venereol. 2013;27(1):1–10.
McGinley KJ, Webster GF, Leyden JJ. Regional variations of cutaneous propionibacteria. Appl Environ Microbiol. 1978;35:62–6.
Leyden JJ, McGinley KJ, Vowels B. Propionibacterium acnes colonization in acne and non-acne. Dematology. 1988;196:55–8.
Kuwahara K, Kitazawa T, Kitagaki H, Tsukamoto T, Kikuchi M. Nadifloxacin, an antiacne quinolone antimicrobial, inhibits the production of proinflammatory cytokines by human peripheral blood mononuclear cells and normal human keratinocytes. J Dermatol Sci. 2005;38(1):47–55.
Murata K, Sugita K, Kobayashi M, Kabashima K, Tokura Y. Nadifloxacin downmodulates antigen-presenting functions of epidermal Langerhans cells and keratinocytes. J Dermatol Sci. 2006;42(2):91–9.
Ingham E, Gowland G, Ward RM, Holland KT, Cunliffe WJ. Antibodies to P. acnes and P. acnes exocellular enzymes in the normal population at various ages and in patients with acne vulgaris. Br J Dermatol. 1987;116:805–12.
Nakatsuji T, Rasochova L, Huang CM. Vaccine therapy for P. acnes-associated diseases. Infect Disord Drug Targets. 2008;8(3):160–5.
Webster GF, Indrisano JP, Leyden JJ. Antibody titers to Propionibacterium acnes cell wall carbohydrate in nodulocystic acne patients. J Invest Dermatol. 1985;84:496–500.
Ashbee HR, Muir SR, Cunliffe WJ, Ingham E. IgG subclasses specific to Staphylococcus epidermidis and Propionibacterium acnes in patients with acne vulgaris. Br J Dermatol. 1997;136:730–3.
Holland K, Cunliffe WJ, Roberts C. Acne vulgaris: an investigation into the number of anaerobic diphtheroids and members of the Micrococcaceae in normal and acne skin. Br J Dermatol. 1977;96:623–6.
Knop J, Ollefs K, Frosch PJ. Anti-P. acnes antibody in comedonal extracts. J Invest Dermatol. 1983;80(1):9–12.
Vymola F, Buda J, Lochmann O, Pillich J. Successful treatment of acne by immunotherapy. J Hyg Epidemiol Microbiol Immunol. 1970;14:135–8.
Goldman L, Michael JG, Riebel S. The immunobiology of acne. A polyvalent propionibacteria vaccine. Cutis. 1979;23:181–4.
Rubisz-Brzezińska J, Wilk-Czyz R, Brzezińska-Wcisło L, Kasprowicz A. Clinical evaluation of serious forms of acne treated with autovaccine. Med Dosw Mikrobiol. 1994;46(1–2 Suppl):35–42 (in Polish).
Zaluga E. Skin reactions to antigens of Propionibacterium acnes in patients with acne vulgaris treated with autovaccine. Ann Acad Med Stetin. 1998;44:65–85 (in Polish).
Hayashi N, Watanabe H, Yasukawa H, Uratsuji H, Kanazawa H, Ishimaru M, Kotera N, Akatsuka M, Kawashima M. Comedolytic effect of topically applied active vitamin D3 analogue on pseudocomedones in the rhino mouse. Br J Dermatol. 2006;155(5):895–901.
Nakatsuji T, Liu Y-T, Huang C-P, Gallo RL, Huang C-M. Antibodies elicited by inactivated P. acnes–based vaccines exert protective immunity and attenuate the IL-8 production in human sebocytes: relevance to therapy for acne vulgaris. J Invest Dermatol. 2008;128:2451–7.
Liu PF, Nakatsuji T, Zhu W, Gallo RL, Huang CM. Passive immunoprotection targeting a secreted CAMP factor of Propionibacterium acnes as a novel immunotherapeutic for acne vulgaris. Vaccine. 2011;29(17):3230–8.
Rasko DA, Moreira CG, de Li R, Reading NC, Ritchie JM, Waldor MK, et al. Targeting QseC signaling and virulence for antibiotic development. Science. 2008;321(5892):1078–80.
Nakatsuji T, Tang DC, Zhang L, Gallo RL, Huang CM. Propionibacterium acnes CAMP factor and host acid sphingomyelinase contribute to bacterial virulence: potential targets for inflammatory acne treatment. PLoS One. 2011;6(4):e14797.
Nagy I, Pivarcsi A, Koreck A, Széll M, Urbán E, Kemény L. Distinct strains of Propionibacterium acnes induce selective human beta-defensin-2 and interleukin-8 expression in human keratinocytes through toll-like receptors. J Invest Dermatol. 2005;124(5):931–8.
Rubinchik E, Dugourd D, Algara T, et al. Antimicrobial and antifungal activities of a novel cationic antimicrobial peptide, omiganan, in experimental skin colonisation models. Int J Antimicrob Agents. 2009;34(5):457–61.
Wang Y, Zhang Z, Chen L, et al. Cathelicidin-BF, a snake cathelicidin-derived antimicrobial peptide, could be an excellent therapeutic agent for acne vulgaris. PLoS One. 2011;6(7):e22120.
Grice EA, Segre JA. The skin microbiome. Nat Rev Microbiol. 2011;9:244–53.
Kitagawa H, Yamanaka K, Kakeda M, Inada H, Imai Y, Gabazza EC, Kurokawa I, Mizutani H. Propionibacterium acnes vaccination induces regulatory T cells and Th1 immune responses and improves mouse atopic dermatitis. Exp Dermatol. 2011;20(2):157–8.
Acknowledgment
No sources of funding were used to prepare this review.
Conflicts of interest
The author has no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simonart, T. Immunotherapy for Acne Vulgaris: Current Status and Future Directions. Am J Clin Dermatol 14, 429–435 (2013). https://doi.org/10.1007/s40257-013-0042-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-013-0042-8