Abstract
Introduction
Diabetes and coronary artery disease are two common conditions that often co-exist. In recent years, sodium-glucose cotransporter 2 inhibitors (SGLT2i) have been demonstrated to provide significant cardioprotective benefits, especially among patients with heart failure.
Objective
In this systematic review, we look to identify the outcomes SGLT2i use in patients undergoing coronary revascularization.
Methods
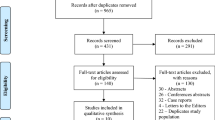
Pubmed and Embase were systematically searched for articles describing the outcomes of patients taking SGLT2i and undergoing coronary revascularization. 834 titles and abstracts were screened, 42 full texts were reviewed, and 18 studies were found to meet the inclusion criteria and were included in this review.
Results
For patients undergoing coronary artery bypass grafting and percutaneous coronary intervention, the use of SGLT2i resulted in reductions in mortality, hospitalization for heart failure, and improved blood glucose; however, these benefits were not consistently reported in the literature. Reduced inflammatory markers and positive cardiac remodeling were identified among patients taking SGLT2i.
Conclusions
Sodium-glucose cotransporter 2 inhibitors (SGLT2i) have been demonstrated to provide benefits for patients with heart failure along with a host of positive modulatory effects on the cardiovascular system, including reductions in inflammatory properties, hypertension, and left ventricular volume load. Given the clear benefit provided by SGLT2i to patients with cardiovascular disease and a host of positive properties that are expected to be protective for patients with ischemic heart disease, future investigation into the relationship between SGLT2i and outcomes for patients undergoing revascularization is imperative.

Similar content being viewed by others
References
Htay T, Soe K, Lopez-Perez A, Doan AH, Romagosa MA, Aung K. Mortality and cardiovascular disease in type 1 and type 2 diabetes. Curr Cardiol Rep. 2019;21:1–7.
Navaratnarajah M, Rea R, Evans R, Gibson F, Antoniades C, Keiralla A, et al. Effect of glycaemic control on complications following cardiac surgery: literature review. J Cardiothorac Surg. 2018;13:10.
Halkos ME, Puskas JD, Lattouf OM, Kilgo P, Kerendi F, Song HK, et al. Elevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2008;136:631–40.
Henning RJ. Type-2 diabetes mellitus and cardiovascular disease. Future Cardiol. 2018;14:491–509.
Rieg T, Vallon V. Development of SGLT1 and SGLT2 inhibitors. Diabetologia. 2018;61:2079–86.
Stone JA, Houlden RL, Lin P, Udell JA, Verma S. Cardiovascular protection in people with diabetes. Can J Diabetes. 2018;42:S162–9.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
O’Meara E, McDonald M, Chan M, Ducharme A, Ezekowitz JA, Giannetti N, et al. CCS/CHFS heart failure guidelines: clinical trial update on functional mitral regurgitation, SGLT2 Inhibitors, ARNI in HFpEF, and Tafamidis in Amyloidosis. Can J Cardiol. 2020;36:159–69.
Thourani VH, Weintraub WS, Stein B, Gebhart SSP, Craver JM, Jones EL, et al. Influence of diabetes mellitus on early and late outcome after coronary artery bypass grafting. Ann Thorac Surg. 1999;67:1045.
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol. 2002;40:418–23.
Woods SE, Smith JM, Sohail S, Sarah A, Engle A. The influence of type 2 diabetes mellitus in patients undergoing coronary artery bypass graft surgery: an 8-year prospective cohort study. Chest. 2004;126:1789–95.
Cardona S, Pasquel FJ, Fayfman M, Peng L, Jacobs S, Vellanki P, et al. Hospitalization costs and clinical outcomes in CABG patients treated with intensive insulin therapy. J Diabetes Complications. 2017;31:742–7.
ADVANCE Collaborative Group; Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Eng J Med 2008;358:2560–72.
Skyler JS, Bergenstal R, Bonow RO, Buse J, Deedwania P, Gale EAM, et al. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA Diabetes Trials. Diabetes Care. 2009;32:187–92.
Turnbull FM, Abraira C, Anderson RJ, Byington RP, Chalmers JP, Duckworth WC, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009;52:2288–98.
Liosis S, Hochadel M, Darius H, Behrens S, Mudra H, Lauer B, et al. Effect of renal insufficiency and diabetes mellitus on in-hospital mortality after acute coronary syndromes treated with primary PCI. Results from the ALKK PCI Registry. Int J Cardiol. 2019;292:43–9.
Karayiannides S, Norhammar A, Frøbert O, James SK, Lagerqvist B, Lundman P. Prognosis in patients with diabetes mellitus and STEMI undergoing primary PCI. J Am Coll Cardiol. 2018;72:1427–8.
Cannon CP, Perkovic V, Agarwal R, Baldassarre J, Bakris G, Charytan DM, et al. Evaluating the effects of canagliflozin on cardiovascular and renal events in patients with type 2 diabetes mellitus and chronic kidney disease according to baseline HbA1c, Including Those With HbA1c <7%: Results From the CREDENCE Trial. Circulation. 2020;141:407–10.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Eng J Med. 2020;383:1413–24.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Eng J Med. 2021;385:1451–61.
Ferrannini E, Mark M, Mayoux E. CV Protection in the EMPA-REG OUTCOME Trial: A “Thrifty Substrate” Hypothesis. Diabetes Care. 2016;39:1108–14.
Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A, et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME® trial. Eur Heart J. 2016;37:1526–34.
Verma S, Mazer CD, Fitchett D, Inzucchi SE, Pfarr E, George JT, et al. Empagliflozin reduces cardiovascular events, mortality and renal events in participants with type 2 diabetes after coronary artery bypass graft surgery: subanalysis of the EMPA-REG OUTCOME® randomised trial. Diabetologia. 2018;61:1712–23.
Perkovic V, de Zeeuw D, Mahaffey KW, Fulcher G, Erondu N, Shaw W, et al. Canagliflozin and renal outcomes in type 2 diabetes: results from the CANVAS Program randomised clinical trials. Lancet Diabetes Endocrinol. 2018;6:691–704.
Solomon SD, McMurray JJV, Claggett B, de Boer RA, DeMets D, Hernandez AF, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Eng J Med. 2022;387:1089–98.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Eng J Med. 2017;377:644–57.
Olsen MB, Gregersen I, Sandanger Ø, Yang K, Sokolova M, Halvorsen BE, et al. Targeting the inflammasome in cardiovascular disease. JACC Basic Transl Sci. 2022;7:84–98.
Paolisso P, Foà A, Bergamaschi L, Donati F, Fabrizio M, Chiti C, et al. Hyperglycemia, inflammatory response and infarct size in obstructive acute myocardial infarction and MINOCA. Cardiovasc Diabetol. 2021;20(1):33.
Paolisso P, Bergamaschi L, Santulli G, Gallinoro E, Cesaro A, Gragnano F, et al. Infarct size, inflammatory burden, and admission hyperglycemia in diabetic patients with acute myocardial infarction treated with SGLT2-inhibitors: a multicenter international registry. Cardiovasc Diabetol. 2022;21:1–12.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535–b2535.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700–b2700.
Sardu C, Massetti M, Testa N, di Martino L, Castellano G, Turriziani F, et al. Effects of Sodium-Glucose Transporter 2 Inhibitors (SGLT2-I) in Patients With Ischemic Heart Disease (IHD) Treated by Coronary Artery Bypass Grafting via MiECC: Inflammatory Burden, and Clinical Outcomes at 5 Years of Follow-Up. Front Pharmacol. 2021;12:1–10.
Lee SJ, Lee KH, Oh HG, Seo HJ, Jeong SJ, Kim CH. Effect of sodium-glucose cotransporter-2 inhibitors versus dipeptidyl peptidase 4 inhibitors on cardiovascular function in patients with type 2 diabetes mellitus and coronary artery disease. J Obes Metab Syndr. 2019;28:254–61.
Lee H-F, Chan Y-H, Chuang C, Li P-R, Yeh Y-H, Hsiao F-C, et al. Cardiovascular, renal, and lower limb outcomes in patients with type 2 diabetes after percutaneous coronary intervention and treated with sodium–glucose cotransporter 2 inhibitors vs. dipeptidyl peptidase-4 inhibitors. Eur Heart J Cardiovasc Pharmacother. 2023;9:301–10.
Paolisso P, Bergamaschi L, Gragnano F, Gallinoro E, Cesaro A, Sardu C, et al. Outcomes in diabetic patients treated with SGLT2-Inhibitors with acute myocardial infarction undergoing PCI: the SGLT2-I AMI PROTECT Registry. Pharmacol Res. 2023;187: 106597.
Lin Y, Zhou F, Wang X, Guo Y, Chen W. Effect of dapagliflozin on clinical outcome after drug-eluting stent implantation in elderly T2DM patients: a real-world study. Comput Math Methods Med. 2023;2023:1–5.
Marfella R, Sardu C, D’Onofrio N, Fumagalli C, Scisciola L, Sasso FC, et al. SGLT-2 inhibitors and in-stent restenosis-related events after acute myocardial infarction: an observational study in patients with type 2 diabetes. BMC Med. 2023;21(1):71.
Adel SMH, Jorfi F, Mombeini H, Rashidi H, Fazeli S. Effect of a low dose of empagliflozin on short-term outcomes in type 2 diabetics with acute coronary syndrome after percutaneous coronary intervention. Saudi Med J. 2022;43:458–64.
Feitosa MPM, Lima EG, Abizaid AAC, Mehran R, Lopes NHM, de Assis Fischer Ramos T, et al. The safety of SGLT-2 inhibitors in diabetic patients submitted to elective percutaneous coronary intervention regarding kidney function: SAFE-PCI pilot study. Diabetol Metab Syndr. 2023;15:138.
Hua R, Ding N, Guo H, Wu Y, Yuan Z, Li T. Contrast-induced acute kidney injury in patients on SGLT2 inhibitors undergoing percutaneous coronary interventions: a propensity-matched analysis. Front Cardiovasc Med. 2022;9:1–9.
Khorlampenko AA, Karetnikova VN, Kochergina AM, Ignatova JS, Dyleva JA, Gruzdeva OL. Effect of empagliflosin on renal filtration in patients with coronary heart disease undergoing percutaneous coronary intervention [in Russian]. Kardiologiya. 2020;60:63–8.
von Lewinski D, Kolesnik E, Tripolt NJ, Pferschy PN, Benedikt M, Wallner M, et al. Empagliflozin in acute myocardial infarction: the EMMY trial. Eur Heart J. 2022;43:4421–32.
Zhu Y, Zhang J, Yan X, Sun L, Ji Y, Wang F. Effect of dapagliflozin on the prognosis of patients with acute myocardial infarction undergoing percutaneous coronary intervention. Cardiovasc Diabetol. 2022;21:1–10.
Hashikata T, Ikutomi M, Jimba T, Shindo A, Kakuda N, Katsushika S, et al. Empagliflozin attenuates neointimal hyperplasia after drug-eluting-stent implantation in patients with type 2 diabetes. Heart Vessels. 2020;35:1378–89.
Dayem KA, Younis O, Zarif B, Attia S, AbdelSalam A. Impact of dapagliflozin on cardiac function following anterior myocardial infarction in non-diabetic patients—DACAMI (a randomized controlled clinical trial). Int J Cardiol. 2023;379:9–14.
Sourij C, Aziz F, Tripolt NJ, Siller-Matula J, Pferschy PN, Kolesnik E, et al. Effects of empagliflozin in women and men with acute myocardial infarction—an analysis from the EMMY trial. Hellenic J Cardiol. 2023. https://doi.org/10.1016/j.hjc.2023.05.007.
Benedikt M, Mangge H, Aziz F, Curcic P, Pailer S, Herrmann M, et al. Impact of the SGLT2-inhibitor empagliflozin on inflammatory biomarkers after acute myocardial infarction – a post-hoc analysis of the EMMY trial. Cardiovasc Diabetol. 2023;22:166.
McDonald M, Virani S, Chan M, Ducharme A, Ezekowitz JA, Giannetti N, et al. CCS/CHFS heart failure guidelines update: defining a new pharmacologic standard of care for heart failure with reduced ejection fraction. Can J Cardiol. 2021;37:531–46.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/hfsa guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:E895-1032.
Sardu C, Trotta MC, Sasso FC, Sacra C, Carpinella G, Mauro C, et al. SGLT2-inhibitors effects on the coronary fibrous cap thickness and MACEs in diabetic patients with inducible myocardial ischemia and multi vessels non-obstructive coronary artery stenosis. Cardiovasc Diabetol. 2023;22:80.
Gager GM, von Lewinski D, Sourij H, Jilma B, Eyileten C, Filipiak K, et al. Effects of SGLT2 Inhibitors on Ion Homeostasis and Oxidative Stress associated Mechanisms in Heart Failure. Biomed Pharmacother. 2021;143: 112169.
D’Onofrio N, Sardu C, Trotta MC, Scisciola L, Turriziani F, Ferraraccio F, et al. Sodium-glucose co-transporter2 expression and inflammatory activity in diabetic atherosclerotic plaques: effects of sodium-glucose co-transporter2 inhibitor treatment. Mol Metab. 2021;54: 101337.
Salvatore T, Caturano A, Galiero R, di Martino A, Albanese G, Vetrano E, et al. Cardiovascular benefits from gliflozins: effects on endothelial function. Biomedicines. 2021;9:1356.
Paolisso P, Bergamaschi L, Cesaro A, Gallinoro E, Gragnano F, Sardu C, et al. Impact of SGLT2-inhibitors on contrast-induced acute kidney injury in diabetic patients with acute myocardial infarction with and without chronic kidney disease: Insight from SGLT2-I AMI PROTECT registry. Diabetes Res Clin Pract. 2023;202: 110766.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflicts of interest/Competing interest
Ryaan EL-Andari, Nicholas Fialka, Jimmy Kang, Sabin J Bozso, Jayan Nagendran, and Jeevan Nagendran declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Author Contributions
REA: study design, conceptualization, literature search, data collection, data analysis, data interpretation, generation of figures, writing of the manuscript, approval of the final manuscript. NF: study design, conceptualization, literature search, data interpretation, writing and proofreading the manuscript, approval of the final manuscript. JK: study design, conceptualization, data interpretation, writing and proofreading the manuscript, approval of the final manuscript. SJB: study design, conceptualization, data interpretation, writing and proofreading the manuscript, approval of the final manuscript. Jayan N: study design, conceptualization, data interpretation, writing and proofreading the manuscript, approval of the final manuscript. Jeevan N: study design, conceptualization, data interpretation, writing and proofreading the manuscript, approval of the final manuscript.
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
EL-Andari, R., Fialka, N.M., Kang, J. et al. The Use of Sodium-Glucose Cotransporter-2 Inhibitors in Coronary Revascularization: Where Are We Now? A Systematic Review. Am J Cardiovasc Drugs 24, 55–69 (2024). https://doi.org/10.1007/s40256-023-00618-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-023-00618-0