Abstract
Background
Patients with left ventricular thrombus are at high risk for ischemic stroke and systemic embolization. The mainstay of treatment is anticoagulation, but it remains unclear if direct-acting oral anticoagulants (DOACs) are a safe and effective treatment strategy compared to warfarin. We conducted a population-based retrospective cohort study to evaluate the effectiveness and safety of DOACs compared to warfarin in an integrated health system in the United States.
Methods
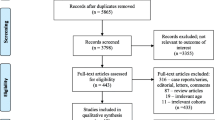
Consecutive patients with left ventricular thrombus on transthoracic echocardiogram from May 2010 to April 2020 were identified. Comparative effectiveness and safety of DOACs and warfarin were evaluated using multivariable Cox proportional hazard models and inverse probability of treatment weighting.
Results
Among 433 patients with left ventricular thrombus, 134 (30.9%) were treated with DOACs and 299 (69.1%) were treated with warfarin. Patients were followed for a median of 3.4 years. For the primary effectiveness outcome of ischemic stroke, systemic embolism, and transient ischemic attack, no significant difference was observed between use of DOACs compared to warfarin (adjusted hazard ratio [HR] of 0.75, 95% confidence interval [CI] 0.48–1.18, p = 0.21). For the primary safety outcome of intracranial hemorrhage, gastrointestinal bleeding, and other bleed requiring hospitalization, DOAC usage was associated with a lower risk of bleeding (HR 0.58, 95% CI 0.39–0.87, p = 0.0008).
Conclusions
In this diverse population-based cohort of patients, DOAC treatment for left ventricular thrombus appears to be as safe and effective as warfarin treatment. These findings support the use of DOACs for patients with left ventricular thrombus.


Similar content being viewed by others
References
Robinson AA, Jain A, Gentry M, McNamara RL. Left ventricular thrombi after STEMI in the primary PCI era: a systematic review and meta-analysis. Int J Cardiol. 2016;15(221):554–9.
Nihoyannopoulos P, Smith GC, Maseri A, Foale RA. The natural history of left ventricular thrombus in myocardial infarction: a rationale in support of masterly inactivity. J Am Coll Cardiol. 1989;14(4):903–11.
Visser CA, Kan G, Lie KI, Durrer D. Left ventricular thrombus following acute myocardial infarction: a prospective serial echocardiographic study of 96 patients. Eur Heart J. 1983;4(5):333–7.
Jugdutt BI, Sivaram CA. Prospective two-dimensional echocardiographic evaluation of left ventricular thrombus and embolism after acute myocardial infarction. J Am Coll Cardiol. 1989;13(3):554–64.
Asinger RW, Mikell FL, Elsperger J, Hodges M. Incidence of left-ventricular thrombosis after acute transmural myocardial infarction. Serial evaluation by two-dimensional echocardiography. N Engl J Med. 1981;305(6):297–302.
Weinsaft JW, Kim J, Medicherla CB, Ma CL, Codella NC, Kukar N, et al. Echocardiographic algorithm for post-myocardial infarction LV thrombus: a gatekeeper for thrombus evaluation by delayed enhancement CMR. JACC Cardiovasc Imaging. 2016;9(5):505–15.
Poss J, Desch S, Eitel C, de Waha S, Thiele H, Eitel I. Left ventricular thrombus formation after ST-segment-elevation myocardial infarction: insights from a cardiac magnetic resonance multicenter study. Circ Cardiovasc Imaging. 2015;8(10):e003417.
Gianstefani S, Douiri A, Delithanasis I, Rogers T, Sen A, Kalra S, et al. Incidence and predictors of early left ventricular thrombus after ST-elevation myocardial infarction in the contemporary era of primary percutaneous coronary intervention. Am J Cardiol. 2014;113(7):1111–6.
Vaitkus PT, Barnathan ES. Embolic potential, prevention and management of mural thrombus complicating anterior myocardial infarction: a meta-analysis. J Am Coll Cardiol. 1993;22(4):1004–9.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Eikelboom JW, Connolly SJ, Brueckmann M, Granger CB, Kappetein AP, Mack MJ, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013;369(13):1206–14.
Abdelnabi M, Saleh Y, Fareed A, Nossikof A, Wang L, Morsi M, et al. Comparative study of oral anticoagulation in left ventricular thrombi (No-LVT Trial). J Am Coll Cardiol. 2021;77(12):1590–2.
Alcalai R, Butnaru A, Moravsky G, Yagel O, Rashad R, Ibrahimli M, et al. Apixaban versus warfarin in patients with left ventricular thrombus, a prospective multicenter randomized clinical trial. Eur Heart J Cardiovasc Pharmacother. 2021. https://doi.org/10.1093/ehjcvp/pvab057
Robinson AA, Trankle CR, Eubanks G, Schumann C, Thompson P, Wallace RL, et al. Off-label use of direct oral anticoagulants compared with warfarin for left ventricular thrombi. JAMA Cardiol. 2020;5(6):685–92.
Ali Z, Isom N, Dalia T, Sami F, Mahmood U, Shah Z, et al. Direct oral anticoagulant use in left ventricular thrombus. Thromb J. 2020;18:29.
Guddeti RR, Anwar M, Walters RW, Apala D, Pajjuru V, Kousa O, et al. Treatment of left ventricular thrombus with direct oral anticoagulants: a retrospective observational study. Am J Med. 2020;133(12):1488–91.
Dalia T, Lahan S, Ranka S, Goyal A, Zoubek S, Gupta K, et al. Warfarin versus direct oral anticoagulants for treating left ventricular thrombus: a systematic review and meta-analysis. Thromb J. 2021;19(1):7.
Beyer-Westendorf J, Forster K, Ebertz F, Gelbricht V, Schreier T, Gobelt M, et al. Drug persistence with rivaroxaban therapy in atrial fibrillation patients-results from the Dresden non-interventional oral anticoagulation registry. Europace. 2015;17(4):530–8.
Garkina SV, Vavilova TV, Lebedev DS, Mikhaylov EN. Compliance and adherence to oral anticoagulation therapy in elderly patients with atrial fibrillation in the era of direct oral anticoagulants. J Geriatr Cardiol. 2016;13(9):807–10.
Derose SF, Contreras R, Coleman KJ, Koebnick C, Jacobsen SJ. Race and ethnicity data quality and imputation using US Census data in an integrated health system: the Kaiser Permanente Southern California experience. Med Care Res Rev. 2013;70(3):330–45.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–72.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Roberti R, Iannone LF, Palleria C, Curcio A, Rossi M, Sciacqua A, et al. Direct oral anticoagulants: from randomized clinical trials to real-world clinical practice. Front Pharmacol. 2021;12:684638.
Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342–52.
Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799–808.
Lopez-Lopez JA, Sterne JAC, Thom HHZ, Higgins JPT, Hingorani AD, Okoli GN, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ. 2017;359:j5058.
White HD, Gruber M, Feyzi J, Kaatz S, Tse HF, Husted S, et al. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med. 2007;167(3):239–45.
Jones M, McEwan P, Morgan CL, Peters JR, Goodfellow J, Currie CJ. Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non-valvar atrial fibrillation: a record linkage study in a large British population. Heart. 2005;91(4):472–7.
Sarawate C, Sikirica MV, Willey VJ, Bullano MF, Hauch O. Monitoring anticoagulation in atrial fibrillation. J Thromb Thrombolysis. 2006;21(2):191–8.
Connolly SJ, Pogue J, Eikelboom J, Flaker G, Commerford P, Franzosi MG, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008;118(20):2029–37.
Leow AS, Sia CH, Tan BY, Kaur R, Yeo TC, Chan MY, et al. Characterisation of acute ischemic stroke in patients with left ventricular thrombi after myocardial infarction. J Thromb Thrombolysis. 2019;48(1):158–66.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–236.
Bass ME, Kiser TH, Page RL 2nd, McIlvennan CK, Allen LA, Wright G, et al. Comparative effectiveness of direct oral anticoagulants and warfarin for the treatment of left ventricular thrombus. J Thromb Thrombolysis. 2021;52(2):517–22.
Iqbal H, Straw S, Craven TP, Stirling K, Wheatcroft SB, Witte KK. Direct oral anticoagulants compared to vitamin K antagonist for the management of left ventricular thrombus. ESC Heart Fail. 2020;7(5):2032–41.
Fleddermann AM, Hayes CH, Magalski A, Main ML. Efficacy of direct acting oral anticoagulants in treatment of left ventricular thrombus. Am J Cardiol. 2019;124(3):367–72.
Mueller T, Alvarez-Madrazo S, Robertson C, Wu O, Bennie M. Comparative safety and effectiveness of direct oral anticoagulants in patients with atrial fibrillation in clinical practice in Scotland. Br J Clin Pharmacol. 2019;85(2):422–31.
Lip GY, Larsen TB, Skjoth F, Rasmussen LH. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J Am Coll Cardiol. 2012;60(8):738–46.
Fu W, Guo H, Guo J, Lin K, Wang H, Zhang Y, et al. Relative efficacy and safety of direct oral anticoagulants in patients with atrial fibrillation by network meta-analysis. J Cardiovasc Med (Hagerstown). 2014;15(12):873–9.
Schneeweiss S, Gagne JJ, Patrick AR, Choudhry NK, Avorn J. Comparative efficacy and safety of new oral anticoagulants in patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2012;5(4):480–6.
Allard L, Bernhard B, Windecker S, Valgimigli M, Grani C. Left ventricular thrombus in ischaemic heart disease: diagnosis, treatment and gaps of knowledge. Eur Heart J Qual Care Clin Outcomes. 2021. https://doi.org/10.1093/ehjqcco/qcab097
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflict of interest
John Herald, Jesse Goitia, Lewei Duan, Aiyu Chen, and Ming-Sum Lee declare that they have no potential conflicts of interest that might be relevant to the contents of this article.
Ethics approval
The present study was approved by the Kaiser Permanente Southern California Institutional Review Board.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
JH: investigation, validation, writing; JG: conceptualization, investigation, data curation, methodology, reviewing; LD: data curation, analysis, reviewing, methodology; AC: data curation, analysis, reviewing; MSL: conceptualization, investigation, methodology, writing, reviewing, editing.
Rights and permissions
About this article
Cite this article
Herald, J., Goitia, J., Duan, L. et al. Safety and Effectiveness of Direct Oral Anticoagulants Versus Warfarin for Treating Left Ventricular Thrombus. Am J Cardiovasc Drugs 22, 437–444 (2022). https://doi.org/10.1007/s40256-022-00533-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-022-00533-w