Abstract
Type 2 diabetes mellitus (T2DM) is associated with high cardiovascular morbidity and mortality, and cardiovascular diseases are the leading causes of death and disability in people with T2DM. Unfortunately, therapies strictly aimed at glycemic control have poorly contributed to a significant reduction in the risk of cardiovascular events. On the other hand, randomized controlled trials have shown that five glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and one exendin-based GLP-1 RA reduced atherosclerotic cardiovascular events in patients with diabetes at high cardiovascular risk. Furthermore, a meta-analysis including these six agents showed a reduction in major adverse cardiovascular events as well as all-cause mortality compared with placebo, regardless of structural homology. Evidence has also shown that some drugs in this class have beneficial effects on renal outcomes, such as preventing the onset of macroalbuminuria. In addition to lowering blood pressure, these drugs also favorably impacted on body weight in large randomized controlled trials as in real-world studies, a result considered a priority in T2DM management; these and other factors may justify the benefits of GLP-1 RAs upon the cardiovascular system, regardless of glycemic control. Finally, studies showed safety with a low risk of hypoglycemia and no increase in pancreatitis events. Given these benefits, GLP-1 RAs were preferentially endorsed in the guidelines of the European and American societies for patients with these conditions. This narrative review provides a current and comprehensive overview of GLP-1 RAs as cardiovascular and renal protective agents, far beyond their use as glucose-lowering drugs, supporting their effectiveness in treating patients with T2DM at high cardiovascular risk.




Similar content being viewed by others
References
Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. 2019;74(20):2529–32. https://doi.org/10.1016/j.jacc.2019.10.009.
Dunbar SB, et al. Projected costs of informal caregiving for cardiovascular disease: 2015 to 2035: a policy statement from the American Heart Association. Circulation. 2018;137(19):e558–77. https://doi.org/10.1161/CIR.0000000000000570.
Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21(4):21. https://doi.org/10.1007/s11886-019-1107-y.
Raghavan S, et al. Diabetes mellitus-related all-cause and cardiovascular mortality in a national cohort of adults. J Am Heart Assoc. 2019;8(4): e011295. https://doi.org/10.1161/JAHA.118.011295.
Penna C, et al. Effect of hyperglycaemia and diabetes on acute myocardial ischaemia-reperfusion injury and cardioprotection by ischaemic conditioning protocols. Br J Pharmacol. 2020;177(23):5312–35. https://doi.org/10.1111/bph.14993.
Fox CS, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2015;38(9):1777–803. https://doi.org/10.2337/dci15-0012.
Ray KK, et al. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: a meta-analysis of randomised controlled trials. Lancet. 2009;373(9677):1765–72. https://doi.org/10.1016/S0140-6736(09)60697-8.
Ferrari F, et al. The role of sodium-glucose cotransporter-2 inhibitors in patients with heart failure, regardless of diabetes status: focus on cardiovascular disease. Ann Pharmacother. 2021;55(10):1267–75. https://doi.org/10.1177/1060028020985111.
[No authors listed]. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):854–65. https://doi.org/10.1016/S0140-6736(98)07037-8.
Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356(24):2457–71. https://doi.org/10.1056/NEJMoa072761.
Hiatt WR, Kaul S, Smith RJ. The cardiovascular safety of diabetes drugs—insights from the rosiglitazone experience. N Engl J Med. 2013;369:1285–7. https://doi.org/10.1056/NEJMp1309610.
Gourgari E, Wilhelm EE, Hassanzadeh H, Aroda VR, Shoulson I. A comprehensive review of the FDA-approved labels of diabetes drugs: indications, safety, and emerging cardiovascular safety data. J Diabetes Complications. 2017;31(12):1719–27. https://doi.org/10.1016/j.jdiacomp.2017.08.005.
Marso SP, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44. https://doi.org/10.1056/NEJMoa1607141.
Husain M, et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2019;381(9):841–51. https://doi.org/10.1056/NEJMoa1901118.
Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res. 2010;107(9):1058–70. https://doi.org/10.1161/CIRCRESAHA.110.223545.
Tessari P, et al. Nitric oxide synthesis is reduced in subjects with type 2 diabetes and nephropathy. Diabetes. 2010;59(9):2152–9. https://doi.org/10.2337/db09-1772.
Deacon CF. Physiology and pharmacology of dpp-4 in glucose homeostasis and the treatment of type 2 diabetes. Front Endocrinol (Lausanne). 2019;10:80. https://doi.org/10.3389/fendo.2019.00080.
Pomero F, Di Minno MN, Fenoglio L, Gianni M, Ageno W, Dentali F. Is diabetes a hypercoagulable state? A critical appraisal. Acta Diabetol. 2015;52(6):1007–16. https://doi.org/10.1007/s00592-015-0746-8.
Schaan BD, et al. Diabetes and cardiovascular events in high-risk patients: Insights from a multicenter registry in a middle-income country. Diabetes Res Clin Pract. 2017;127:275–84. https://doi.org/10.1016/j.diabres.2017.03.021.
Gregg EW, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–23. https://doi.org/10.1056/NEJMoa1310799.
Rawshani A, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379(7):633–44. https://doi.org/10.1056/NEJMoa1800256.
Ramracheya R, et al. GLP-1 suppresses glucagon secretion in human pancreatic alpha-cells by inhibition of P/Q-type Ca2+ channels. Physiol Rep. 2018;6(17): e13852. https://doi.org/10.14814/phy2.13852.
Lastya A, Saraswati MR, Suastika K. The low level of glucagon-like peptide-1 (glp-1) is a risk factor of type 2 diabetes mellitus. BMC Res Notes. 2014;7:849. https://doi.org/10.1186/1756-0500-7-849.
Anderson JW, Kendall CW, Jenkins DJ. Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr. 2003;22(5):331–9. https://doi.org/10.1080/07315724.2003.10719316.
Crane J, McGowan B. The GLP-1 agonist, liraglutide, as a pharmacotherapy for obesity. Ther Adv Chronic Dis. 2016;7(2):92–107. https://doi.org/10.1177/2040622315620180.
Skibicka KP. The central GLP-1: implications for food and drug reward. Front Neurosci. 2013;7:181. https://doi.org/10.3389/fnins.2013.00181.
Richard JE, Anderberg RH, Göteson A, Gribble FM, Reimann F, Skibicka KP. Activation of the GLP-1 receptors in the nucleus of the solitary tract reduces food reward behavior and targets the mesolimbic system. PLoS ONE. 2015;10(3): e0119034. https://doi.org/10.1371/journal.pone.0119034.
Sharma D, Verma S, Vaidya S, Kalia K, Tiwari V. Recent updates on GLP-1 agonists: current advancements and challenges. Biomed Pharmacother. 2018;108:952–62. https://doi.org/10.1016/j.biopha.2018.08.088.
Kalra S, Sahay R. A review on semaglutide: an oral glucagon-like peptide 1 receptor agonist in management of type 2 diabetes mellitus. Diabetes Ther. 2020;11:1965–82. https://doi.org/10.1007/s13300-020-00894-y.
Prasad-Reddy L, Isaacs D. A clinical review of GLP-1 receptor agonists: efficacy and safety in diabetes and beyond. Drugs Context. 2015;4: 212283. https://doi.org/10.7573/dic.212283.
Pfeffer MA, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–57. https://doi.org/10.1056/NEJMoa1509225.
Marso SP, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. https://doi.org/10.1056/NEJMoa1603827.
Mann JFE, et al. Liraglutide and renal outcomes in type 2 diabetes. N Engl J Med. 2017;377(9):839–48. https://doi.org/10.1056/NEJMoa1616011.
Marson SP, et al. Effects of liraglutide on cardiovascular outcomes in patients with diabetes with or without heart failure. J Am Coll Cardiol. 2020;75(10):1128–41. https://doi.org/10.1016/j.jacc.2019.12.063.
Cosentino F, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323. https://doi.org/10.1093/eurheartj/ehz486.
Leiter LA, et al. Cardiovascular risk reduction with once-weekly semaglutide in subjects with type 2 diabetes: a post hoc analysis of gender, age, and baseline CV risk profile in the SUSTAIN 6 trial. Cardiovasc Diabetol. 2019;18(1):73. https://doi.org/10.1186/s12933-019-0871-8.
Holman RR, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228–39. https://doi.org/10.1056/NEJMoa1612917.
Gerstein HC, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30. https://doi.org/10.1016/S0140-6736(19)31149-3.
Gerstein HC, et al. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Lancet. 2019;394(10193):131–8. https://doi.org/10.1016/S0140-6736(19)31150-X.
Hernandez AF, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018;392(10157):1519–29. https://doi.org/10.1016/S0140-6736(18)32261-X.
Nuhoho S, Gupta J, Hansen BB, Fletcher-Louis M, Dang-Tan T, Paine A. Orally administered semaglutide versus glp-1 ras in patients with type 2 diabetes previously receiving 1–2 oral antidiabetics: systematic review and network meta-analysis. Diabetes Ther. 2019;10(6):2183–99. https://doi.org/10.1007/s13300-019-00706-y.
Gerstein HC, et al. Cardiovascular and renal outcomes with efpeglenatide in type 2 diabetes. N Engl J Med. 2021;385:896–907. https://doi.org/10.1056/NEJMoa2108269.
Pratley RE, et al. Body weight management and safety with efpeglenatide in adults without diabetes: a phase II randomized study. Diabetes Obes Metab. 2019;21(11):2429–39. https://doi.org/10.1111/dom.13824.
Rosenstock J, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 2021;398(10295):143–55. https://doi.org/10.1016/S0140-6736(21)01324-6 (Epub 2021 June 27; Erratum in: Lancet. 2021;398(10296):212).
Frías JP, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503–15. https://doi.org/10.1056/NEJMoa2107519.
Wilson JM, et al. The dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist, tirzepatide, improves lipoprotein biomarkers associated with insulin resistance and cardiovascular risk in patients with type 2 diabetes. Diabetes Obes Metab. 2020;22(12):2451–9. https://doi.org/10.1111/dom.14174.
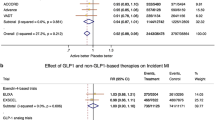
Kristensen SL, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7(10):776–85. https://doi.org/10.1016/S2213-8587(19)30249-9.
Giugliano D, Maiorino MI, Bellastella G, Longo M, Chiodini P, Esposito K. GLP-1 receptor agonists for prevention of cardiorenal outcomes in type 2 diabetes: an updated meta-analysis including the REWIND and PIONEER 6 trials. Diabetes Obes Metab. 2019;21(11):2576–80.
Sattar N, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet. 2021;9(10):653–62. https://doi.org/10.1016/S2213-8587(21)00203-5.
Giugliano D, et al. GLP-1 receptor agonists and cardiorenal outcomes in type 2 diabetes: an updated meta-analysis of eight CVOTs. Cardiovasc Diabetol. 2021;20(1):189. https://doi.org/10.1186/s12933-021-01366-8.
Qian W, Liu F, Yang Q. Effect of glucagon-like peptide-1 receptor agonists in subjects with type 2 diabetes mellitus: a meta-analysis. J Clin Pharm Ther. 2021. https://doi.org/10.1111/jcpt.13502 (Epub ahead of print).
Palmer SC, et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2021;13(372): m4573. https://doi.org/10.1136/bmj.m4573.
Uneda K, et al. Systematic review and meta-analysis for prevention of cardiovascular complications using GLP-1 receptor agonists and SGLT-2 inhibitors in obese diabetic patients. Sci Rep. 2021;11(1):10166. https://doi.org/10.1038/s41598-021-89620-7.
Ida S, et al. Effects of oral antidiabetic drugs and glucagon-like peptide-1 receptor agonists on left ventricular diastolic function in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis. Heart Fail Rev. 2021;26(5):1151–8. https://doi.org/10.1007/s10741-020-09936-w.
Marsico F, et al. Effects of glucagon-like peptide-1 receptor agonists on major cardiovascular events in patients with Type 2 diabetes mellitus with or without established cardiovascular disease: a meta-analysis of randomized controlled trials. Eur Heart J. 2020;41(35):3346–58. https://doi.org/10.1093/eurheartj/ehaa082.
Patoulias D, Papadopoulos C, Stavropoulos K, Imprialos K, Doumas M. Updated meta-analysis of trials assessing the cardiovascular efficacy of sodium-glucose co-transporter-2 inhibitors and glucagon-like peptide-1 receptor agonists in black patients. Am J Cardiol. 2020;15(137):133–5. https://doi.org/10.1016/j.amjcard.2020.10.004.
Mata-Cases M, Franch-Nadal J, Ortega E, Real J, Gratacòs M, Vlacho B, Mauricio D. Glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: real-world evidence from a Mediterranean area. Curr Med Res Opin. 2019;35(10):1735–44.
Feher M, et al. Effectiveness of liraglutide and lixisenatide in the treatment of type 2 diabetes: real-world evidence from The Health Improvement Network (THIN) Database in the United Kingdom. Diabetes Ther. 2017;8(2):417–31.
Ishigaki Y, et al. Glucagon-like peptide-1 receptor agonist utilization in type 2 diabetes in Japan: a retrospective database analysis (JDDM 57). Diabetes Ther. 2021;12(1):345–61. https://doi.org/10.1007/s13300-020-00977-w.
Ostawal A, Mocevic E, Kragh N, Xu W. Clinical effectiveness of liraglutide in type 2 diabetes treatment in the real-world setting: a systematic literature review. Diabetes Ther. 2016;7(3):411–38. https://doi.org/10.1007/s13300-016-0180-0.
Moreno Obregón F, et al. Real-life experience with dulaglutide: analysis of clinical effectiveness to 24 months. Diabetes Res Clin Pract. 2019;158: 107916. https://doi.org/10.1016/j.diabres.2019.107916.
Baviera M, et al. Lower risk of death and cardiovascular events in patients with diabetes initiating glucagon-like peptide-1 receptor agonists or sodium-glucose cotransporter-2 inhibitors: a real-world study in two Italian cohorts. Diabetes Obes Metab. 2021;23(7):1484–95. https://doi.org/10.1111/dom.14361.
Longato E, Di Camillo B, Sparacino G, Gubian L, Avogaro A, Fadini GP. Cardiovascular outcomes of type 2 diabetic patients treated with SGLT-2 inhibitors versus GLP-1 receptor agonists in real-life. BMJ Open Diabetes Res Care. 2020;8:e001451.
Pasternak B, et al. Use of glucagon-like peptide 1 receptor agonists and risk of serious renal events: scandinavian cohort study. Diabetes Care. 2020;43:1326–35.
Zerovnik S, Kos M, Locatelli I. Cardiovascular morbidity and mortality in patients with type 2 diabetes using novel antidiabetic medicines as add-on therapy: an observational real-world study. BMJ Open. 2021;11(9): e051549. https://doi.org/10.1136/bmjopen-2021-051549.
Rea F, Ciardullo S, Savaré L, Perseghin G, Corrao G. Comparing medication persistence among patients with type 2 diabetes using sodium-glucose cotransporter 2 inhibitors or glucagon-like peptide-1 receptor agonists in real-world setting. Diabetes Res Clin Pract. 2021;3: 109035. https://doi.org/10.1016/j.diabres.2021.109035.
Trevisan M, et al. Glucagon-like peptide-1 receptor agonists and the risk of cardiovascular events in diabetes patients surviving an acute myocardial infarction. Eur Heart J Cardiovasc Pharmacother. 2021;7(2):104–11. https://doi.org/10.1093/ehjcvp/pvaa004.
Dong Z, et al. Protein kinase A mediates glucagon-like peptide 1-induced nitric oxide production and muscle microvascular recruitment. Am J Physiol Endocrinol Metab. 2013;304(2):E222–8. https://doi.org/10.1152/ajpendo.00473.2012.
Almutairi M, Al Batran R, Ussher JR. Glucagon-like peptide-1 receptor action in the vasculature. Peptides. 2019;111:26–32. https://doi.org/10.1016/j.peptides.2018.09.002.
Li Y, et al. Liraglutide protects against lethal renal ischemia-reperfusion injury by inhibiting high-mobility group box 1 nuclear-cytoplasmic translocation and release. Pharmacol Res. 2021;1: 105867. https://doi.org/10.1016/j.phrs.2021.105867.
Shi L, et al. Liraglutide attenuates high glucose-induced abnormal cell migration, proliferation, and apoptosis of vascular smooth muscle cells by activating the GLP-1 receptor, and inhibiting ERK1/2 and PI3K/Akt signaling pathways. Cardiovasc Diabetol. 2015;7(14):18. https://doi.org/10.1186/s12933-015-0177-4.
Bruen R, et al. Liraglutide dictates macrophage phenotype in apolipoprotein E null mice during early atherosclerosis. Cardiovasc Diabetol. 2017;16(1):143.
Dieter BP, Alicic RZ, Tuttle KR. GLP-1 receptor agonists in diabetic kidney disease: from the patient-side to the bench-side. Am J Physiol Ren Physiol. 2018;315(6):F1519–25. https://doi.org/10.1152/ajprenal.00211.2018.
Ding L, Zhang J. Glucagon-like peptide-1 activates endothelial nitric oxide synthase in human umbilical vein endothelial cells. Acta Pharmacol Sin. 2012;33(1):75–81. https://doi.org/10.1038/aps.2011.149.
Katsurada K, Nandi SS, Sharma NM, Zheng H, Liu X, Patel KP. Does glucagon-like peptide-1 induce diuresis and natriuresis by modulating afferent renal nerve activity? Am J Physiol Ren Physiol. 2019;317(4):F1010–21. https://doi.org/10.1152/ajprenal.00028.2019.
Rakipovski G, et al. The GLP-1 analogs liraglutide and semaglutide reduce atherosclerosis in ApoE−/− and LDLr−/− mice by a mechanism that includes inflammatory pathways. JACC Basic Transl Sci. 2018;3(6):844–57. https://doi.org/10.1016/j.jacbts.2018.09.004.
Hogan AE, et al. Glucagon-like peptide 1 analogue therapy directly modulates innate immune-mediated inflammation in individuals with type 2 diabetes mellitus. Diabetologia. 2014;57(4):781–4. https://doi.org/10.1007/s00125-013-3145-0.
Zhang Y, Chen R, Jia Y, Chen M, Shuai Z. Effects of exenatide on coagulation and platelet aggregation in patients with type 2 diabetes. Drug Des Devel Ther. 2021;15:3027–40. https://doi.org/10.2147/DDDT.S312347.
Ninčević V, Omanović Kolarić T, Roguljić H, Kizivat T, Smolić M, Bilić ĆI. Renal benefits of SGLT 2 inhibitors and GLP-1 receptor agonists: evidence supporting a paradigm shift in the medical management of type 2 diabetes. Int J Mol Sci. 2019;20(23):5831. https://doi.org/10.3390/ijms20235831.
Neeland IJ, et al. Effects of liraglutide on visceral and ectopic fat in adults with overweight and obesity at high cardiovascular risk: a randomised, double-blind, placebo-controlled, clinical trial. Lancet Diabetes Endocrinol. 2021;9(9):595–605. https://doi.org/10.1016/S2213-8587(21)00179-0.
Drab SR. Glucagon-like peptide-1 receptor agonists for type 2 diabetes: a clinical update of safety and efficacy. Curr Diabetes Rev. 2016;12(4):403–13. https://doi.org/10.2174/1573399812666151223093841.
Sterling J, Hua P, Dunaief JL, Cui QN, VanderBeek BL. Glucagon-like peptide 1 receptor agonist use is associated with reduced risk for glaucoma. Br J Ophthalmol. 2021. https://doi.org/10.1136/bjophthalmol-2021-319232 (Epub ahead of print).
Sun F, et al. Impact of GLP-1 receptor agonists on blood pressure, heart rate and hypertension among patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetes Res Clin Pract. 2015;110(1):26–37. https://doi.org/10.1016/j.diabres.2015.07.015.
Heuvelman VD, Van Raalte DH, Smits MM. Cardiovascular effects of glucagon-like peptide 1 receptor agonists: from mechanistic studies in humans to clinical outcomes. Cardiovasc Res. 2020;116(5):916–30. https://doi.org/10.1093/cvr/cvz323.
Smits MM, et al. Heart rate acceleration with GLP-1 receptor agonists in type 2 diabetes patients: an acute and 12-week randomised, double-blind, placebo-controlled trial. Eur J Endocrinol. 2017;176(1):77–86. https://doi.org/10.1530/EJE-16-0507.
Baker C, Retzik-Stahr C, Singh V, Plomondon R, Anderson V, Rasouli N. Should metformin remain the first-line therapy for treatment of type 2 diabetes? Ther Adv Endocrinol Metab. 2021;13(12):2042018820980225. https://doi.org/10.1177/2042018820980225.
An H, He L. Current understanding of metformin effect on the control of hyperglycemia in diabetes. J Endocrinol. 2016;228(3):R97-106. https://doi.org/10.1530/JOE-15-0447.
Song Y, Ma P, Gao Y, Xiao P, Xu L, Liu H. A bibliometrics analysis of metformin development from 1980 to 2019. Front Pharmacol. 2021;28(12): 645810. https://doi.org/10.3389/fphar.2021.645810.
Good CB, Pogach LM. Should metformin be first-line therapy for patients with type 2 diabetes and chronic kidney disease? Informed patients should decide. JAMA Intern Med. 2018;178(7):911–2.
Hur KY, et al. Metformin treatment for patients with diabetes and chronic kidney disease: a Korean Diabetes Association and Korean Society of Nephrology Consensus Statement. Diabetes Metab J. 2020;44(1):3–10. https://doi.org/10.4093/dmj.2020.0004.
Wang W, et al. Efficacy and safety of once-weekly dulaglutide versus insulin glargine in mainly Asian patients with type 2 diabetes mellitus on metformin and/or a sulphonylurea: a 52-week open-label, randomized phase III trial. Diabetes Obes Metab. 2019;21(2):234–43. https://doi.org/10.1111/dom.13506.
Virani SS, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–743. https://doi.org/10.1161/CIR.0000000000000950.
Shin H, Schneeweiss S, Glynn RJ, Patorno E. Trends in first-line glucose-lowering drug use in adults with type 2 diabetes in light of emerging evidence for SGLT-2i and GLP-1 RA. Diabetes Care. 2021;44(8):1774–82. https://doi.org/10.2337/dc20-2926.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S98–110. https://doi.org/10.2337/dc20-S009.
Davies MJ, et al. Management of hyperglycemia in type 2 diabetes, 2018: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701. https://doi.org/10.2337/dci18-0033.
Visseren FLJ, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2021;42(34):3227–337.
Das SR, et al. 2020 expert consensus decision pathway on novel therapies for cardiovascular risk reduction in patients with type 2 diabetes: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2020;76(9):1117–45. https://doi.org/10.1016/j.jacc.2020.05.037.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was partially supported by the Hospital de Clínicas de Porto Alegre Research Incentive Fund (FIPE-HCPA), Porto Alegre, Brazil, and by the Coordination for the Improvement of Higher Education Personnel—Brazil (CAPES)—funding code 001. FF receives financial support from CAPES. RDS is recipient of a Brazilian National Council for Scientific and Technological Development (CNPq) research scholarship (filing #303734/2018-3). RS receives research productivity funding from CNPq.
Conflicts of interest
RDS has received honoraria related to consulting, research, and/or speaker activities from Abbott, Amgen, Aché, Amryt, AstraZeneca, Esperion, EMS, Kowa, Hypera, Merck, MSD, Novo Nordisk, Novartis, PTC, Pfizer, Roche, and Sanofi. Filipe Ferrari, Rafael S. Scheffel, Vítor M. Martins, and Ricardo Stein have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors have read and approved the submission.
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Author contributions
Conception and design of the research; acquisition, analysis, and interpretation of the data; and writing of the manuscript: FF, RSS, VMM, RDS, RS. Critical revision of the manuscript for intellectual content: FF, RSS, RDS, RS.
Rights and permissions
About this article
Cite this article
Ferrari, F., Scheffel, R.S., Martins, V.M. et al. Glucagon-Like Peptide-1 Receptor Agonists in Type 2 Diabetes Mellitus and Cardiovascular Disease: The Past, Present, and Future. Am J Cardiovasc Drugs 22, 363–383 (2022). https://doi.org/10.1007/s40256-021-00515-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-021-00515-4