Abstract
Background
Obesity hypertension is an ongoing pandemic. The first-line medications to treat this condition are still subject to debate. We compared diuretics, calcium-channel blockers (CCB), beta-blockers (BB), angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB) as an initial antihypertensive therapy for prevention of cardiovascular morbimortality of hypertensive individuals who are overweight or obese.
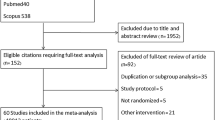
Methods
We conducted a search of the literature for randomized clinical trials in which at least 50% of the participants were overweight or obese. The primary outcomes were all-cause mortality, cardiovascular mortality, acute myocardial infarction (MI), heart failure (HF), stroke, or end-stage renal disease.
Results
Our search yielded 16 randomized studies. Comparisons of two classes of drugs with at least two studies indicated that (1) CCB and ACEI increased the risk of HF [relative risk (RR) = 2.26; 95% confidence interval (CI) 1.16–4.40] and stroke [hazard ratio (HR) = 1.13; 1.00–1.26]), respectively, compared to diuretics; and (2) CCB showed a reduction in stroke (HR = 0.77; 0.66–0.89) and total mortality (HR = 0.94; 0.87–1.01) compared to the BB atenolol. Comparisons of two classes of antihypertensive medications with only one study showed that the risk of MI was higher with ARB valsartan versus CCB (HR = 1.19; 95% CI 1.02–1.38, p = 0.02). In contrast, losartan lowered the risk of a composite cardiovascular outcome compared to atenolol (HR = 0.87; 95% CI 0.77–0.98, p = 0.02).
Conclusions
In hypertensive subjects with excess weight, diuretics are more effective for preventing HF and stroke than CCB and ACEI, respectively. CCB are a good first-line choice for prevention of cardiovascular disease, except HF.






Similar content being viewed by others
References
Obesity and Overweight. World Health Organization. 2018, https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 24 July 2019.
Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121(7):492–6. https://doi.org/10.1016/j.puhe.2007.01.006.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23. https://doi.org/10.1016/S0140-6736(05)17741-1.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50. https://doi.org/10.1161/CIRCULATIONAHA.115.018912.
Garrison RJ, Kannel WB, Stokes J 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987;16(2):235–51.
Kassab S, Kato T, Wilkins FC, Chen R, Hall JE, Granger JP. Renal denervation attenuates the sodium retention and hypertension associated with obesity. Hypertension. 1995;25(4 Pt 2):893–7.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991–1006. https://doi.org/10.1161/circresaha.116.305697.
Grassi G, Seravalle G, Dell’Oro R, Turri C, Bolla GB, Mancia G. Adrenergic and reflex abnormalities in obesity-related hypertension. Hypertension. 2000;36(4):538–42.
de Paula RB, da Silva AA, Hall JE. Aldosterone antagonism attenuates obesity-induced hypertension and glomerular hyperfiltration. Hypertension. 2004;43(1):41–7. https://doi.org/10.1161/01.HYP.0000105624.68174.00.
Briones AM, Nguyen Dinh Cat A, Callera GE, Yogi A, Burger D, He Y, et al. Adipocytes produce aldosterone through calcineurin-dependent signaling pathways: implications in diabetes mellitus-associated obesity and vascular dysfunction. Hypertension. 2012;59(5):1069–78. https://doi.org/10.1161/hypertensionaha.111.190223.
Cassano PA, Segal MR, Vokonas PS, Weiss ST. Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol. 1990;1(1):33–48.
Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128(2):81–8.
Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134(1):1–11.
Zhang T, Zhang H, Li S, Li Y, Liu Y, Fernandez C, et al. Impact of adiposity on incident hypertension is modified by insulin resistance in adults: longitudinal observation from the Bogalusa Heart Study. Hypertension. 2016;67(1):56–62. https://doi.org/10.1161/HYPERTENSIONAHA.115.06509.
Francischetti EA, Genelhu VA. Obesity-hypertension: an ongoing pandemic. Int J Clin Pract. 2007;61(2):269–80. https://doi.org/10.1111/j.1742-1241.2006.01262.x.
do Carmo JM, da Silva AA, Wang Z, Fang T, Aberdein N, de Lara Rodriguez CE, et al. Obesity-induced hypertension: brain signaling pathways. Curr Hypertens Rep. 2016;18(7):58. https://doi.org/10.1007/s11906-016-0658-1.
Rahmouni K, Correia ML, Haynes WG, Mark AL. Obesity-associated hypertension: new insights into mechanisms. Hypertension. 2005;45(1):9–14. https://doi.org/10.1161/01.HYP.0000151325.83008.b4.
Goodfriend TL, Calhoun DA. Resistant hypertension, obesity, sleep apnea, and aldosterone: theory and therapy. Hypertension. 2004;43(3):518–24. https://doi.org/10.1161/01.HYP.0000116223.97436.e5.
Cardillo C, Campia U, Iantorno M, Panza JA. Enhanced vascular activity of endogenous endothelin-1 in obese hypertensive patients. Hypertension. 2004;43(1):36–40. https://doi.org/10.1161/01.HYP.0000103868.45064.81.
Blood Pressure Lowering Treatment Trialists C, Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336(7653):1121–3. https://doi.org/10.1136/bmj.39548.738368.be.
de Simone G, Wachtell K, Palmieri V, Hille DA, Beevers G, Dahlof B, et al. Body build and risk of cardiovascular events in hypertension and left ventricular hypertrophy: the LIFE (Losartan Intervention For Endpoint reduction in hypertension) study. Circulation. 2005;111(15):1924–31. https://doi.org/10.1161/01.CIR.0000161799.91577.0A.
Weber MA, Jamerson K, Bakris GL, Weir MR, Zappe D, Zhang Y, et al. Effects of body size and hypertension treatments on cardiovascular event rates: subanalysis of the ACCOMPLISH randomised controlled trial. Lancet. 2013;381(9866):537–45. https://doi.org/10.1016/S0140-6736(12)61343-9.
Reisin E, Graves JW, Yamal JM, Barzilay JI, Pressel SL, Einhorn PT, et al. Blood pressure control and cardiovascular outcomes in normal-weight, overweight, and obese hypertensive patients treated with three different antihypertensives in ALLHAT. J Hypertens. 2014;32(7):1503–13. https://doi.org/10.1097/hjh.0000000000000204(discussion 13).
Jordan J, Yumuk V, Schlaich M, Nilsson PM, Zahorska-Markiewicz B, Grassi G, et al. Joint statement of the European Association for the Study of Obesity and the European Society of Hypertension: obesity and difficult to treat arterial hypertension. J Hypertens. 2012;30(6):1047–55. https://doi.org/10.1097/HJH.0b013e3283537347.
Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd-Jones D, et al. Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of the Obesity Society and the American Society of Hypertension. J Clin Hypertens. 2013;15(1):14–33. https://doi.org/10.1111/jch.12049.
Higgins JPT, Altman DG. Assessing risk of bias in included studies. Cochrane handbook for systermatic reviews of interventions West Sussex. Hoboken: Wiley; 2008. p. 187–241.
Altman DG, Bland JM. Detecting skewness from summary information. BMJ. 1996;313(7066):1200. https://doi.org/10.1136/bmj.313.7066.1200.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ. 2007;176(8):1091–6. https://doi.org/10.1503/cmaj.060410.
Brown MJ, Palmer CR, Castaigne A, de Leeuw PW, Mancia G, Rosenthal T, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet. 2000;356(9227):366–72. https://doi.org/10.1016/S0140-6736(00)02527-7.
Rosei EA, Dal Palu C, Leonetti G, Magnani B, Pessina A, Zanchetti A. Clinical results of the verapamil in hypertension and atherosclerosis study. VHAS Investigators. J Hypertens. 1997;15(11):1337–44.
Officers A, Coordinators for the ACRGTA, Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Jama. 2002;288(23):2981–97.
Borhani NO, Mercuri M, Borhani PA, Buckalew VM, Canossa-Terris M, Carr AA, et al. Final outcome results of the Multicenter Isradipine Diuretic Atherosclerosis Study (MIDAS). A randomized controlled trial. Jama. 1996;276(10):785–91.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417–28. https://doi.org/10.1056/NEJMoa0806182.
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906. https://doi.org/10.1016/S0140-6736(05)67185-1.
Zanchetti A, Bond MG, Hennig M, Neiss A, Mancia G, Dal Palu C, et al. Calcium antagonist lacidipine slows down progression of asymptomatic carotid atherosclerosis: principal results of the European Lacidipine Study on Atherosclerosis (ELSA), a randomized, double-blind, long-term trial. Circulation. 2002;106(19):2422–7.
Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli FH, et al. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. Jama. 2003;290(21):2805–16. https://doi.org/10.1001/jama.290.21.2805.
Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL, et al. A comparison of outcomes with angiotensin-converting–enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348(7):583–92. https://doi.org/10.1056/NEJMoa021716.
The Australian therapeutic trial in mild hypertension. Report by the Management Committee. Lancet. 1980;1(8181):1261–7.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). Jama. 1991;265(24):3255–64.
Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003. https://doi.org/10.1016/S0140-6736(02)08089-3.
Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022–31. https://doi.org/10.1016/S0140-6736(04)16451-9.
Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med. 1998;338(10):645–52. https://doi.org/10.1056/NEJM199803053381003.
Wilhelmsen L, Berglund G, Elmfeldt D, Fitzsimons T, Holzgreve H, Hosie J, et al. Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial. J Hypertens. 1987;5(5):561–72.
Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547–59. https://doi.org/10.1056/NEJMoa0801317.
Black HR, Davis B, Barzilay J, Nwachuku C, Baimbridge C, Marginean H, et al. Metabolic and clinical outcomes in nondiabetic individuals with the metabolic syndrome assigned to chlorthalidone, amlodipine, or lisinopril as initial treatment for hypertension: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Diabetes Care. 2008;31(2):353–60. https://doi.org/10.2337/dc07-1452.
Chapman N, Dobson J, Wilson S, Dahlof B, Sever PS, Wedel H, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49(4):839–45. https://doi.org/10.1161/01.HYP.0000259805.18468.8c.
Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68. https://doi.org/10.1016/S0140-6736(15)00257-3.
Alvarez-Alvarez B, Abad-Cardiel M, Fernandez-Cruz A, Martell-Claros N. Management of resistant arterial hypertension: role of spironolactone versus double blockade of the renin-angiotensin-aldosterone system. J Hypertens. 2010;28(11):2329–35. https://doi.org/10.1097/HJH.0b013e32833d4c99.
Vaclavik J, Sedlak R, Plachy M, Navratil K, Plasek J, Jarkovsky J, et al. Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension. 2011;57(6):1069–75. https://doi.org/10.1161/HYPERTENSIONAHA.111.169961.
Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone versus clonidine as a fourth-drug therapy for resistant hypertension: the ReHOT randomized study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681–90. https://doi.org/10.1161/HYPERTENSIONAHA.117.10662.
Oxlund CS, Henriksen JE, Tarnow L, Schousboe K, Gram J, Jacobsen IA. Low dose spironolactone reduces blood pressure in patients with resistant hypertension and type 2 diabetes mellitus: a double blind randomized clinical trial. J Hypertens. 2013;31(10):2094–102. https://doi.org/10.1097/HJH.0b013e3283638b1a.
Davis BR, Kostis JB, Simpson LM, Black HR, Cushman WC, Einhorn PT, et al. Heart failure with preserved and reduced left ventricular ejection fraction in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Circulation. 2008;118(22):2259–67. https://doi.org/10.1161/CIRCULATIONAHA.107.762229.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9. https://doi.org/10.1056/NEJMoa052256.
Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the framingham heart study of the national heart, lung, and blood institute. Circulation. 2009;119(24):3070–7. https://doi.org/10.1161/CIRCULATIONAHA.108.815944.
Jamerson KA, Devereux R, Bakris GL, Dahlof B, Pitt B, Velazquez EJ, et al. Efficacy and duration of benazepril plus amlodipine or hydrochlorothiazide on 24-hour ambulatory systolic blood pressure control. Hypertension. 2011;57(2):174–9. https://doi.org/10.1161/HYPERTENSIONAHA.110.159939.
Olde Engberink RH, Frenkel WJ, van den Bogaard B, Brewster LM, Vogt L, van den Born BJ. Effects of thiazide-type and thiazide-like diuretics on cardiovascular events and mortality: systematic review and meta-analysis. Hypertension. 2015;65(5):1033–40. https://doi.org/10.1161/HYPERTENSIONAHA.114.05122.
Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43(1):4–9. https://doi.org/10.1161/01.HYP.0000103632.19915.0E.
Ernst ME, Carter BL, Goerdt CJ, Steffensmeier JJ, Phillips BB, Zimmerman MB, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47(3):352–8. https://doi.org/10.1161/01.HYP.0000203309.07140.d3.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–115. https://doi.org/10.1161/HYP.0000000000000065.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–25. https://doi.org/10.1161/CIRCULATIONAHA.105.595496.
Angeli F, Verdecchia P, Reboldi GP, Gattobigio R, Bentivoglio M, Staessen JA, et al. Calcium channel blockade to prevent stroke in hypertension: a meta-analysis of 13 studies with 103,793 subjects. Am J Hypertens. 2004;17(9):817–22. https://doi.org/10.1016/j.amjhyper.2004.06.002.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. https://doi.org/10.1136/bmj.b1665.
Gress TW, Nieto FJ, Shahar E, Wofford MR, Brancati FL. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. Atherosclerosis Risk in Communities Study. N Engl J Med. 2000;342(13):905–12. https://doi.org/10.1056/nejm200003303421301.
Opie LH, Yusuf S, Kubler W. Current status of safety and efficacy of calcium channel blockers in cardiovascular diseases: a critical analysis based on 100 studies. Prog Cardiovasc Dis. 2000;43(2):171–96. https://doi.org/10.1053/pcad.2000.7010.
Carlberg B, Samuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004;364(9446):1684–9. https://doi.org/10.1016/S0140-6736(04)17355-8.
Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366(9496):1545–53. https://doi.org/10.1016/S0140-6736(05)67573-3.
Kuyper LM, Khan NA. Atenolol vs nonatenolol beta-blockers for the treatment of hypertension: a meta-analysis. Can J Cardiol. 2014;30(5 Suppl):S47–53. https://doi.org/10.1016/j.cjca.2014.01.006.
Wright JT Jr, Probstfield JL, Cushman WC, Pressel SL, Cutler JA, Davis BR, et al. ALLHAT findings revisited in the context of subsequent analyses, other trials, and meta-analyses. Arch Intern Med. 2009;169(9):832–42. https://doi.org/10.1001/archinternmed.2009.60.
Egan BM, Lackland DT, Cutler NE. Awareness, knowledge, and attitudes of older americans about high blood pressure: implications for health care policy, education, and research. Arch Intern Med. 2003;163(6):681–7.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–219. https://doi.org/10.1093/eurheartj/eht151.
Barzilay JI, Davis BR, Cutler JA, Pressel SL, Whelton PK, Basile J, et al. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2006;166(20):2191–201. https://doi.org/10.1001/archinte.166.20.2191.
Whelton PK, Barzilay J, Cushman WC, Davis BR, Iiamathi E, Kostis JB, et al. Clinical outcomes in antihypertensive treatment of type 2 diabetes, impaired fasting glucose concentration, and normoglycemia: antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2005;165(12):1401–9. https://doi.org/10.1001/archinte.165.12.1401.
Wright JT Jr, Harris-Haywood S, Pressel S, Barzilay J, Baimbridge C, Bareis CJ, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168(2):207–17. https://doi.org/10.1001/archinternmed.2007.66.
Wassertheil-Smoller S, Fann C, Allman RM, Black HR, Camel GH, Davis B, The SHEP Cooperative Research Group, et al. Relation of low body mass to death and stroke in the systolic hypertension in the elderly program. Arch Internal Med. 2000;160(4):494–500.
Group SR, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16. https://doi.org/10.1056/nejmoa1511939.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15. https://doi.org/10.1001/jama.2014.18574.
Larochelle P, Tobe SW, Lacourciere Y. beta-Blockers in hypertension: studies and meta-analyses over the years. Can J Cardiol. 2014;30(5 Suppl):S16–22. https://doi.org/10.1016/j.cjca.2014.02.012.
Zhang Y, Sun N, Jiang X, Xi Y. Comparative efficacy of beta-blockers on mortality and cardiovascular outcomes in patients with hypertension: a systematic review and network meta-analysis. J Am Soc Hypertens. 2017;11(7):394–401. https://doi.org/10.1016/j.jash.2017.05.001.
Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, et al. Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e116–35. https://doi.org/10.1161/HYP.0000000000000067.
Barnett AH, Bain SC, Bouter P, Karlberg B, Madsbad S, Jervell J, et al. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. N Engl J Med. 2004;351(19):1952–61. https://doi.org/10.1056/NEJMoa042274.
Strauss MH, Hall AS. Angiotensin receptor blockers may increase risk of myocardial infarction: unraveling the ARB-MI paradox. Circulation. 2006;114(8):838–54. https://doi.org/10.1161/CIRCULATIONAHA.105.594986.
Verma S, Strauss M. Angiotensin receptor blockers and myocardial infarction. BMJ. 2004;329(7477):1248–9. https://doi.org/10.1136/bmj.329.7477.1248.
Savarese G, Gotto AM Jr, Paolillo S, D’Amore C, Losco T, Musella F, et al. Benefits of statins in elderly subjects without established cardiovascular disease: a meta-analysis. J Am Coll Cardiol. 2013;62(22):2090–9. https://doi.org/10.1016/j.jacc.2013.07.069.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs–overview and meta-analyses. J Hypertens. 2015;33(2):195–211. https://doi.org/10.1097/hjh.0000000000000447.
Bangalore S, Makani H, Radford M, Thakur K, Toklu B, Katz SD, et al. Clinical outcomes with beta-blockers for myocardial infarction: a meta-analysis of randomized trials. Am J Med. 2014;127(10):939–53. https://doi.org/10.1016/j.amjmed.2014.05.032.
Cheng J, Zhang W, Zhang X, Han F, Li X, He X, et al. Effect of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on all-cause mortality, cardiovascular deaths, and cardiovascular events in patients with diabetes mellitus: a meta-analysis. JAMA Intern Med. 2014;174(5):773–85. https://doi.org/10.1001/jamainternmed.2014.348.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3–15. https://doi.org/10.1097/HJH.0000000000000065.
Acknowledgements
We would like to thank Mauricio de Assis Fontes for his helpful assistance in the preparation of this article.
Author information
Authors and Affiliations
Contributions
Authors contributed equally to the manuscript.
Corresponding author
Ethics declarations
Funding
ESFC received grants from (1) Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) (project E-26/202.938/2015; http://www.faperj.br/) and (2) Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (process no. 307045/20161; http://www.cnpq.br/). The funders had no direct role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
All authors (EAF, VGA, LFSF, RSD, and ESFC) declare that they have no potential conflicts of interest that might be relevant to the contents of this article.
Rights and permissions
About this article
Cite this article
Francischetti, E.A., de Abreu, V.G., da Silva Figueiredo, L.F. et al. Effects of Blood Pressure Lowering Agents on Cardiovascular Outcomes in Weight Excess Patients: A Systematic Review and Meta-analysis. Am J Cardiovasc Drugs 20, 447–470 (2020). https://doi.org/10.1007/s40256-019-00393-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-019-00393-x