Abstract
Purpose
Diabetes can cause nerve damage, vascular issues, and reduced blood flow to organs such as the feet, leading to foot deformities and ulcers due to high glucose levels. A healthy dietary pattern like DASH can improve insulin sensitivity and weight loss. Due to limited data and rare evidence, our study aims to investigate the relationship between DASH diet adherence and anthropometric, cardiovascular, and foot ulcer indicators.
Methods
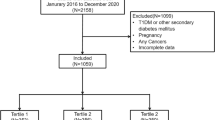
The study included 339 diabetic patients with foot ulcers (122 females and 217 males). The study gathered data on patient dietary intake, anthropometric measurements, biochemistry, foot ulcers, and novel atherogenic risk factors per international definitions.
Results
The average BMI of the participants was 29.2 ± 5.0, 28.1 ± 4.3, and 28.2 ± 4.2 in the tertiles of DASH index (P-value: 0.18). By increasing the adherence to the DASH index, the monofilament score did not change significantly OR: 1.47; CI: (0.81-2.67). Also, foot ulcer area did not change significantly between DASH tertiles OR: 1.01; CI: (0.56-1.83). Atherogenic risk factors also decreased among the DASH tertiles, but statistically not significant.
Conclusion
DASH adherence did not change neuropathy score and cholindex and cardiovascular risk factors significantly and has no significant effect on foot ulcer size.
Similar content being viewed by others
Data availability
The data, which is mentioned in the manuscript, will be made available upon request from the authors. Please feel free to contact the authors for access to the data.
Notes
Metabolic equivalent
Major adverse cardiovascular events
Myocardial infarction
Coronary artery bypass graft
Coronary artery disease
Cardiovascular
Abbreviations
- DASH:
-
Dietary Approaches to Stop Hypertension
- WC:
-
Waist Circumference
- HC:
-
Hip Circumference
- BMI:
-
Body Mass Index
- SES:
-
Socioeconomic Status
- MACE:
-
Major Adverse Cardiovascular Events
- SBP:
-
Systolic Blood Pressure
- DBP:
-
Diastolic Blood Pressure
- FBS:
-
Fasting Blood Sugar
- HbA1C:
-
Hemoglobin A1C
- TC:
-
Total Cholesterol
- TG:
-
Triglycerides
- HDL-C:
-
High Density Lipoprotein cholesterol
- LDL-C:
-
Low Density Lipoprotein cholesterol
- ABSI:
-
A Body Shape Index
- BRI:
-
Body Roundness Index
- AVI:
-
Abdominal Volume Index
- CRI-1:
-
Castelli Index-I
- CRI-II:
-
Castelli Index-II
- CI:
-
Cholesterol Index
- AIP:
-
Atherogenic Index of Plasma
- LAP:
-
Lipid Accumulation Plasma
- CVD:
-
Cardiovascular Disease
References
Basiri R, Spicer MT, Ledermann T, Arjmandi BH. Effects of nutrition intervention on blood glucose, body composition, and phase angle in obese and overweight patients with diabetic foot ulcers. Nutrients. 2022;14(17):3564. https://doi.org/10.3390/nu14173564.
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–75. https://doi.org/10.1056/NEJMra1615439.
Yazdanpanah L, Shahbazian H, Nazari I, Arti HR, Ahmadi F, Mohammadianinejad SE, Cheraghian B, Latifi SM. Prevalence and related risk factors of diabetic foot ulcer in Ahvaz, south west of Iran. Diabetes Metab Syndr. 2018;12(4):519–24. https://doi.org/10.1016/j.dsx.2018.03.018.
Armstrong DG, Hanft JR, Driver VR, Smith AP, Lazaro-Martinez JL, Reyzelman AM, Furst GJ, Vayser DJ, Cervantes HL, Snyder RJ, Moore MF, May PE, Nelson JL, Baggs GE, Voss AC. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled trial. Diabet Med. 2014;31(9):1069–77. https://doi.org/10.1111/dme.12509.
Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care. 1998;21(5):855–9. https://doi.org/10.2337/diacare.21.5.855.
Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and Cardiovascular diseases. Circ Res. 2020;126(11):1477–500. https://doi.org/10.1161/circresaha.120.316101.
Ahmed B, Sultana R, Greene MW. Adipose tissue and insulin resistance in obese. Biomed Pharmacother. 2021;137:111315. https://doi.org/10.1016/j.biopha.2021.111315.
He S, Chen X. Could the new body shape index predict the new onset of diabetes mellitus in the Chinese population? PLoS ONE. 2013;8(1):e50573. https://doi.org/10.1371/journal.pone.0050573.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, Maeda Y, McDougall A, Peterson CM, Ravussin E, Heymsfield SB. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obes (Silver Spring). 2013;21(11):2264–71. https://doi.org/10.1002/oby.20408.
Liu B, Liu B, Wu G, Yin F. Relationship between body-roundness index and metabolic syndrome in type 2 diabetes. Diabetes Metab Syndr Obes. 2019;12:931–5. https://doi.org/10.2147/dmso.S209964.
Geraci G, Zammuto M, Gaetani R, Mattina A, D’Ignoto F, Geraci C, Noto D, Averna M, Cottone S, Mulè G. Relationship of a body shape index and body roundness index with carotid atherosclerosis in arterial hypertension. Nutr Metab Cardiovasc Dis. 2019;29(8):822–9. https://doi.org/10.1016/j.numecd.2019.04.013.
Guerrero-Romero F, Rodríguez-Morán M. Abdominal volume index. An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. 2003;34(5):428–32. https://doi.org/10.1016/s0188-4409(03)00073-0.
Okamoto M, Nakamura F, Musha T, Kobayashi Y. Association between novel arterial stiffness indices and risk factors of cardiovascular disease. BMC Cardiovasc Disord. 2016;16(1):211. https://doi.org/10.1186/s12872-016-0389-x.
Hu X, Appleton AA, Ou Y, Zhang Y, Cai A, Zhou Y, Dong H. Abdominal volume index trajectories and risk of diabetes mellitus: results from the China Health and Nutrition Survey. J Diabetes Investig. 2022;13(5):868–77. https://doi.org/10.1111/jdi.13733.
Sabarinathan M, Ds DR, Ananthi N, Krishnan M. Atherogenic index of plasma, lipid accumulation and visceral adiposity in metabolic syndrome patients. Bioinformation. 2022;18(11):1109–13. https://doi.org/10.6026/973206300181109.
Fu L, Zhou Y, Sun J, Zhu Z, Xing Z, Zhou S, Wang Y, Tai S. Atherogenic index of plasma is associated with major adverse cardiovascular events in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2021;20(1):201. https://doi.org/10.1186/s12933-021-01393-5.
Akpınar O, Bozkurt A, Acartürk E, Seydaoğlu G. A new index (CHOLINDEX) in detecting coronary artery disease risk. Anadolu Kardiyol Derg. 2013;13(4):315–9. https://doi.org/10.5152/akd.2013.098.
Nunes SH, Nogueira Saad MA, da Cruz Filho RA, Jorge AJL, Santos M, Martins WA, Campos TL, Rosa MLG. Is lipid accumulation product a better cardiovascular risk predictor in elderly individuals than anthropometric measures? Rev Port Cardiol (Engl Ed). 2021;40(8):539–44. https://doi.org/10.1016/j.repce.2020.09.007.
Uusitupa M, Khan TA, Viguiliouk E, Kahleova H, Rivellese AA, Hermansen K, Pfeiffer A, Thanopoulou A, Salas-Salvadó J, Schwab U, Sievenpiper JL. Prevention of type 2 diabetes by Lifestyle changes: a systematic review and Meta-analysis. Nutrients. 2019;11(11):2611. https://doi.org/10.3390/nu11112611.
Martínez García RM, Fuentes Chacón RM, Lorenzo Mora AM, Ortega Anta RM. Nutrition in the prevention and healing of chronic wounds. Importance in improving the diabetic foot. Nutr Hosp. 2021;38(Spec No2):60–3. https://doi.org/10.20960/nh.03800.
Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 2010;25(1):61–8. https://doi.org/10.1177/0884533609358997.
Nestel PJ, Mori TA. Dietary patterns, dietary nutrients and cardiovascular disease. Rev Cardiovasc Med. 2022;23(1):17. https://doi.org/10.31083/j.rcm2301017.
Tapsell LC, Neale EP, Satija A, Hu FB. Foods, nutrients, and dietary patterns: interconnections and implications for dietary guidelines. Adv Nutr. 2016;7(3):445–54. https://doi.org/10.3945/an.115.011718.
Chiavaroli L, Viguiliouk E, Nishi SK, Blanco Mejia S, Rahelić D, Kahleová H, Salas-Salvadó J, Kendall CW, Sievenpiper JL. DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients. 2019;11(2). https://doi.org/10.3390/nu11020338
Shirani F, Salehi-Abargouei A, Azadbakht L. Effects of Dietary Approaches to Stop Hypertension (DASH) diet on some risk for developing type 2 diabetes: a systematic review and meta-analysis on controlled clinical trials. Nutrition. 2013;29(7–8):939–47. https://doi.org/10.1016/j.nut.2012.12.021.
Razavi Zade M, Telkabadi MH, Bahmani F, Salehi B, Farshbaf S, Asemi Z. The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: a randomized clinical trial. Liver Int. 2016;36(4):563–71. https://doi.org/10.1111/liv.12990.
Ibsen DB, Levitan EB, Åkesson A, Gigante B, Wolk A. The DASH diet is associated with a lower risk of heart failure: a cohort study. Eur J Prev Cardiol. 2022;29(7):1114–23. https://doi.org/10.1093/eurjpc/zwac003.
Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, Champagne CM, Hoben KP. Descriptive characteristics of the dietary patterns used in the Dietary approaches to stop hypertension trial. DASH Collaborative Research Group. J Am Diet Assoc. 1999;99(8 Suppl):S19-27. https://doi.org/10.1016/s0002-8223(99)00412-5.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20. https://doi.org/10.1001/archinte.168.7.713.
Panbehkar-Jouybari M, Mollahosseini M, Salehi-Abargouei A, Fallahzadeh H, Mirzaei M, Hosseinzadeh M. The Mediterranean diet and dietary approach to stop hypertension (DASH)-style diet are differently associated with lipid profile in a large sample of Iranian adults: a cross-sectional study of Shahedieh cohort. BMC Endocr Disord. 2021;21(1):192. https://doi.org/10.1186/s12902-021-00856-w.
Monteiro-Soares M, Russell D, Boyko EJ, Jeffcoate W, Mills JL, Morbach S, Game F. Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3273. https://doi.org/10.1002/dmrr.3273.
Wilasrusmee C, Suthakorn J, Guerineau C, Itsarachaiyot Y, Sa-Ing V, Proprom N, Lertsithichai P, Jirasisrithum S, Kittur D. A novel robotic monofilament test for diabetic neuropathy. Asian J Surg. 2010;33(4):193–8. https://doi.org/10.1016/s1015-9584(11)60006-7.
Moghaddam MHB, Aghdam F, Asghari Jafarabadi M, Allahverdipour H, Nikookheslat S, Safarpour S. The Iranian version of International Physical Activity Questionnaire (IPAQ) in Iran: content and construct validity, factor structure, internal consistency and stability. World Appl Sci J. 2012;18:1073–80. https://doi.org/10.5829/idosi.wasj.2012.18.08.754.
Pastori D, Carnevale R, Nocella C, Novo M, Santulli M, Cammisotto V, Menichelli D, Pignatelli P, Violi F. Gut-derived serum lipopolysaccharide is associated with enhanced risk of major adverse cardiovascular events in atrial fibrillation: effect of adherence to mediterranean diet. J Am Heart Assoc. 2017;6(6). https://doi.org/10.1161/jaha.117.005784
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE. 2012;7(7):e39504. https://doi.org/10.1371/journal.pone.0039504.
Liu Y, Liu X, Guan H, Zhang S, Zhu Q, Fu X, Chen H, Tang S, Feng Y, Kuang J. Body roundness index is a superior obesity index in predicting diabetes risk among hypertensive patients: a prospective cohort study in China. Front Cardiovasc Med. 2021;8:736073. https://doi.org/10.3389/fcvm.2021.736073.
Dobiásová M. AIP–atherogenic index of plasma as a significant predictor of cardiovascular risk: from research to practice. Vnitr Lek. 2006;52(1):64–71.
Kaneva AM, Bojko ER. Age-adjusted cut-off values of lipid accumulation product (LAP) for predicting hypertension. Sci Rep. 2021;11(1):11095. https://doi.org/10.1038/s41598-021-90648-y.
Toi PL, Anothaisintawee T, Chaikledkaew U, Briones JR, Reutrakul S, Thakkinstian A. Preventive role of diet interventions and dietary factors in type 2 diabetes mellitus: an umbrella review. Nutrients. 2020;12(9):2722. https://doi.org/10.3390/nu12092722.
Chiu S, Bergeron N, Williams PT, Bray GA, Sutherland B, Krauss RM. Comparison of the DASH (Dietary approaches to stop hypertension) diet and a higher-fat DASH diet on blood pressure and lipids and lipoproteins: a randomized controlled trial. Am J Clin Nutr. 2016;103(2):341–7. https://doi.org/10.3945/ajcn.115.123281.
Maddock J, Ziauddeen N, Ambrosini GL, Wong A, Hardy R, Ray S. Adherence to a Dietary approaches to stop hypertension (DASH)-type diet over the life course and associated vascular function: a study based on the MRC 1946 British birth cohort. Br J Nutr. 2018;119(5):581–9. https://doi.org/10.1017/s0007114517003877.
Joyce BT, Wu D, Hou L, Dai Q, Castaneda SF, Gallo LC, Talavera GA, Sotres-Alvarez D, Van Horn L, Beasley JM, Khambaty T, Elfassy T, Zeng D, Mattei J, Corsino L, Daviglus ML. DASH diet and prevalent metabolic syndrome in the hispanic community health study/study of Latinos. Prev Med Rep. 2019;15:100950. https://doi.org/10.1016/j.pmedr.2019.100950
Ghorabi S, Salari-Moghaddam A, Daneshzad E, Sadeghi O, Azadbakht L, Djafarian K. Association between the DASH diet and metabolic syndrome components in Iranian adults. Diabetes Metab Syndr. 2019;13(3):1699–704. https://doi.org/10.1016/j.dsx.2019.03.039.
Soltani S, Shirani F, Chitsazi MJ, Salehi-Abargouei A. The effect of dietary approaches to stop hypertension (DASH) diet on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Obes Rev. 2016;17(5):442–54. https://doi.org/10.1111/obr.12391.
Henning RJ. Type-2 diabetes mellitus and cardiovascular disease. Future Cardiol. 2018;14(6):491–509. https://doi.org/10.2217/fca-2018-0045.
Rubio-Almanza M, Cámara-Gómez R, Merino-Torres JF. Obesity and type 2 diabetes: also linked in therapeutic options. Endocrinol Diabetes Nutr (Engl Ed). 2019;66(3):140–9. https://doi.org/10.1016/j.endinu.2018.08.003.
Mohamadi A, Shiraseb F, Mirzababaei A, AkbarySedigh A, Ghorbani M, Clark CCT, Aali Y, Mirzaei K. The association between adherence to diet quality index and cardiometabolic risk factors in overweight and obese women: a cross-sectional study. Front Public Health. 2023;11:1169398. https://doi.org/10.3389/fpubh.2023.1169398.
Mirzababaei A, Shiraseb F, Abaj F, Khosroshahi RA, Tavakoli A, Koohdani F, Clark CCT, Mirzaei K. The effect of dietary total antioxidant capacity (DTAC) and Caveolin-1 gene variant interaction on cardiovascular risk factors among overweight and obese women: a cross-sectional investigation. Clin Nutr. 2021;40(8):4893–903. https://doi.org/10.1016/j.clnu.2021.07.013.
Agostinis-Sobrinho C, Dias AF, Brand C, Norkiene S, Abreu S, Gaya ACA, Gaya AR, Lopes L, Moreira C, Mota J, Santos R. Adherence to Southern European Atlantic Diet and physical fitness on the atherogenic index of plasma in adolescents. Cad Saude Publica. 2019;35(12):e00200418. https://doi.org/10.1590/0102-311x00200418.
Shahdadian F, Saneei P, Lotfi K, Feizi A, Askari G, Safavi SM. Association of plant-based diets with adropin, atherogenic index of plasma, and metabolic syndrome and its components: a cross-sectional study on adults. Front Nutr. 2023;10:1077709. https://doi.org/10.3389/fnut.2023.1077709.
Edwards MK, Loprinzi PD. Physical activity and diet on atherogenic index of plasma among adults in the United States: mediation considerations by central adiposity. Eur J Clin Nutr. 2018;72(6):826–31. https://doi.org/10.1038/s41430-017-0066-x.
Zalejska-Fiolka J, Hubková B, Birková A, Veliká B, Puchalska B, Kasperczyk S, Błaszczyk U, Fiolka R, Bożek A, Maksym B, Mareková M, Birkner E. Prognostic value of the modified atherogenic index of plasma during body Mass reduction in Polish Obese/Overweight people. Int J Environ Res Public Health. 2018;16(1). https://doi.org/10.3390/ijerph16010068.
Guo R, Li N, Yang R, Liao XY, Zhang Y, Zhu BF, Zhao Q, Chen L, Zhang YG, Lei Y. Effects of the modified DASH Diet on adults with elevated blood pressure or hypertension: a systematic review and meta-analysis. Front Nutr. 2021;8. https://doi.org/10.3389/fnut.2021.725020.
Liese AD, Bortsov A, Günther AL, Dabelea D, Reynolds K, Standiford DA, Liu L, Williams DE, Mayer-Davis EJ, D’Agostino RB Jr, Bell R, Marcovina S. Association of DASH diet with cardiovascular risk factors in youth with diabetes mellitus: the SEARCH for diabetes in Youth study. Circulation. 2011;123(13):1410–7. https://doi.org/10.1161/circulationaha.110.955922.
Gholami F, Martami F, Ghorbaninezhad P, Mirrafiei A, Ebaditabar M, Davarzani S, Babaei N, Djafarian K, Shab-Bidar S. Association of low-carbohydrate diet score and carbohydrate quality with visceral adiposity and lipid accumulation product. Br J Nutr. 2023;129(5):843–53. https://doi.org/10.1017/s000711452200143x.
Kane JP, Pullinger CR, Goldfine ID, Malloy MJ. Dyslipidemia and Diabetes Mellitus: role of lipoprotein species and interrelated pathways of lipid metabolism in diabetes mellitus. Curr Opin Pharmacol. 2021;61:21–7. https://doi.org/10.1016/j.coph.2021.08.013.
Bahiru E, Hsiao R, Phillipson D, Watson KE. Mechanisms and treatment of dyslipidemia in diabetes. Curr Cardiol Rep. 2021;23(4):26. https://doi.org/10.1007/s11886-021-01455-w.
Zeinalabedini M, Nasli-Esfahani E, Esmaillzadeh A, Azadbakht L. How is healthy eating index-2015 related to risk factors for cardiovascular disease in patients with type 2 diabetes. Front Nutr. 2023;10:1201010. https://doi.org/10.3389/fnut.2023.1201010.
Boghossian NS, Yeung EH, Mumford SL, Zhang C, Gaskins AJ, Wactawski-Wende J, Schisterman EF. Adherence to the Mediterranean diet and body fat distribution in reproductive aged women. Eur J Clin Nutr. 2013;67(3):289–94. https://doi.org/10.1038/ejcn.2013.4.
Patel P, Abate N. Body fat distribution and insulin resistance. Nutrients. 2013;5(6):2019–27. https://doi.org/10.3390/nu5062019.
Burhans MS, Hagman DK, Kuzma JN, Schmidt KA, Kratz M. Contribution of adipose tissue inflammation to the development of type 2 diabetes Mellitus. Compr Physiol. 2018;9(1):1–58. https://doi.org/10.1002/cphy.c170040.
Armstrong DG, Tan TW, Boulton AJM, Bus SA. Diabetic foot ulcers: A review. JAMA. 2023;330(1):62–75. https://doi.org/10.1001/jama.2023.10578.
Blanchette V, Brousseau-Foley M. Multidisciplinary management of diabetic foot ulcer infection. Rev Med Interne. 2021;42(3):193–201. https://doi.org/10.1016/j.revmed.2020.09.004.
Stein J, Geisel J, Obeid R. Association between neuropathy and B-vitamins: a systematic review and meta-analysis. Eur J Neurol. 2021;28(6):2054–64. https://doi.org/10.1111/ene.14786.
Pratama S, Lauren BC, Wisnu W. The efficacy of vitamin B(12) supplementation for treating vitamin B(12) deficiency and peripheral neuropathy in metformin-treated type 2 diabetes mellitus patients: a systematic review. Diabetes Metab Syndr. 2022;16(10):102634. https://doi.org/10.1016/j.dsx.2022.102634.
Didangelos T, Karlafti E, Kotzakioulafi E, Margariti E, Giannoulaki P, Batanis G, Tesfaye S, Kantartzis K. Vitamin B12 supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, placebo-controlled trial. Nutrients. 2021;13(2):395. https://doi.org/10.3390/nu13020395.
Sajid N, Miyan Z, Zaidi SIH, Jaffri SSA, AbdeAli M. Protein requirement and its intake in subjects with diabetic foot ulcers at a tertiary care hospital. Pak J Med Sci. 2018;34(4):886–90. https://doi.org/10.12669/pjms.344.15399.
Lauwers P, Dirinck E, Van Bouwel S, Verrijken A, Van Dessel K, Van Gils C, Sels M, Peiffer F, Van Schil P, De Block C, Hendriks J. Malnutrition and its relation with diabetic foot ulcer severity and outcome: a review. Acta Clin Belg. 2022;77(1):79–85. https://doi.org/10.1080/17843286.2020.1800315.
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, Deery HG, Embil JM, Joseph WS, Karchmer AW, Pinzur MS, Senneville E. Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):e132-173. https://doi.org/10.1093/cid/cis346.
Moore ZE, Corcoran MA, Patton D. Nutritional interventions for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev. 2020;7(7):Cd011378. https://doi.org/10.1002/14651858.CD011378.pub2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Human Ethics Committee of Tehran University of Medical Sciences approved the study protocol [IR.TUMS.EMRI.REC.1401.072]. All participants completed written consent forms confirming that they understood and agreed to participate.
Competing interests
The authors have no financial or non-financial interests directly or indirectly related to the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jalalzadeh, M., Nasli-Esfahani, E., Montazer, M. et al. Association between DASH and novel atherogenic risk factors, anthropometric indices and foot ulcer indicators in type 2 diabetic patients with foot ulcer: a cross-sectional study. J Diabetes Metab Disord (2024). https://doi.org/10.1007/s40200-024-01427-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-024-01427-1