Abstract
Background
Diabetes mellitus can cause several long-term macrovascular and microvascular complications including nephropathy, neuropathy, and retinopathy (DR). Several studies have reported positive associations between eating pathologies and DR; however, these studies have not been aggregated and sub-grouped into type of pathological eating behaviour, and the differences in risk according to type of eating behaviour is unknown. The aim of this review, therefore, was to aggregate risks of DR in populations with and without pathological eating behaviours, stratified according to eating behaviour.
Methods
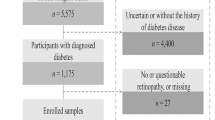
A systematic review and meta-analysis was conducted. Major databases and grey literature were search from inception until 1/6/2021. Studies reporting the prevalence of pathological eating behaviours (against a control group with no pathological eating behaviours) in diabetic people with and without DR were included. Odds ratios were calculated from primary data.
Results
Seven studies with eight independent outcomes with a total of 1162 participants were included. The odds ratio of DR in the total pooled analysis was 2.94 (95%CI 1.86–4.64; p = <0.001; I2 = 29.59). Two types of eating behaviour yielded enough data for sub-group analysis. Eating disorder not otherwise specified yielded an odds ratio of 2.73 (95%CI 1.81–4.10; p = <0.001; I2 = 0.00), and binge eating disorder yielded an non-significant odds ratio of 0.92 (95%CI 0.31–2.77; p = 0.887;I2 = 0.00).
Discussion
The likelihood of DR increases almost three times in the presence of pathological eating behaviours. More studies are required to confirm this in clinical populations stratified by eating disorder. Practitioners working with people with diabetes should closely monitor eating behaviours to preclude this risk.



Similar content being viewed by others
Data availability
All data from this study are available from pre-published papers.
References
diabetes.co.uk. Dry mouth and diabetes. 2020. https://www.diabetes.co.uk/diabetes-complications/dry-mouth.html. Accessed 28 Jul 2020.
Hirai FE, Tielsch JM, Klein BE, Klein R. Ten-year change in vision-related quality of life in type 1 diabetes: Wisconsin epidemiologic study of diabetic retinopathy. Ophthalmology. 2011;118:353–8.
Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013;93:137–88. https://doi.org/10.1152/physrev.00045.2011.
Mathur R, Bhaskaran K, Edwards E, et al. Population trends in the 10-year incidence and prevalence of diabetic retinopathy in the UK: a cohort study in the clinical practice research datalink 2004–2014. BMJ Open. 2017;7:e014444. https://doi.org/10.1136/bmjopen-2016-014444.
Ren C, Liu W, Li J, et al. Physical activity and risk of diabetic retinopathy: a systematic review and meta-analysis. Acta Diabetol. 2019;56:823–37.
Kim TK, Won JY, Shin JA, et al. The association of metabolic syndrome with diabetic retinopathy: the Korean national health and nutrition examination survey 2008–2012. PLoS One. 2016;11:e0157006.
Tapp RJ, Shaw JE, Harper CA, et al. The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care. 2003;26:1731–7.
Zhang X, Saaddine JB, Chou C-F, et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. Jama. 2010;304:649–56.
Kostev K, Rathmann W. Diabetic retinopathy at diagnosis of type 2 diabetes in the UK: a database analysis. Diabetologia. 2013;56:109–11.
Nicolau J, Romerosa JM, Rodríguez I, et al. Associations of food addiction with metabolic control, medical complications and depression among patients with type 2 diabetes. Acta Diabetol. 2020;57:1093–100.
Takii M, Uchigata Y, Nozaki T, et al. Classification of type 1 diabetic females with bulimia nervosa into subgroups according to purging behavior. Diabetes Care. 2002;25:1571–5.
Rodin G, Olmsted MP, Rydall AC, et al. Eating disorders in young women with type 1 diabetes mellitus. J Psychosom Res. 2002;53:943–9.
American Psychiatric Association. DSM-V. 2013.
Nielsen S. Eating disorders in females with type 1 diabetes: an update of a meta-analysis. Eur Eating Disord Rev. 2002;10:241–54.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Joanna Briggs Institute Checklist for Cohort Studies. https://jbi.global/sites/default/files/2021-03/Checklist_for_Cohort_Studies.docx. Accessed 24 Jun 2021.
Joanna Briggs Institute Checklist for Case Control Studies. https://jbi.global/sites/default/files/2021-03/Checklist_for_Case_Control_Studies.docx. Accessed 24 Jun 2021.
Joanna Briggs Institute Checklist for Analytical Cross Sectional Studies. https://jbi.global/sites/default/files/2021-03/Checklist_for_Analytical_Cross_Sectional_Studies.docx. Accessed 24 Jun 2021.
Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive Meta analysis. Englewood, NJ: Biostat; 2013.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta analysis detected by a simple, graphical test. BMJ. Br Med J. 1997; https://doi.org/10.1136/bmj.315.7109.629.
Sterne JA, Egger M, Moher D (2008) Addressing reporting biases. Cochrane handbook for systematic reviews of interventions: Cochrane book series 297–333.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336:924–6.
Rydall AC, Rodin GM, Olmsted MP, et al. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. N Engl J Med. 1997;336:1849–54.
Cantwell R, Steel JM. Screening for eating disorders in diabetes mellitus. J Psychosom Res. 1996;40:15–20.
Nicolau J, Simó R, Sanchís P, et al. Eating disorders are frequent among type 2 diabetic patients and are associated with worse metabolic and psychological outcomes: results from a cross-sectional study in primary and secondary care settings. Acta Diabetol. 2015;52:1037–44.
Polonsky WH, Anderson BJ, Lohrer PA, et al. Insulin omission in women with IDDM. Diabetes Care. 1994;17:1178–85.
Colas C. Eating disorders and retinal lesions in type 1 (insulin-dependent) diabetic women. Diabetologia. 1991;34:288–8.
Takii M, Komaki G, Uchigata Y, et al. Differences between bulimia nervosa and binge-eating disorder in females with type 1 diabetes: the important role of insulin omission. J Psychosom Res. 1999;47:221–31.
Goldstein DE, Blinder KJ, Ide CH, et al. Glycemic control and development of retinopathy in youth-onset insulin-dependent diabetes mellitus: results of a 12-year longitudinal study. Ophthalmology. 1993;100:1125–32. https://doi.org/10.1016/S0161-6420(93)31516-2.
Henricsson M, Nilsson A, Janzon L, Groop L. The effect of glycaemic control and the introduction of insulin therapy on retinopathy in non-insulin-dependent diabetes mellitus. Diabet Med. 1997;14:123–31.
Çelik S, Kayar Y, Önem Akçakaya R, et al. Correlation of binge eating disorder with level of depression and glycemic control in type 2 diabetes mellitus patients. Gen Hosp Psychiatry. 2015;37:116–9. https://doi.org/10.1016/j.genhosppsych.2014.11.012.
Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethics approval
As this was a review on already published papers, no ethical approval was required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 107 kb)
Rights and permissions
About this article
Cite this article
Trott, M., Driscoll, R., Iraldo, E. et al. Pathological eating behaviours and risk of retinopathy in diabetes: a systematic review and meta-analysis. J Diabetes Metab Disord 21, 1047–1054 (2022). https://doi.org/10.1007/s40200-022-00980-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-00980-x