Abstract
Objective
The burden of diabetes is increasing rapidly in Turkey; however, there is insufficient information regarding the interrelated factors of diabetes. This study aims to fill this gap by investigating associated characteristics and self-care behaviors of patients with diabetes.
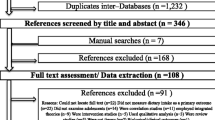
Methods
Path analysis was used to test interrelated factors of diabetes. Data were obtained from a cross-sectional, population-based study (Turkey Health Survey) from 2014. The determined sample size was 9,740 households, and 26,075 individuals were interviewed. There were 19,129 persons who reported having diabetes. Age and gender characteristics and disease-related self-care behaviors of individuals were collected through a self-reported questionnaire. Goodness-of-fit indices were used to assess model fit.
Results
The results demonstrated that patient characteristics, self-care behaviors, and diabetes are causally interrelated (p < 0.0001). Blood glucose monitoring mediated the interrelationships between patient demographic characteristics and diabetes. The model fit indices indicated a good fit of the path model to the data (goodness-of-fit index = 0.96; comparative fit index = 0.89; incremental fit index = 0.89; normed fit index = 0.89). The fight against the increasing prevalence of diabetes mandates enhancing self-care behaviors of individuals with diabetes, including regular blood glucose monitoring and the inculcation of healthy dietary habits.
Conclusions
The results can guide health policy makers to promote patient-centered management of diabetes in the age of the escalating burden of this disease.



Similar content being viewed by others
References
Misra A, Gopalan H, Jayawardena R, Hills AP, Soares M, Reza-Albarrán AA, Ramaiya KL. Diabetes in developing countries. J Diabetes. 2019;11:522–39.
Organisation for Economic Co-operation and Development (OECD). Diabetes prevalence, in health at a glance 2017: OECD Indicators, OECD Publishing. Paris. 2017. https://doi.org/10.1787/health_glance-2017-15-en. Accessed 3 June 2021.
International Diabetes Federation (IDF) (Atlas). http://www.diabetesatlas.org/across-the-globe.html. 2019. Accessed 22 Mar 2019.
Satman I, Yilmaz T, Sengül A, Salman S, Salman F, Uygur S, Bastar I, Tütüncü Y, Sargin M, Dinççag N, Karsidag K, Kalaça S, Ozcan C, King H. Population-based study of diabetes and risk characteristics in Turkey: results of the Turkish diabetes epidemiology study (TURDEP). Diabetes Care. 2002;25:1551–6.
Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, Karsidag K, Genc S, Telci A, Canbaz B, Turker F, Yilmaz T, Cakir B, Tuomilehto J. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169–80.
Organisation for Economic Co-operation and Development (OECD)/European Union “Diabetes prevalence”, in Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris/European Union, Brussels. 2018. https://doi.org/10.1787/health_glance_eur-2018-18-en. Accessed 13 June 2021.
Sözmen K, Unal B, Capewell S, Critchley J, O’Flaherty M. Estimating diabetes prevalence in Turkey in 2025 with and without possible interventions to reduce obesity and smoking prevalence, using a modelling approach. Int J Public Health. 2015;60:13–21.
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–49.
Bullard T, Ji M, An R, Trinh L, Mackenzie M, Mullen SP. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: cancer, cardiovascular disease, and diabetes. BMC Public Health. 2019;19:1–11.
Lange S, Vollmer S. The effect of economic development on population health: a review of the empirical evidence. Br Med Bull. 2017;121:47–60.
Popkin BM, Reardon T. Obesity and food system transition in Latin America. Obes Rev. 2018;19:1028–64.
Atun R, Davies JI, Gale EAM, Bärnighausen T, Beran D, Kengne A, et al. Diabetes in Sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrionol. 2017;5:622–67.
Gulati S, Misra A. Abnormal obesity and type 2 diabetes in Asian Indians: dietary strategies including edible oils, cooking practices and sugar intake. Eur J Clin Nutr. 2017;71:850–7.
Acemoglu S, Ucer M. The ups and downs of Turkish growth, 2002–2015: political dynamics, the European union and the institutional slide. 2015. The National Bureau of Economic Research. http://www.nber.org/papers/w21608. Accessed 10 June 2021.
Uner MM, Gungordu A. The new middle class in Turkey: A qualitative study in a dynamic economy. Int Bus Rev. 2016;25:668–78.
Chambers D, Phan UTX, Chanadang S, Maughan C, Sanchez K, Di Donfrancesco B, Gomez D, Higa F, Li H, Chambers E, Esen E. Motivations for food consumption during specific eating occasions in Turkey. Food. 2016;5:1–14.
Akbay C, Tiryaki GY, Gul A. Consumer characteristics influencing fast food consumption in Turkey. Food Control. 2007;18:904–13.
Erem C, Arslan C, Hacihasanoglu A, Deger O, Topbas M, Ukinc K, Ersöz HO, Telatar M. Prevalence of obesity and associated risk factors in a Turkish population. Obes Res. 2004;12:1117–27.
Aga FB, Dunbar SB, Kebede T, Higgins MK, Gary RA. Correlates of self-care behaviors in adults with Type 2 diabetes and comorbid heart failure. Diabetes Educ. 2019;45:380–96.
RobatSarpooshi D, Mahdizadeh M, Siuki HA, Haddadi M, Robatsarpooshi H, Peyman N. The relationship between health literacy level and self-care behaviors in patients with diabetes. Patient Relat Outcome Meas. 2020;11:129–35.
Mirahmadizadeh A, Khorshidsavar H, Seif M, Sharifi MH. Adherence to medication, diet and physical activity and the associated factors amongst patients with type 2 diabetes. Diabetes Ther. 2020;11:479–94.
Maleki Chollou K, Gaffari-Fam S, Babazadeh T, Daemi A, Bahadori A, Heidari S. The association of health literacy level with self-care behaviors and glycemic control in a low education population with type 2 diabetes mellitus: a cross-sectional study in Iran. Diabet Metab Synd Ob. 2020;13:1685–93.
Turkish Statistical Institute (TurkStat)-Turkey Health Survey (THS). 2014. http://www.turkstat.gov.tr/. Accessed 12 June 2021.
Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE. Understanding the influence of psychological and socioeconomic factors on diabetes self-care using structured equation modeling. Patient Educ Couns. 2015;91:34–40.
Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE. Relationship between social determinants of health and processes and outcomes in adults with type 2 diabetes: validation of a conceptual framework. BMC Endoc Disord. 2014;14:1–10.
Gao J, Wang J, Zhu Y, Yu J. Validation of an information–motivation–behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013;13:1–6.
Min D, Cho E. Associations among health behaviors, body mass index, hypertension, and diabetes mellitus. A path analysis. Medicine. 2018;97:e10981.
Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. EJBRM. 2008;6:53–60.
Babaniamansour S, Aliniagerdroudbari E, Niroomand M. Glycemic control and associated factors among Iranian population with type 2 diabetes mellitus: a cross-sectional study. J Diabetes Metab Disord. 2020;19:933–40.
Pokhrel S, Shrestha S, Timilsina A, Sapkota M, Bhatt MP, Pardhe BD. Self-care adherence and barriers to good Glycaemic control in Nepalese type 2 diabetes mellitus patients: a hospital-based cross sectional study. J Multidiscip Healthc. 2019;12:817–26.
Ahmad NAA, Sallehuddin MAA, Teo YC, Rahman HA. Self-care management of patients with diabetes: nurses’ perspectives. J Diabetes Metab Disord. 2020;19:1537–42.
Ruedy KJ, Parkin CG, Riddlesworth TD, Graham C. Continuous glucose monitoring in older adults with Type 1 and Type 2 diabetes using multiple daily injections of ınsulin: results from the DIAMOND Trial. J Diabetes Sci Technol. 2017;11(6):1138–46.
Moström P, Ahlen E. Imberg H, Hansson PO, Lind M. Adherence of self-monitoring of blood glucose in persons with type 1 diabetes in Sweden. BMJ Open Diabetes Res Care. 2017;5:000342.
Shakeel PM, Baskar S, Dhulipala VRS, Jaber MM. Cloud based framework for diagnosis of diabetes mellitus using k-means clustering. Health Inf Sci Syst. 2018;6(16):1–7.
Kime, N., Pringle, A., Zwolinsky, S., Vishnubala D. How prepared are healthcare professionals for delivering physical activity guidance to those with diabetes? A formative evaluation. BMC Health Serv Res. 2020;20(8). https://doi.org/10.1186/s12913-019-4852-0.
Thorne SE, Paterson BL. Health care professional support for self-care management in chronic illness: Insights from diabetes research. Patient Educ Couns. 2001;42:81–90.
OECD Health data. Health at a galance. 2019. https://data.oecd.org/healthres/doctors.htm. Accessed 12 June 2021.
Hatun S, Yesiltepe Mutlu G, Cinaz P, et al. Characteristics of Turkish children with Type 2 diabetes at onset: a multicentre, cross-sectional study. Diabetic Med. 2019;36:1243–50.
Iturralde E, Chi FW, Grant RW, et al. Association of anxiety with high-cost health care use among individuals with type 2 diabetes. Diabetes Care. 2019;42:1669–74.
Top M, Aslan H, Akyürek ÇE, Aslan EÇ. Costs analysis of diabetes mellitus: A study based on hospital invoices and diagnosis related groups. Health Policy Techn. 2020;9(1):23–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest related to this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cinaroglu, S. Associated patient demographic characteristics and disease-related self-care behaviors with diabetes: a mediation model. J Diabetes Metab Disord 20, 1301–1308 (2021). https://doi.org/10.1007/s40200-021-00856-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00856-6