Abstract
Purpose
Designing mobile-based applications is one of the tools to raise the awareness of patients and the care team. Aim of this study is to identify the data elements of a mobile-based application to overweight and obesity management for children and adolescents from the experts’ point of view.
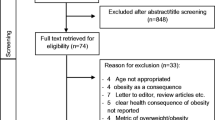
Methods
In this descriptive-analytical article, data collection was conducted through library and Internet research. The research population comprised 30 nutritionists selected via simple sampling method. The research instrument was a questionnaire developed by the researcher in four sections: demographic data, assessment data, therapeutic recommendations and application capabilities. Validity and reliability were confirmed by Content Validity Ratio (CVR) and Delphi method respectively.
Results
The Minimum Data Set (MDS) required for overweight and obesity management in children and adolescents was designed based on the data from the guidelines of the United States, Canada, Australia, Britain, Iran, and experts' opinions. The importance of this MDS suggested was calculated based on the percentage points given by experts for the demographic data of 100%, the assessment data of 88.33%, the therapeutic recommendations of 97.67%, and the application capabilities of 88.94%.
Conclusion
Identifying prevention and control minimum data set of overweight and obesity in children and adolescents from the point of view of experts will be effective in improving the applications in this field. This MDS has two parts of data elements: the first for recognition of the framework of evaluating and applying therapeutic methods that can empower parents to manage the child's body mass and the second as a patient's personal record for storage a set of data that can be used by nutritionists in visits to healthcare centers.

Similar content being viewed by others
Abbreviations
- MDS:
-
Minimum Data Set
- CVR:
-
Content Validity Ratio
- CVI:
-
Content Validity Index
- CDC:
-
Centers for Disease Control
- AAP:
-
American Academy of Pediatrics
- WHO:
-
World Health Organization
- ICSI:
-
Institute for Clinical Systems Improvement
- NHS:
-
National Health Service
- MVPA:
-
Moderate-to-vigorous intensity physical activity
- MET:
-
Metabolic equivalent of task
References
Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS. Healthier options for public schoolchildren program improves weight and blood pressure in 6-to 13-year-olds. J Am Diet Assoc. 2010. https://doi.org/10.1016/j.jada.2009.10.029.
Razavi N, Mahjouri M, Arzaghi M. Behavioral therapy in obesity. J Diabetes Metab Iran. 2013;12(5):467–77.
Gregory JW. Prevention of obesity and metabolic syndrome in children. Front Endocrinol (Lausanne). 2019;1(10):669. https://doi.org/10.3389/fendo.2019.00669 (eCollection 2019).
Malik VS, Ravindra K, Attri SV, Bhadada SK, Singh M. Higher body mass index is an important risk factor in COVID-19 patients: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2020. https://doi.org/10.1007/s11356-020-10132-4.
Sá-Caputo DC, Paineiras-Domingos LL, Oliveira R, Neves MFT, Brandão A, Marin PJ, Sañudo B, Furness T, Taiar R, Bernardo-Filho M. Acute effects of whole-body vibration on the pain level, flexibility, and cardiovascular responses in individuals with metabolic syndrome. Dose Response. 2018;16(4):1559325818802139. https://doi.org/10.1177/1559325818802139.
Caprio S, Santoro N, Weiss R. Childhood obesity and the associated rise in cardiometabolic complications. Nat Metab. 2020;2(3):223–32. https://doi.org/10.1038/s42255-020-0183-z.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. https://doi.org/10.1016/S0140-6736(14)60460-8.
Akbari N, Tavakol K, Parvin N, Delaram M, Kazemiyan A. Comparative survey of parents’ BMI in obese and non-obese 6–12-year-old children in Esfahan. J Holist Nurs Midwifery. 2000;15(2):1–6.
Mirsolimany H, Mokhtari N, Mirhadiyan L, Kazemnejad E. Survey predictors of overweight and obesity in children beginning. J Holist Nurs Midwifery. 2015;25(3):55–62.
Saperstein SL, Atkinson NL, Gold RS. The impact of internet use for weight loss. Obes Rev. 2007. https://doi.org/10.1111/j.1467-789X.2007.00374.x.
Pasdar Y, Moridi S, Najafi F, Niazi P, Heidary M. The effect of nutritional intervention and physical activities on weight reduction. J Kermanshah Univ Med Sci. 2012;15(6):427–34.
Mehraeen E, Safdari R, SeyedAlinaghi S, Mohammadzadeh N, Mohraz M. Common elements and features of a mobile-based self-management system for people living with HIV. Electron Phys. 2018; 10(4):6655-6662. https://doi.org/10.19082/6655.
Nguyen B, Kornman KP, Baur LA. A review of electronic interventions for prevention and treatment of overweight and obesity in young people. Obes Rev. 2011. https://doi.org/10.1111/j.1467-789X.2010.00830.x.
Hammersley ML, Jones RA, Okely AD. Parent-focused childhood and adolescent overweight and obesity eHealth interventions: a systematic review and meta-analysis. J Med Internet Res. 2016. https://doi.org/10.2196/jmir.5893.
Barton AJ. The regulation of mobile health applications. BMC Med. 2012; https://doi.org/10.1186/1741-7015-10-46.
Kurdi HA, Alkhowaiter A, Al-Muaibed A, Alotaibi B, Alhaweal R, Alotaibi T. MyPDA: a mobile healthcare application for personal diet assisting. 2012 International Conference on Advanced Computer Science Applications and Technologies (ACSAT) IEEE. 2012; https://doi.org/10.1109/ACSAT.2012.17.
Alnasser AA, Amalraj RE, Sathiaseelan A, Al-khalifa AS, Marais D. Do Arabic weight-loss apps adhere to evidence-informed practices? Transl Behav Med. 2016;6(3):396–402. https://doi.org/10.1007/s13142-015-0347-7.
Santoro E, Castelnuovo G, Zoppis I, Mauri G, Sicurello F. Social media and mobile applications in chronic disease prevention and management. Front Psych. 2015; https://doi.org/10.3389/fpsyg.2015.00567.
Podina IR, Fodor LA, Cosmoiu A, Boian R. An evidence-based gamified mHealth intervention for overweight young adults with maladaptive eating habits: study protocol for a randomized controlled trial. Trials. 2017; https://doi.org/10.1186/s13063-017-2340-6.
Bhardwaj NN, Wodajo B, Gochipathala K, Paul DP, Coustasse A. Can mHealth revolutionize the way we manage adult obesity? Perspectives in Health Information Management. 2017; 14(Spring):1a. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5430129/. Accessed 27 Aug 2019.
Kazemi-Arpanahi H, Vasheghani-Farahani A, Baradaran A, Mohammadzadeh N, Ghazisaeedi M. Developing a Minimum Data Set (MDS) for cardiac electronic implantable devices implantation. J Acad Med Sci Bosnia Herzegovina. 2018; https://doi.org/10.5455/aim.2018.26.164-168.
Sheykhotayefeh M, Safdari R, Ghazisaeedi M, Khademi SH, Seyed Farajolah SS, Maserat E, et al. Development of a Minimum Data Set (MDS) for C-section Anesthesia Information Management System (AIMS). Anesthesiol Pain Med. 2016;7(2):e44132. https://doi.org/10.5812/aapm.44132.
Ahmadi M, Alipour J, Mohammadi A, Khorami F. Development a minimum data set of the information management system for burns. J Intl Soc Burn Injur. 2015; https://doi.org/10.1016/j.burns.2014.12.009.
Staiano AE, Gonugunta N, Drazba KT, Marker A. Childhood obesity treatment: obesity reduction strategic initiative. Baptist community ministries & pennington biomedical research center. 2014. https://www.pbrc.edu/obesitytoolkit/. Accessed 27 Aug 2019.
Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. National Health and Medical Research Council. 2013. https://www.nhmrc.gov.au/about-us/publications/clinical-practice-guidelines-management-overweight-and-obesity. Accessed 27 Aug 2019.
Centre for Public Health Excellence at NICE (UK); National Collaborating Centre for Primary Care (UK). Obesity: The prevention, identification, assessment and management of overweight and obesity in adults and children [Internet]. London: National Institute for Health and Clinical Excellence (UK); 2006. https://www.ncbi.nlm.nih.gov/pubmed/22497033. Accessed 27 Aug 2019.
Fitch A, Fox C, Bauerly K, Gross A, Heim C, Judge-Dietz J, Kaufman T, et al. Prevention and management of obesity for children and adolescents. Institute for Clinical Systems Improvement (ICSI). 2013. https://www.ncbi.nlm.nih.gov/nlmcatalog/101670425. Accessed 27 Aug 2019.
Management of Obesity, A National Clinical Guideline. Scottish Intercollegiate Guidelines Network(SIGN), Management of Obesity Guideline Development Group. 2010. https://www.sign.ac.uk/assets/sign115.pdf. Accessed 27 Aug 2019.
Waltz CF, Bausell RB. Nursing research: design, statistics, and computer analysis. Illustrated ed. Philadelphia: F.A. Davis Co; 1981.
Lawshe CH. A quantitative approach to content validity. Personnel Psychol. 1975; https://doi.org/10.1111/j.1744-6570.1975.tb01393.x.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. https://doi.org/10.1007/BF02310555.
Raj M, Kumar RK. Obesity in children & adolescents. Indian J Med Res. 2010;132(5):598–607.
Papandreou D, Malindretos P, Rousso I. Risk factors for childhood obesity in a Greek paediatric population. Publ Health Nutr. 2010; https://doi.org/10.1017/S1368980009993156.
Vanhala M, Korpelainen R, Tapanainen P, Kaikkonen K, Kaikkonen H, Saukkonen T, et al. Lifestyle risk factors for obesity in 7- year- old children. Obes Res Clin Pract. 2009; https://doi.org/10.1016/j.orcp.2009.01.003.
Lee EY, Yoon KH. Epidemic obesity in children and adolescents: risk factors and prevention. Front Med. 2018;12:658–66. https://doi.org/10.1007/s11684-018-0640-1.
Yen CF, Hsiao RC, Ko CH, Yen JY, Huang CF, Liu SC, et al. The relationships between body mass index and television viewing, internet use and cellular phone use: the moderating effects of socio-demographic characteristics and exercise. Int J Eat Disord. 2010;43:565–71. https://doi.org/10.1002/eat.20683.
Arluk SL, Branch JD, Swain DP, Dowling EA. Childhood obesity’s relationship to time spent in sedentary behavior. Mil Med. 2003;168:583–6. https://doi.org/10.1093/milmed/168.7.583.
Vicente-Rodríguez G, Rey-López JP, Martín-Matillas M, Moreno LA, Wärnberg J, Redondo C, et al. Television watching, videogames, and excess of body fat in Spanish adolescents: the AVENA study. Nutrition. 2008;24:654–62. https://doi.org/10.1016/j.nut.2008.03.011.
Akhavan S, Fallah R, Golestan M, Sadr M. Prevalence and risk factors of obesity and overweight among primary school children in Yazd. J Shahid Sadoughi Univ Med Sci. 2009;16(5):8–13.
Mitchell JA, Pate RR, Beets MW, Nader PR. Time spent in sedentary behavior and changes in childhood BMI: a longitudinal study from ages 9 to 15 years. Int J Obes (Lond). 2013;37(1):54–60. https://doi.org/10.1038/ijo.2012.41.
Raistenskis J, Sidlauskiene A, Strukcinskiene B, Uğur Baysal S, Buckus R. Physical activity and physical fitness in obese, overweight, and normal-weight children. Turk J Med Sci. 2016;46(2):443–50. https://doi.org/10.3906/sag-1411-119.
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008; https://doi.org/10.1093/sleep/31.5.619.
Alborzimanesh M, Kimiagar M, Rashidkhani B, Atefi- SS. The relation between overweight and obesity with some lifestyle factors in the 3rd – 5th-grade primary schoolgirls in Tehran city 6th district. Iran J NutrSci Food Technol. 2011;6(3):75–84.
Fornari E, Maffeis C. Treatment of metabolic syndrome in children. Front Endocrinol (Lausanne). 2019;15(10):702. https://doi.org/10.3389/fendo.2019.00702.
Kelishadi RHM, Sadeghi M, Roohafza H, Tavasoli A, Khosravi A, Ansari R, Ansari Z, Bashardoust N. The impact of familial factors on obesity in Iranian children and adolescents. J Pediatr Neonatal. 2005;2(2):16–23.
Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, Kazak A. Influence of stress in parents on child obesity and related behaviors. Pediatrics. 2012;130(5):e1096–104.
von Philipsborn P, Stratil JM, Burns J, Busert LK, Pfadenhauer LM, Polus S, et al. Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. Cochrane Database Syst Rev. 2019; 6:CD012292. https://doi.org/10.1002/14651858.CD012292.pub2.
Hemmingsson E. A new model of the role of psychological and emotional distress in promoting obesity: conceptual review with implications for treatment and prevention. Obes Rev. 2014;15:769–79. https://doi.org/10.1111/obr.12197.
Specchia ML, Barbara A, Campanella P, Parente P, Mogini V, Ricciardi W, et al. Highly-integrated programs for the prevention of obesity and overweight in children and adolescents: results from a systematic review and meta-analysis. Ann Ist Super Sanita. 2018;54:332–9. https://doi.org/10.4415/ANN_18_04_10.
Psaltopoulou T, Tzanninis S, Ntanasis-Stathopoulos I, Panotopoulos G, Kostopoulou M, Tzanninis IG, et al. Prevention and treatment of childhood and adolescent obesity: a systematic review of meta-analyses. World J Pediatr. 2019;30:3–12. https://doi.org/10.1007/s12519-019-00266.
Magge SN, Goodman E, Armstrong SC, Committee on nutrition, section on endocrinology, section on obesity. The metabolic syndrome in children and adolescents: shifting the focus to cardiometabolic risk factor clustering. Pediatrics. 2017; 140: e20171603. https://doi.org/10.1542/peds.2017-1603.
Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019; 7:CD001871. https://doi.org/10.1002/s14651858.CD001871.pub4.
Tavasoli E, Nilsaz M, Raiesi M, Javadzadeh H, Mohamadi F, Gharlipour Z, Vafaee R, Mohamadi J. Prevention of overweight and obesity in children and adolescents: a review on the accomplished interventional studies. J Ilam Univ Med Sci. 2013;21(4):83–90.
Acknowledgments
The results described in this paper formed part of a thesis submitted by the first author (EH) for an MSc degree in Health Information Technology at Tehran University of Medical Sciences. The authors extend thanks to professionals working at the Department of Health Information Management and Department of Nutritional Sciences in Tehran University of Medical Sciences.
This research has been supported by Tehran University of Medical Sciences & Health Services grant 98-02-31-41689; with ethical code IR.TUMS.SPH.REC.1397.104.
Author information
Authors and Affiliations
Contributions
EH, LSh, MM and RN participated in the elaboration and execution of the study.EH and SB did the statistical analysis.EH and AR coordinated the study and helped on the draft of manuscript. EH, MM, AR, RN and SB reviewed. EH and LSh approved the final version of this investigation. EH submitted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics code
This study was approved by the Research Ethics Committee of the Iran National Committee for Ethics in Biomedical Research with the number IR.TUMS.SPH.REC.1397.104.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hajizadeh, E., Shahmoradi, L., Mahmoodi, M. et al. Identification of the minimum data set to design a mobile-based application on overweight and obesity management for children and adolescents. J Diabetes Metab Disord 20, 1011–1020 (2021). https://doi.org/10.1007/s40200-021-00807-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00807-1