Abstract
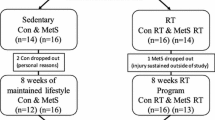
Elevated plasma homocysteine concentration is a risk factor for cardiovascular disease, which seems to be the main cause of increased mortality in patients with type 2 diabetes. Previous studies have demonstrated the effect of exercise on homocysteine levels and the magnitude of these benefits seems to depend on the type, mode and frequency of training. The present study aimed to compare the effects of aerobic and resistance training on plasma homocysteine in individuals with type 2 diabetes. The study included 15 individuals undergoing aerobic training, 14 subjects undergoing resistance training, and 18 individuals in the control group. Homocysteine, total cholesterol and fractions, glucose, and anthropometric measurements were conducted. The training program lasted 16 weeks. Aerobic training was performed twice a week and lasted 75 min, and resistance training was performed twice a week and lasted 75 min. Homocysteine levels were not significantly different between before and after training. High-density lipoprotein levels increased in both training groups and decreased in the control group. Glucose levels decreased after aerobic and resistance training. Body fat mass (percentage and total) decreased in both training group, but with more expression in the aerobic group. We conclude that 16-week aerobic and resistance training programs did not significantly affect plasma homocysteine levels in patients with type 2 diabetes. Nevertheless, these training programs yielded positive results in HDL control, plasma glucose, and body composition.
Similar content being viewed by others
Abbreviations
- HPLC:
-
High-performance liquid chromatography
- VLDL:
-
Very-low-density lipoprotein
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- EDTA:
-
Ethylenediaminetetraacetic acid
- BMI:
-
Body mass index
- 1-RM:
-
1 Maximum repetition
References
Clough GF, Turzyniecka M, Walter L, Krentz AJ, Wild SH, Chipperfield AJ, et al. Muscle microvascular dysfunction in central obesity is related to muscle insulin insensitivity but is not reversed by high-dose statin treatment. Diabetes. 2009;58:1185–91.
Gatti A, Maranghi M, Bacci S, Carallo C, Gnasso A, Mandosi E, et al. Poor glycemic control is an independent risk factor for low HDL cholesterol in patients with type 2 diabetes. Diabetes Care. 2009;32:1550–2.
Martins RA, Veríssimo MT, Silva MJC, Cumming SP, Teixeira AM. Effects of aerobic and strength-based training on metabolic health indicators in older adults. Lipids Health Dis. 2010;9:1–6.
Gabriel R, Saiz C, Susi R, Alonso M, Vega S, López I, et al. Epidemiology of lipid profile of the Spanish elderly population: the EPICARDIAN study. Med Clin. 2004;122:605–9.
Ekelund U, Brage S, Griffin SJ, Wareham NJ. Objectively measured moderate- and vigorous-intensity physical activity but not sedentary time predicts insulin resistance in high-risk individuals. Diabetes Care. 2009;32:1081–6.
King H, Kriska AM. Prevention of type II diabetes by physical training: epidemiological considerations and study methods. Diabetes Care. 1992;15:1794–9.
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the council on clinical cardiology (subcommittee on exercise, rehabilitation, and prevention) and the council on nutrition, physical activity, and metabolism (subcommittee on physical activity). Circulation. 2003;107:3109–16.
Guthikonda S, Haynes WG. Homocysteine: role and implications in atherosclerosis. Curr Atheroscler Rep. 2006;8:100–6.
Rudy A, Kowalska I, Straczkowski M, Kinalska I. Homocysteine concentrations and vascular complications in patients with type 2 diabetes. Diabetes Metab. 2005;31:112–7.
Neves LB, Macedo DM, Lopes AC. Homocisteína. J Bras Patol Med Lab. 2004;40:311–20.
Austin RC, Lentz SR, Werstuck GH. Role of hyperhomocysteinemia in endothelial dysfunction and atherothrombotic disease. Cell Death & Differentiation. 2004;11:S56–64.
Deminice R, Ribeiro DF, Frajacomo FTT. The effects of acute exercise and exercise training on plasma Homocysteine: a MetaAnalysis. PLoS One. 2016;11:1–17.
Maroto-Sánchez B, Lopez-Torrez O, Palacios G, González-Gross M. What do we know about homocysteine and exercise? A review from the literature. Clin Chem Lab Med. 2016;54:1561–77.
Silva AS, Mota MPG. Effects of physical activity and training programs on plasma homocysteine levels: a systematic review. Amino Acids. 2014;46:1795–04.
Silva AS, Lacerda FV, Mota MPG. Efeito do Treinamento Aeróbio nos níveis de homocisteína em indivíduos diabéticos do tipo 2. Rev Bras Med Esporte. 2015;21:275–8.
Molina-López J, Molina JM, Chirosa LJ, Florea DI, Sáez L, Planells E. Effect of folic acid supplementation on homocysteine concentration and association with training in handball players. J Int Soc Sports Nutr. 2013;10:1–8.
Guzel NA, Pinar L, Colakoglu F, Karacan S, Ozer C. Long-term callisthenic exercise–related changes in blood lipids, Homocysteine, nitric oxide levels and body composition in middle-aged healthy sedentary women. Chin J Physiol. 2012;55:202–9.
Sotgia S, Carru C, Caria MA, Tadolini B, Deiana L, Zinellu A. Acute variations in homocysteine levels are related to creatine changes induced by physical activity. Clin Nutr. 2007;26:444–9.
Boreham CAGRA, Murphy KMH, Tully M, Wallace WFM, Young I. Training effects of short bouts of stair climbing on cardiorespiratory fitness, blood lipids, and homocysteine in sedentary young women. Br J Sports Med. 2005;39:590–3.
Randeva HS, Lewandowski KC, Drzewoski J, Brooke-Wavell K, O'Callaghan C, Czupryniak L, et al. Exercise decreases plasma total homocysteine in overweight young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87:4496–501.
Herrmann M, Schorr H, Obeid R, Scharhag J, Urhausen A, Kindermann W, et al. Homocysteine increases during endurance exercise. Clin Chem Lab Med. 2003;41:1518–24.
Silva AS, Lacerda FV, Mota MPG. Effect of strength training on plasma levels of Homocysteine in patients with type 2 diabetes. Int J Prev Med. 2019;10:1–6.
Vincent HK, Bourguignon C, Vincent KR. Resistance training lowers exercise-induced oxidative stress and homocysteine levels in overweight and obese older adults. Obesity. 2006;14:1921–30.
Vincent KR, Braith RW, Bottiglieri T, Vincent HK, Lowenthal DT. Homocysteine and lipoprotein levels following resistance training in older adults. Prev Cardiol. 2003;6:197–203.
Ferin R, Pavão ML, Baptista J. Methodology for a rapid and simultaneous determination of total cysteine, homocysteine, cysteinylglycine and glutathione in plasma by isocratic RP-HPLC. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;911:15–20.
Ichinose S, Nakamura M, Maeda M, Ikeda R, Wada M, Nakazato M, et al. A validated HPLC-fluorescence method with a semi-micro column for routine determination of homocysteine, cysteine and cysteamine, and the relation between the thiol derivatives in normal human plasma. Biomed Chromatogr. 2009;23:935–9.
Sawuta JP, Banecka-Majkutewicz Z, Kadzinski L, Jakóbkiewicz-Banecka J, Wegrzyn G, Nyka W, et al. Improved HPLC method for total plasma homocysteine detection and quantification. Acta Biochim Pol. 2008;55:119–25.
Orsatti FL, Nahas EAP, Nahas-Neto J, Maesta N, Orsatti CL, Fernandes CE. Effects of resistance training and soy Isoflavone on body composition in postmenopausal women. Obstet Gynecol Int. 2010;2010:1–8.
Christos ZE, Tokmakidis SP, Volaklis KA, Kotsa K, Touvra AM, Douda E, et al. Lipoprotein profile, glycemic control and physical fitness after strength and aerobic training in post-menopausal women with type 2 diabetes. Eur J Appl Physiol. 2009;106:901–7.
Rahnama R, Nouri R, Rahmaninia F, Damirchi A, Emami H. The effects of exercise training on maximum aerobic capacity, resting heart rate, blood pressure and anthropometric variables of postmenopausal women with breast cancer. J Res Med Sci. 2010;15:78–83.
Rech CR, Cordeiro BA, Petroski EL, Vasconcelos FAG. Utilização da espessura de dobras cutâneas para a estimativa da gordura corporal em idosos. Rev Nutr. 2010;23:17–26.
Ribeiro AC, Sávio KEO, Rodrigues MLCF, Costa THM, Schmitz BAS. Validação de um questionário de frequência de consumo alimentar para população adulta. Rev Nutr. 2006;19:553–62.
Fisberg RM, Marchioni DML, Colucci ACA. Avaliação do consumo alimentar e da ingestão de nutrientes na prática clínica. Arq Bras Endocrinol Metab. 2009;53:617–24.
Sigal RJ, Kenny GP, Boule NG, Wells GA, Prud'homme D, Fortier M, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. 2007;147:357–71.
Pizzorno J. Homocysteine: Friend or Foe? Integr Med. 2014;13:8–14.
Chen CN, Brown-Borg HM, Rakoczy SG, Ferrington DA, Thompson LV. Aging impairs the expression of the catalytic subunit of glutamate cysteine ligase in soleus muscle under stress. J Gerontol A Biol Sci Med Sci. 2010;65:129–37.
Lee KY, Kim SJ, Cha YS, So JR, Park JS, Kang KS, et al. Effect of exercise on hepatic gene expression in an obese mouse model using cDNA microarrays. Obesity. 2006;14:1294–302.
Vitvitsky V, Mosharov E, Tritt M, Ataullakhanov F, Banerjee R. Redox regulation of homocysteine-dependent glutathione synthesis. Redox Rep. 2003;8:57–63.
Úbeda N, Carson BP, García-González Á, Aguilar-Ros A, Díaz-Martínez ÁE, Venta R, et al. Muscular contraction frequency does not affect plasma homocysteine concentration in response to energy expenditure- and intensity-matched acute exercise in sedentary males. Appl Physiol Nutr Metab. 2018;43:107–12.
Camera DM, Smiles WJ, Hawley JA. Exercise-induced skeletal muscle signaling pathways and human athletic performance. Free Radic Biol Med. 2016;98:131–43.
Raszkowski RR, Welty JD, Peterson MB. The amino acid composition of actin and myosin and Ca2+-activated myosin adenosine Triphosphatase in chronic canine congestive heart failure. Circ Res. 1977;40:191–8.
Schoenfeld BJ. Does exercise-induced muscle damage play a role in skeletal muscle hypertrophy? J Strength Cond Res. 2012;26:1441–53.
Wang Y, Xu D. Effects of aerobic exercise on lipids and lipoproteins. Lipids Health Dis. 2017;16:132.
Williams AD, Almond J, Ahuja KD, Beard DC, Robertson IK, Ball MJ. Cardiovascular and metabolic effects of community based resistance training in an older population. J Sci Med Sport. 2011;14:331–7.
Wycherley TP, Noakes M, Clifton PM, Cleanthous X, Keogh JB, Brinkworth GD. Timing of protein ingestion relative to resistance exercise training does not influence body composition, energy expenditure, glycaemic control or cardiometabolic risk factors in a hypocaloric, high protein diet in patients with type 2 diabetes. Diabetes Obes Metab. 2010;12:1097–105.
Vind BF, Pehmøller C, Treebak JT, Birk JB, Hey-Mogensen M, Beck-Nielsen H, et al. Impaired insulin-induced site-specific phosphorylation of TBC1 domain family, member 4 (TBC1D4) in skeletal muscle of type 2 diabetes patients is restored by endurance exercise-training. Diabetologia. 2011;54:157–67.
Terada T, Friesen A, Chahal BS, Bell GJ, McCargar LJ, Boulé NG. Feasibility and preliminary efficacy of high intensity interval training in type 2 diabetes. Diabetes Res Clin Pract. 2013;99:120–9.
Balducci S, Zanuso S, Cardelli P, Salvi L, Bazuro A, Pugliese L, et al. Effect of high- versus low-intensity supervised aerobic and resistance training on modifiable cardiovascular risk factors in type 2 diabetes. PLoS One. 2012;7:1–9.
Kadoglou NP, Fotiadis G, Athanasiadou Z, Vitta L, Lampropoulos S, Vrabas IS. The effects of resistance training on ApoB/ApoA-I ratio, Lp(a) and inflammatory markers in patients with type 2 diabetes. Endocrine. 2012;42:561–9.
Plotnikoff RC, Eves N, Jung M, Sigal RJ, Padwal R, Karunamuni N. Multicomponent, home-based resistance training for obese adults with type 2 diabetes: a randomized controlled trial. Int J Obes. 2010;34:1733–41.
Nielsen J, Mogensen M, Vind BF, Sahlin K, Højlund K, Schrøder HD, et al. Increased subsarcolemmal lipids in type 2 diabetes: effect of training on localization of lipids, mitochondria, and glycogen in sedentary human skeletal muscle. Am J Physiol Endocrinol Metab. 2010;298:706–13.
Jensen TE, Richter EA. Regulation of glucose and glycogen metabolism during and after exercise. J Physiol. 2012;590:1069–76.
Egan B, Zierath JR. Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metab. 2013;17:162–84.
Pauli JR, Cintra DE, Souza CT, Ropelle ER. Novos mecanismos pelos quais o exercício físico melhora a resistência à insulina no músculo esquelético. Arq Bras Endocrinol Metab. 2009;53:399–408.
Francisqueti FV, Nascimento AF, Corrêa CR. Obesidade, inflamação e complicações metabólicas. Nutrite. 2015;40:81–9.
Funding
This work was financed by National Funds through FCT - Foundation for Science and Technology under the project UID/DTP/04045/2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
e Silva, A.d., Lacerda, F.V. & da Mota, M.P.G. The effect of aerobic vs. resistance training on plasma homocysteine in individuals with type 2 diabetes. J Diabetes Metab Disord 19, 1003–1009 (2020). https://doi.org/10.1007/s40200-020-00596-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-020-00596-z