Abstract
Most diabetes is polygenic in etiology, with (type 1 diabetes, T1DM) or without (type 2 diabetes, T2DM) an autoimmune basis. Genetic counseling for diabetes generally focuses on providing empiric risk information based on family history and/or the effects of maternal hyperglycemia on pregnancy outcome. An estimated one to five percent of diabetes is monogenic in nature, e.g., maturity onset diabetes of the young, with molecular testing and etiology-based treatment available. However, recent studies show that most monogenic diabetes is misdiagnosed as T1DM or T2DM. While efforts are underway to increase the rate of diagnosis in the diabetes clinic, genetic counselors and clinical geneticists are in a prime position to identify monogenic cases through targeted questions during a family history combined with working in conjunction with diabetes professionals to diagnose and assure proper treatment and familial risk assessment for individuals with monogenic diabetes.
Similar content being viewed by others
Introduction
Diabetes mellitus (commonly referred to as “diabetes” but distinguished from the far less common condition of diabetes insipidus) is a group of metabolic disorders characterized by elevated blood sugar levels that results from insulin deficiency, insulin resistance (defect in the body’s ability to use insulin), or a combination of both. Insulin is secreted from the pancreas and enables cells to use glucose for energy. Diabetes is a major cause of morbidity and mortality, with 8.3 % of the US population (25.8 million people) affected as of 2011 [1]. Chronic hyperglycemia can result in damage to different organ systems including the eyes, heart, kidneys, nerves, and blood vessels. Diabetes is the leading cause of kidney failure, non-traumatic lower-limb amputations, and new cases of blindness among adults and is the seventh leading cause of death in the US, killing more than 1.4 million people worldwide in 2011 [2]. Diagnosing and treating diabetes effectively is paramount to preventing complications.
The etiology of diabetes is highly heterogeneous. The American Diabetes Association (ADA) has classified diabetes into four categories: type 1 diabetes mellitus (T1DM), caused by autoimmune destruction of the pancreatic β-cells; type 2 diabetes mellitus (T2DM), itself a highly heterogeneous group of disorders involving insulin resistance combined with relative insulin deficiency; gestational diabetes mellitus (GDM); and other specific types, another heterogeneous group which includes, among others, forms of diabetes resulting from the inheritance of a mutation in a single gene (monogenic diabetes) [3••].
Knowing the etiology is important so that therapy can be tailored, glycemic control obtained, and complications prevented or reduced in severity. Yet there is increasing evidence that subtype misdiagnosis is common, with a recent study published in 2013 showing that 94 % of children and adolescents with the most common forms of monogenic diabetes (maturity onset diabetes of the young, or MODY) were misdiagnosed, mostly as T1DM or T2DM, and 76 % were receiving the wrong treatment [4••].
Additionally and highly relevant here, since nearly all diabetes has a genetic component ranging from monogenic to polygenic, identifying the specific diabetes subtype allows for more precise risk assessment in family members and allows family members to benefit from a more tailored treatment approach. In this review, we provide a brief overview of the types of diabetes, how they are treated, how they are inherited, and what is currently understood about their genetic etiology and its current implications for use of genetic testing. We then propose a multidisciplinary approach to assuring that individuals with diabetes receive the correct genetic diagnosis and treatment.
Background, Etiology and Practical Genetics Issues by ADA Diabetes Category
T1DM, responsible for about 5–10 % of diabetes cases, results from absolute insulin deficiency, most commonly due to an autoimmune process destroying the pancreatic β-cells. Patients are characteristically young and thin, and many present with severe hyperglycemia in diabetic ketoacidosis. Insulin autoantibodies can be detected in the blood of about 85–90 % of individuals [3••]. More recently, it has become apparent that T1DM can have a later and more insidious onset, sometimes known as latent autoimmune diabetes of adulthood (LADA), which may be incorrectly diagnosed initially as T2DM [5]. T1DM was in the past known as insulin-dependent diabetes mellitus (IDDM) or juvenile diabetes, terms that have fallen out of favor in the quest to categorize diabetes by etiology rather than treatment and in recognition of the ability of T1DM to affect adults. Individuals with T1DM ultimately require insulin for treatment because of loss of β-cells and consequent lack of insulin production.
The largest known genetic contributor to T1DM susceptibility is variation at the human leukocyte antigen (HLA) locus, with some haplotypes having odds ratios (OR) as high as 11 [6], followed by over 40 other primarily genome-wide association study (GWAS)-derived loci with effect sizes ranging from 1.09 to 2.38 [7]. Discovery of these variants is enhancing the ability to understand the physiology of T1DM. However, attempts to build clinically useful models for predicting T1DM risk from these variants have not been successful, and it has been suggested that this would not change with the elucidation of the entire genetic architecture of T1DM [8]. There are ongoing efforts that utilize pre-symptomatic genotyping at the HLA locus to identify individuals at risk and evaluate environmental predictors [9], but to date genetic testing is not considered to be a useful clinical tool in T1DM. Thus, in cases of confirmed T1DM, genetic risk counseling appropriately focuses on empiric risk based on family history.
T2DM, responsible for about 90–95 % of diabetes cases, refers to a heterogeneous group of disorders characterized by a combination of insulin resistance (limitations in the ability to utilize insulin effectively) with a relative insulin deficiency. There is a strong complex and polygenic underlying genetic effect on susceptibility, and factors such as overweight/obesity, sedentary lifestyle and/or aging increase insulin resistance and promote the development of T2DM in susceptible individuals. T2DM is arguably a diagnosis of exclusion since all non-pregnancy diabetes not due to autoimmune processes or a specific known etiology falls into this category. T2DM was in the past known as non-insulin-dependent diabetes mellitus (NIDDM) or adult onset diabetes, terms that have fallen out of favor in the quest to categorize diabetes by etiology rather than treatment and in recognition of the increasing number of children diagnosed with T2DM.
T2DM can be treated with oral agents and in some cases diet and exercise alone, but some affected individuals require insulin depending on the degree of insulin resistance and deficiency and disease duration. Metformin is considered first-line therapy and works partly by reducing insulin resistance [10, 11]. T2DM is highly heterogeneous in etiology and finding the most efficacious treatment can be challenging; for example, not all individuals respond to metformin.
As with T1DM, the genetic architecture of T2DM is complex. To date, variants in at least 65 genetic loci have been implicated in T2DM susceptibility, which together explain approximately 10–11 % of the variance [12••]. Although genetic risk profiling for T2DM is offered by some companies, it does not currently have proven clinical utility [13, 14]. Thus, similar to T1DM, genetic counseling in cases of confirmed T2DM currently focuses on family history-based recurrence risk. The ADA recommends that early (before age 45) testing for T2DM [via fasting or random glucose, oral glucose tolerance test or HBA1c (glycosylated hemoglobin)] be considered in individuals who are overweight [body mass index (BMI) ≥25 kg/m2] and have one or more additional risk factors, one of which is a first-degree relative with diabetes [15].
“Other specific types of diabetes” encompasses several etiologies including those caused by genetic defects in the insulin producing β-cells of the pancreas, genetic defects in insulin action, diseases of the exocrine pancreas (i.e., pancreatitis, trauma, etc.), endocrinopathies (i.e., acromegaly, Cushing’s syndrome, etc.), syndromes that include diabetes as a component, and drug-, injury-, transplant-, or chemical-induced, or infectious. Most relevant to this review are monogenic and syndromic forms of diabetes, which will be discussed in turn here. Table 1 summarizes the most well-established clinical implications of properly diagnosing monogenic diabetes; more detailed information can found at the University of Exeter Medical School website, a major source of research and clinical insights regarding monogenic diabetes and publications (http://www.diabetesgenes.org) [16]. Additional information, including links to patient registries, can be found at The University of Chicago Monogenic Diabetes website (http://monogenicdiabetes.uchicago.edu/what-is-monogenic-diabetes/).
Maturity-onset diabetes of the young (MODY) is the most common type of monogenic diabetes and results from one of several single gene defects in β-cell function. It is inherited in an autosomal dominant manner. In the classic criteria, patients typically present with diabetes at a young age (<25 years), are not necessarily obese, continue to make insulin, lack T1DM-related autoantibodies, and have other family members with diabetes [17, 18]. However, these criteria are likely too narrow. MODY can often be mistaken for both T1DM and T2DM because of overlapping characteristic features. To date, 13 different genes have been implicated in causing MODY [19–23]. Most commonly, MODY results from mutations in transcription factor genes involved in the insulin secretion/β-cell development pathways. Mutations in HNF1A, encoding the transcription hepatic nuclear factor 1α (HNF1α), results in MODY3, the most frequent MODY subtype, responsible for 52 % of MODY cases [24, 25]. Mutations in GCK, encoding the enzyme glucokinase, are implicated in 32 % of MODY cases [26–29]. About 10 % of MODY cases are due to mutations in HNF4A (MODY1), encoding the transcription factor HNF4α. The other genes with mutations more rarely causing MODY include IPF-1 (MODY4), HNF1B (MODY5), NEUROD1 (MODY6), KLF11 (MODY7), CEL (MODY8), PAX4 (MODY9), INS (MODY10), BLK (MODY11), ABCC8 (MODY12), and KCNJ11 (MODY13) [22, 23, 30, 31]. Still, some families with MODY remain genetically unexplained (MODY-X), but with advancements in DNA sequencing techniques, additional genes will continue to be identified [23].
Patients with transcription factor MODY subtypes develop progressive hyperglycemia, typically in adolescence or early adulthood [32]. They are at risk for diabetes-related complications if not treated and so require appropriate monitoring including regular eye and foot exams and screening of the urine for microalbuminuria (the earliest detection for kidney disease) [33]. Patients with HNF1A (MODY3) and HNF4A (MODY1) mutations are especially sensitive to low doses of the sulfonylurea class of antidiabetic agents, which should be tried first, although some still may require insulin, especially at later stages [33–35]. This is in contrast to standard of care for T1DM, where insulin is started immediately upon diagnosis, and T2DM, for which metformin is the first-line treatment. Therefore, distinguishing at least these types of transcription factor diabetes from T1DM and T2DM is paramount.
GCK-MODY (MODY2) characteristically presents with stable, mildly elevated blood glucoses that do not progress or cause complications. Therefore, these patients’ glucoses can be monitored intermittently but most do not necessitate treatment [36]. Since T1DM can present with mild hyperglycemia if diagnosed through routine screening, identifying a GCK mutation can prevent unnecessary invasive and possibly harmful treatment with insulin. As discussed below, GCK mutations increase the risk for GDM, and there appears to be value for optimal pregnancy management in knowing the maternal and fetal mutation status.
Those with MODY5, due to HNF1B mutations, can have developmental problems of the kidneys (most often cysts) and so require co-management by nephrologists [37]. Because of the coexisting renal problems, MODY5 is often classified instead as a syndrome (renal cysts and diabetes syndrome, or RCAD), and poor kidney function in the presence of good glucose control can be a clue to the presence of an HNF1B mutation [38].
Neonatal diabetes is a rare (1/100,000 newborns) monogenic diabetes subtype that presents in the first six months of life, and can be transient (TNDM) or permanent (PNDM) [39]. PNDM most often results from activating mutations in the KCNJ11 gene encoding the pore-forming Kir6.2 subunit of the potassium-sensitive ATP (KATP) channel (57, 58), which in some cases also cause developmental delay and seizures. Most patients with neonatal diabetes due to mutations in KCNJ11 and ABCC8, which encodes the sulfonylurea receptor (SUR) subunit of the KATP channel, can be successfully treated with high doses of the sulfonylurea class of antidiabetic agents. These should be chosen as first-line therapy [40–42], in contrast to other cases of neonatal diabetes, which are treated with insulin. Thus, it is essential for clinical care that any infant diagnosed with diabetes be tested for mutations in these genes, since such a diagnosis makes treatment less invasive and more effective.
Abnormalities leading to overexpression of the imprinted genes PLAGL1 and HYMAI on chromosome 6q are the most common cause of TNDM, accounting for about 70 % of cases, and may also result in accompanying macroglossia or umbilical hernia [43–45]. At onset, TNDM is treated with insulin. Spontaneous remission occurs at a mean age of 4.5 months, at which point therapy can be stopped. Relapses occur in about 50 % of cases during childhood or adolescence, and so these patients and their families need counseling on the symptoms of hyperglycemia and intermittent monitoring of their glucoses after initial remission [43, 45]. On relapse, some require insulin for treatment, whereas others can be managed on pills [39, 41]. Several other genes are implicated in neonatal diabetes including INS, GCK, PDX1, HNF1B, and EIF2AK3.
As noted above, some genetic syndromes include diabetes as a prominent feature or are associated with an increased risk to develop diabetes. Table 2 lists key syndromes with diabetes as a prominent feature.
GDM is hyperglycemia first diagnosed during pregnancy, a time of insulin resistance induced by placental hormones [46]. Women diagnosed with GDM are at a significantly increased risk for developing T2DM later in life [47]. For some women, a diagnosis of GDM may be the first recognition of pre-existing T2DM, which can be asymptomatic. Maternal hyperglycemia in the third trimester is associated with adverse maternal, fetal, and neonatal outcomes including macrosomia and perinatal distress. It is also well-known that pre-existing maternal hyperglycemia increases the risk for certain congenital malformations. Therefore, diagnosis and effective treatment are essential [48]. Treatment of GDM can include lifestyle therapy with diet and exercise, or pharmacological therapy with antidiabetic pills or insulin, depending on the degree of hyperglycemia [49]. In addition, screening for diabetes is recommended 6 to 12 weeks postpartum given the increased risk.
GDM is often viewed not as a specific disease, but as a manifestation of underlying glucose intolerance brought out by the insulin sensitivity-challenging conditions of pregnancy, and this is borne out by the association of T2DM variants with GDM [50]. For example, the TCF7L2 rs7903146 variant conferred an increased risk (1.56- to 2.69-fold for heterozygotes, 2.05- to 3.25-fold for homozygotes compared with non-carriers) [51–53]. Numerous other T2DM-susceptibility variants have been associated with GDM as well [52, 54–58]. Similar to T2DM, these common variants do not currently lend themselves to clinically useful genetic testing. Thus, similarly, family history of both GDM and T2DM can be used as a guide to estimate the risk of GDM.
An area that brings relevance of genetic counseling and testing to GDM is the effect of maternal and fetal genotypes on birth weight, as has been observed with the GCK gene, in which mutations cause a monogenic form of diabetes called MODY2. As discussed in the preceding section, MODY2 is a mild condition that manifests as elevated fasting glucose beginning at birth, often does not present as overt diabetes, generally does not require treatment outside of diet, and is associated with a low rate of complications. However, women with GCK mutations but without overt diabetes have a high likelihood of developing gestational diabetes, often beginning early in pregnancy [59]. Based on the study of several large pedigrees, maternal GCK mutations not passed to the fetus resulted in large babies (86th percentile on average), as expected in GDM. In contrast, paternally inherited fetal GCK mutations resulted in small babies (24th percentile). GCK mutations passed from mother to fetus resulted in average weight babies (53rd percentile) [60]. These findings can be explained by fetal mutations causing reduced glucose sensing and insulin secretion and consequent growth retardation. Maternal mutations compensate by creating a hyperglycemic environment that stimulates increased fetal insulin secretion [60–62]. In a case report, aggressive treatment of GDM with insulin throughout two pregnancies in a GCK mutation carrier resulted in the birth of one baby who inherited the mutation and was in the lowest percentile for weight and a second baby who did not inherit the mutation but was of normal weight [63]. These findings suggest that determining the GCK-mutation status of women with GDM and their infants could be useful in deciding how aggressively to treat the maternal hyperglycemia.
It is not known how prevalent GCK mutations are in GDM, but studies in various populations have estimated 5 % [64–66]. One study selecting 15 women on specific criteria (fasting hyperglycemia outside pregnancy, insulin required during but not outside pregnancy, limited 2 h glucose increase, and first-degree family history) found mutations in 80 % [67]. Very recently, a population-based study in Ireland found evidence that combined criteria of a BMI <25 kg/m2 and fasting glucose ≥5.5 mmol/l could identify women with GCK mutations with a sensitivity of 68 % and specificity of 98 % [68•]. It is not yet known how well these criteria apply to other populations, but the findings reported in the preceding paragraph indicate that knowing the maternal GCK status would be useful during pregnancy. While determining the baby’s mutation status would currently require an invasive test such as amniocentesis, it has been suggested that serial fetal abdominal scans be used to monitor growth in women with GCK mutations [63]. Given that currently (based on a survey reported in 2004) fetal growth in GDM is monitored by ultrasound by only 7 % of OB/GYNs [69], knowledge that the fetus inherited GCK-mutation-induced delayed insulin release could serve as a potential tool for selecting women for more intensive monitoring and potential avoidance of aggressive glucose control during the current and future pregnancies in the presence of a GCK mutation. As the genetic architecture of diabetes continues to be elucidated, other genetic variants could serve as a source of information to guide pregnancy management as well.
Genetic Counseling and Testing in Diabetes
The Clinical Challenge
Anecdotal and survey evidence suggests that a personal or family history of diabetes is rarely a presenting indication for genetic counseling, other than for women with diabetes seeking to understand the risks to the pregnancy associated with exposure to maternal hyperglycemia. When diabetes is encountered in a family history taken for other genetic indications, counselors typically ask patients what type of diabetes, and, if not known, age of onset and whether insulin is used. Patients are then advised that there is an increased risk for diabetes in relatives of individuals with diabetes. Empiric risk figures based on the apparent type of diabetes (1 or 2), such as those presented in Harper [70], are sometimes provided along with an explanation of their limitations.
In the diabetes clinic, both MODY and neonatal diabetes are often misdiagnosed as T1DM and T2DM [4, 71]. When antibody-negative subjects diagnosed with diabetes at less than 20 years old were sequenced for mutations in the HNF1A, HNF4A, and GCK genes, 36 and 51 % were found to be previously misdiagnosed as having T1DM and T2DM, respectively [4••]; 67 % of those diagnosed with diabetes at less than six months old with KCNJ11, ABCC8, and INS gene mutations carried the wrong diagnosis of T1DM [72••]. The molecular diagnosis is often missed because they share similar characteristics with both T1DM and T2DM, and we do not have a validated screening tool to find cases. In addition, healthcare providers are not as well versed on these rarer subtypes as school curricula and medical training tend to focus on the more common T1DM and T2DM. Further compounding the problem is the lack of access to and cost of diagnostic testing.
In sum, current clinical practices do not favor the identification of patients with highly genetic forms of diabetes that may benefit from molecular diagnosis in either the genetics clinic or the diabetes care setting.
Improving the Pickup Rate for Monogenic Diabetes
Properly diagnosing highly genetic forms of diabetes is critical so that patients can potentially go on more optimal therapy (i.e., an oral sulfonylurea agent rather than insulin) for an improved quality of life and often improved glycemic control. Making the proper diagnosis also allows us to predict the clinical course, explain associated clinical features (i.e., renal disease with MODY5), and diagnose family members early to get them on treatment and hopefully prevent complications from developing. Since it appears that highly genetic forms of diabetes are currently unlikely to be identified in either a genetics or diabetes setting, a new model is needed in which each individual with diabetes has the opportunity to be considered for the possibility of diabetes.
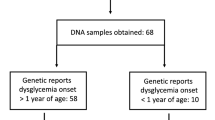
Equal Opportunity for All: Screening and Testing for Monogenic Diabetes in the Diabetes Clinic
In the diabetes clinic, we propose a tiered screening approach in which the target population is all individuals with diabetes. We have begun to implement this approach in the University of Maryland Center for Diabetes and Endocrinology Personalized Diabetes Medicine Program (PDMP) on a research basis. Each new and returning patient with diabetes completes a quick survey consisting of seven yes/no questions that identify patients with a high likelihood of monogenic diabetes. Currently the survey is completed on paper, but development of an electronic version that can integrate with the electronic health record is planned. Patients referred by providers or screening positive on the questionnaire with one of the following profiles are selected for further evaluation: diabetes diagnosed <1 year of age, diagnosed with T1DM and having a parent with T1DM, diagnosed with T2DM at <30 years old and not obese at diagnosis, diagnosed with T2DM at <45 years of age and two or more first- or second-degree relatives diagnosed <50 years of age, or presence of diabetes plus an extrapancreatic feature that may be indicative of a syndrome. Further evaluation using a combination of laboratory testing (C-peptide and IA-2 antibodies) and family and medical history elicited by a genetic counselor is used to determine eligibility for testing.
Testing for the most well-known and clinically actionable forms of monogenic diabetes is currently available in several clinical laboratories. However, the cost of standard Sanger sequencing and sometimes lack of insurance coverage for sequencing several genes that may be implicated can discourage testing. Therefore, several groups outside the US [73•, 74•, 75•] have developed monogenic diabetes panels that utilize next-generation sequencing technologies to test patients suspected to have any type of monogenic diabetes simultaneously for coding mutations in 30 or more genes. We are currently developing such a panel.
Besides the screening and testing algorithm and panel, we are developing protocols for incorporating molecular diagnosis into the electronic health record and using it to inform patient care. Thus, as with any screening program, there are three main goals to our PDMP: to provide the entire target population access to personalized diabetes care; to facilitate accurate follow-up diagnostic testing; and to educate and make available appropriate intervention when a diagnosis is made. We are in the process of extending this approach into primary care settings, where many patients with diabetes are seen for most of their care, and collecting outcome data on the PDMP in order to determine efficacy of this approach so that it can be implemented on a more widespread basis and more specific clinical practice recommendations can be developed. While a genetic counselor is part of the clinical team in our current approach, we recognize that this is unlikely to be possible in all specialty and primary care clinics where people with diabetes are diagnosed and treated. Thus, an important component of a more widespread screening and testing program will be the development of guidelines for referring to genetic counselors and clinical geneticists for evaluation and counseling once a diagnosis has been made. For example, in cases of suspected mitochondrial disorder, we recommend that the patient/family be referred to a clinical geneticist for further evaluation and a thorough discussion of maternal inheritance. We believe that most effective will be a team approach, in which practitioners in diabetes care and genetics engage each other in a reciprocal relationship to assure the optimal diagnosis and treatment of these patients.
The Genetic Counseling Session: A Golden Opportunity for Case Identification
Given the gross underdiagnosis of monogenic diabetes demonstrated previously, the genetic counseling session can be viewed as an opportunity for genetic counselors and geneticists to utilize their skills in family history collection and interpretation to identify patterns consistent with these less common forms of diabetes. In order to accomplish this, we propose a modified version of our diabetes clinic screening and testing protocol, summarized in Fig. 1. In this proposed approach, for each individual mentioned as having diabetes, the consultand is asked the individual’s age of onset, whether the individual was obese at onset, whether a diagnosis was made of T1DM and/or insulin has been used from onset, and whether there are any extrapancreatic features, such as early onset visual/hearing/cognitive impairment and/or kidney or other birth defects. Any individual with a diagnosis before one year of age, particularly before six months of age, should be considered for testing for neonatal diabetes. Individuals in the pedigree with diabetes plus extrapancreatic features should be assessed for the presence of a syndrome through careful review of available medical records and consultation of the literature, OMIM, and other databases. Table 2 lists some of the syndromes with diabetes as a prominent feature and provides insights as to which extrapancreatic features might be seen in syndromic diabetes. For example, it is important to inquire about hearing loss in individuals with diabetes, as it could be indicative of mitochondrial dysfunction as well as Wolfram and Roger’s syndromes. Diagnosis of a syndrome then facilitates genetic counseling regarding risk and testing options for additional family members.
Individuals who have neither neonatal onset nor a syndrome can be evaluated for scenarios that, based on published guidelines or research [15, 76, 77••], are consistent with monogenic diabetes: (1) diagnosis of T1DM in a parent and child, (2) diagnosis of T2DM before age 30 in the absence of obesity, and (3) diagnosis of diabetes before age 45 and two first-degree relatives in the same lineage diagnosed with diabetes before age 50. We have developed this third criterion as a starting point to use family history to increase the pickup rate over more strict age and obesity criteria. For family members meeting these criteria, the genetic team could work with the diabetes team to determine whether the individual was antibody negative and C-peptide positive, in which case MODY testing would be considered. Finally, those not meeting any of the criteria above would be considered to have T1DM or T2DM based on history, and empiric risk counseling could be provided. While, as stated earlier, common genetic variant susceptibility panels have not proven to be a useful approach for modifying risk for T1DM and T2DM, the polygenic burden approach, in which models constructed from several hundred thousand SNPs currently under study may prove useful in the future, particularly in the absence of available or extensive family history information.
Education is key
In order to increase recognition of these rarer subtypes of diabetes, it is important to include information about monogenic diabetes and features that distinguish it from T1DM and T2DM in medical school, genetic counseling, residence, and fellowship curricula. Primary care physicians, endocrinologists, diabetes educators, genetic counselors, and geneticists are especially likely to see these patients in their clinics and need to be ready to recognize them.
Conclusion
The etiology of diabetes is extremely heterogeneous. While most individuals have T1DM or T2DM and complex inheritance, some diabetes results from a mutation in a single gene. Many of the relevant genes have been known for nearly two decades, but these forms of diabetes remain vastly underdiagnosed. Properly diagnosing monogenic diabetes can have a profound impact on health and quality of life. It is hoped that the information provided in these pages will arm both genetics and diabetes professionals with the tools to begin to work cooperatively to identify, diagnose, and provide these individuals with optimal care.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Centers for disease control and prevention. National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States. 2011.
World health organization, http://www.who.int/en/. 2013.
•• American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2014;S81–S90. Comprehensive overview of diabetes, its subtypes, and diagnostic criteria; part of the Clinical Practice Guidelines issued annually by the American Diabetes Association.
•• Pihoker C, Gilliam LK, Ellard S, et al. SEARCH for Diabetes in Youth Study Group. Prevalence, characteristics and clinical diagnosis of maturity onset diabetes of the young due to mutations in HNF1A, HNF4A, and glucokinase: results from the SEARCH for Diabetes in Youth. J Clin Endocrinol Metab. 2013;98:4055–4062. Recent report from a US population-based study revealing the prevalence and underdiagnoses of monogenic diabetes among children and adolescents.
Stenstrom G, Gottsater A, Bakhtadze E, Berger B, Sundkvist G. Latent autoimmune diabetes in adults: definition, prevalence, beta-cell function, and treatment. Diabetes. 2005;54:S68–72.
Erlich H, Valdes AM, Noble J, Carlson JA, Varney M, Concannon P, Mychaleckyj JC, Todd JA, Bonella P, Fear AL, Lavant E, Louey A, Moonsamy P, Type 1 Diabetes Genetics Consortium. HLA DR-DQ haplotypes and genotypes and type 1 diabetes risk: analysis of the type 1 diabetes genetics consortium families. Diabetes. 2008;57:1084–92.
Pociot F, Akolkar B, Concannon P, Erlich HA, Julier C, Morahan G, Nierras CR, Todd JA, Rich SS, Nerup J. Genetics of type 1 diabetes: what’s next? Diabetes. 2010;59:1561–71.
Clayton DG. Prediction and interaction in complex disease genetics: experience in type 1 diabetes. PLoS Genet. 2009;5:e1000540.
Hagopian WA, Erlich H, Lernmark A, Rewers M, Ziegler AG, Simell O, Akolkar B, Vogt R, Blair A, Ilonen J, Krischer J, She J, TEDDY Study Group. The Environmental Determinants of Diabetes in the Young (TEDDY): genetic criteria and international diabetes risk screening of 421,000 infants. Pediatr Diabetes. 2011;12:733–43.
Stumvoll M, Nurjhan N, Perriello G, Dailey G, Gerich JE. Metabolic effects of metformin in non-insulin-dependent diabetes mellitus. N Engl J Med. 1995;333:550–4.
Giannarelli R, Aragona M, Coppelli A, Del Prato S. Reducing insulin resistance with metformin: the evidence today. Diabetes Metab. 2003;29:6S28–35.
•• Morris AP, Voight BF, Teslovich TM, Ferreira T, Segre AV, Steinthorsdottir V, Strawbridge RJ, Khan H, Grallert H, Mahajan A, Prokopenko I, Kang HM, Dina C, Esko T, Fraser RM, Kanoni S, Kumar A, Lagou V, Langenberg C, Luan J, Lindgren CM, Muller-Nurasyid M, Pechlivanis S, Rayner NW, Scott LJ, Wiltshire S, Yengo L, Kinnunen L, Rossin EJ, Raychaudhuri S, Johnson AD, Dimas AS, Loos RJ, Vedantam S, Chen H, Florez JC, Fox C, Liu CT, Rybin D, Couper DJ, Kao WH, Li M, Cornelis MC, Kraft P, Sun Q, van Dam RM, Stringham HM, Chines PS, Fischer K, Fontanillas P, Holmen OL, Hunt SE, Jackson AU, Kong A, Lawrence R, Meyer J, Perry JR, Platou CG, Potter S, Rehnberg E, Robertson N, Sivapalaratnam S, Stancakova A, Stirrups K, Thorleifsson G, Tikkanen E, Wood AR, Almgren P, Atalay M, Benediktsson R, Bonnycastle LL, Burtt N, Carey J, Charpentier G, Crenshaw AT, Doney AS, Dorkhan M, Edkins S, Emilsson V, Eury E, Forsen T, Gertow K, Gigante B, Grant GB, Groves CJ, Guiducci C, Herder C, Hreidarsson AB, Hui J, James A, Jonsson A, Rathmann W, Klopp N, Kravic J, Krjutskov K, Langford C, Leander K, Lindholm E, Lobbens S, Mannisto S, Mirza G, Muhleisen TW, Musk B, Parkin M, Rallidis L, Saramies J, Sennblad B, Shah S, Sigurethsson G, Silveira A, Steinbach G, Thorand B, Trakalo J, Veglia F, Wennauer R, Winckler W, Zabaneh D, Campbell H, van Duijn C, Uitterlinden AG, Hofman A, Sijbrands E, Abecasis GR, Owen KR, Zeggini E, Trip MD, Forouhi NG, Syvanen AC, Eriksson JG, Peltonen L, Nothen MM, Balkau B, Palmer CN, Lyssenko V, Tuomi T, Isomaa B, Hunter DJ, Qi L, Wellcome Trust Case Control Consortium, Meta-Analyses of Glucose and Insulin-related traits Consortium (MAGIC) Investigators, Genetic Investigation of ANthropometric Traits (GIANT) Consortium, Asian Genetic Epidemiology Network-Type 2 Diabetes (AGEN-T2D) Consortium, South Asian Type 2 Diabetes (SAT2D) Consortium, Shuldiner AR, Roden M, Barroso I, Wilsgaard T, Beilby J, Hovingh K, Price JF, Wilson JF, Rauramaa R, Lakka TA, Lind L, Dedoussis G, Njolstad I, Pedersen NL, Khaw KT, Wareham NJ, Keinanen-Kiukaanniemi SM, Saaristo TE, Korpi-Hyovalti E, Saltevo J, Laakso M, Kuusisto J, Metspalu A, Collins FS, Mohlke KL, Bergman RN, Tuomilehto J, Boehm BO, Gieger C, Hveem K, Cauchi S, Froguel P, Baldassarre D, Tremoli E, Humphries SE, Saleheen D, Danesh J, Ingelsson E, Ripatti S, Salomaa V, Erbel R, Jockel KH, Moebus S, Peters A, Illig T, de Faire U, Hamsten A, Morris AD, Donnelly PJ, Frayling TM, Hattersley AT, Boerwinkle E, Melander O, Kathiresan S, Nilsson PM, Deloukas P, Thorsteinsdottir U, Groop LC, Stefansson K, Hu F, Pankow JS, Dupuis J, Meigs JB, Altshuler D, Boehnke M, McCarthy MI, DIAbetes Genetics Replication And Meta-analysis (DIAGRAM) Consortium. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012;44:981–90. Most recent meta-analysis of type 2 diabetes genes.
Kuehn BM. Inconsistent results, inaccurate claims plague direct-to-consumer gene tests. JAMA. 2010;1313:45–52.
Mihaescu R, Meigs J, Sijbrands E, Janssens AC. Genetic risk profiling for prediction of type 2 diabetes. PLoS Curr. 2011;3:RRN1208.
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2014;37:S14–80.
Murphy R, Ellard S, Hattersley AT. Clinical implications of a molecular genetic classification of monogenic beta-cell diabetes. Nat Clin Pract Endocrinol Metab. 2008;4:200–13.
Froguel P, Velho G. Molecular genetics of maturity-onset diabetes of the young. Trends Endocrinol Metab. 1999;10:142–6.
Ehtisham S, Hattersley AT, Dunger DB, Barrett TG. First UK survey of paediatric type 2 diabetes and MODY. Arch Dis Child. 2004;89:526–9.
Ledermann HM. Maturity-onset diabetes of the young (MODY) at least ten times more common in Europe than previously assumed? Diabetologia. 1995;38:1482.
Schober E, Rami B, Grabert M, Thon A, Kapellen T, Reinehr T, Holl RW, Wiss DPV. Initiative of the German Working Group for Paediatric Diabetology and phenotypical aspects of maturity-onset diabetes of the young (MODY diabetes) in comparison with Type 2 diabetes mellitus (T2DM) in children and adolescents: experience from a large multicentre database. Diabet Med. 2009;26:466–73.
Molven A, Njolstad PR. Role of molecular genetics in transforming diagnosis of diabetes mellitus. Expert Rev Mol Diagn. 2011;11:313–20.
Bowman P, Flanagan SE, Edghill EL, Damhuis A, Shepherd MH, Paisey R, Hattersley AT, Ellard S. Heterozygous ABCC8 mutations are a cause of MODY. Diabetologia. 2012;55:123–7.
Bonnefond A, Philippe J, Durand E, Dechaume A, Huyvaert M, Montagne L, Marre M, Balkau B, Fajardy I, Vambergue A, Vatin V, Delplanque J, Le Guilcher D, De Graeve F, Lecoeur C, Sand O, Vaxillaire M, Froguel P. Whole-exome sequencing and high throughput genotyping identified KCNJ11 as the thirteenth MODY gene. PLoS One. 2012;7:e37423.
Shields BM, Hicks S, Shepherd MH, Colclough K, Hattersley AT, Ellard S. Maturity-onset diabetes of the young (MODY): how many cases are we missing? Diabetologia. 2010;53:2504–8.
Frayling TM, Bulamn MP, Ellard S, Appleton M, Dronsfield MJ, Mackie AD, Baird JD, Kaisaki PJ, Yamagata K, Bell GI, Bain SC, Hattersley AT. Mutations in the hepatocyte nuclear factor-1 alpha gene are a common cause of maturity-onset diabetes of the young in the UK. Diabetes. 1997;46:720–5.
Matschinsky FM, Glaser B, Magnuson MA. Pancreatic beta-cell glucokinase: closing the gap between theoretical concepts and experimental realities. Diabetes. 1998;47:307–15.
Froguel P, Zouali H, Vionnet N, Velho G, Vaxillaire M, Sun F, Lesage S, Stoffel M, Takeda J, Passa P. Familial hyperglycemia due to mutations in glucokinase. Definition of a subtype of diabetes mellitus. N Engl J Med. 1993;328:697–702.
Byrne MM, Sturis J, Clement K, Vionnet N, Pueyo ME, Stoffel M, Takeda J, Passa P, Cohen D, Bell GI. Insulin secretory abnormalities in subjects with hyperglycemia due to glucokinase mutations. J Clin Invest. 1994;93:1120–30.
Shields BM, Spyer G, Slingerland AS, Knight BA, Ellard S, Clark PM, Hauguel-de Mouzon S, Hattersley AT. Mutations in the glucokinase gene of the fetus result in reduced placental weight. Diabetes Care. 2008;31:753–7.
Molven A, Ringdal M, Nordbo AM, Raeder H, Stoy J, Lipkind GM, Steiner DF, Philipson LH, Bergmann I, Aarskog D, DE Undlien, Joner G, Sovik O, Norwegian Childhood Diabetes Study Group, Bell GI, Njolstad PR. Mutations in the insulin gene can cause MODY and autoantibody-negative type 1 diabetes. Diabetes. 2008;57:1131–5.
Beards F, Frayling T, Bulman M, Horikawa Y, Allen L, Appleton M, Bell GI, Ellard S, Hattersley AT. Mutations in hepatocyte nuclear factor 1 beta are not a common cause of maturity-onset diabetes of the young in the UK. Diabetes. 1998;47:1152–4.
Bellanne-Chantelot C, Levy DJ, Carette C, Saint-Martin C, Riveline JP, Larger E, Valero R, Gautier JF, Reznik Y, Sola A, Hartemann A, Laboureau-Soares S, Laloi-Michelin M, Lecomte P, Chaillous L, Dubois-Laforgue D, Timsit J, French Monogenic Diabetes Study Group. Clinical characteristics and diagnostic criteria of maturity-onset diabetes of the young (MODY) due to molecular anomalies of the HNF1A gene. J Clin Endocrinol Metab. 2011;96:E1346–51.
Velho G, Vaxillaire M, Boccio V, Charpentier G, Froguel P. Diabetes complications in NIDDM kindreds linked to the MODY3 locus on chromosome 12q. Diabetes Care. 1996;19:915–9.
Pearson ER, Liddell WG, Shepherd M, Corrall RJ, Hattersley AT. Sensitivity to sulphonylureas in patients with hepatocyte nuclear factor-1 alpha gene mutations: evidence for pharmacogenetics in diabetes. Diabet Med. 2000;17:543–5.
Pearson ER, Starkey BJ, Powell RJ, Gribble FM, Clark PM, Hattersley AT. Genetic cause of hyperglycaemia and response to treatment in diabetes. Lancet. 2003;362:1275–81.
Velho G, Blanche H, Vaxillaire M, Bellanne-Chantelot C, Pardini VC, Timsit J, Passa P, Deschamps I, Robert JJ, Weber IT, Marotta D, Pilkis SJ, Lipkind GM, Bell GI, Froguel P. Identification of 14 new glucokinase mutations and description of the clinical profile of 42 MODY-2 families. Diabetologia. 1997;40:217–24.
Nishigori H, Yamada S, Kohama T, Tomura H, Sho K, Horikawa Y, Bell GI, Takeuchi T, Takeda J. Frameshift mutation, A263fsinsGG, in the hepatocyte nuclear factor-1 beta gene associated with diabetes and renal dysfunction. Diabetes. 1998;47:1354–5.
Edghill EL, Bingham C, Slingerland AS, Minton JA, Noordam C, Ellard S, Hattersley AT. Hepatocyte nuclear factor-1 beta mutations cause neonatal diabetes and intrauterine growth retardation: support for a critical role of HNF-1 beta in human pancreatic development. Diabet Med. 2006;23:1301–6.
Polak M, Shield J. Neonatal and very-early-onset diabetes mellitus. Semin Neonatol. 2004;9:59–65.
Zung A, Glaser B, Nimri R, Zadik Z. Glibenclamide treatment in permanent neonatal diabetes mellitus due to an activating mutation in Kir6.2. J Clin Endocrinol Metab. 2004;89:5504–7.
Babenko AP, Polak M, Cave H, Busiah K, Czernichow P, Scharfmann R, Bryan J, Aguilar-Bryan L, Vaxillaire M, Froguel P. Activating mutations in the ABCC8 gene in neonatal diabetes mellitus. N Engl J Med. 2006;355:456–66.
Pearson ER, Flechtner I, Njolstad PR, Malecki MT, Flanagan SE, Larkin B, Ashcroft FM, Klimes I, Codner E, Iotova V, Slingerland AS, Shield J, Robert JJ, Holst JJ, Clark PM, Ellard S, Sovik O, Polak M, Hattersley AT, Neonatal Diabetes International Collaborative Group. Switching from insulin to oral sulfonylureas in patients with diabetes due to Kir6.2 mutations. N Engl J Med. 2006;355:467–77.
Docherty LE, Kabwama S, Lehmann A, Hawke E, Harrison L, Flanagan SE, Ellard S, Hattersley AT, Shield JP, Ennis S, Mackay DJ, Temple IK. Clinical presentation of 6q24 transient neonatal diabetes mellitus (6q24 TNDM) and genotype-phenotype correlation in an international cohort of patients. Diabetologia. 2013;56:758–62.
Arima T, Drewell RA, Arney KL, Inoue J, Makita Y, Hata A, Oshimura M, Wake N, Surani MA. A conserved imprinting control region at the HYMAI/ZAC domain is implicated in transient neonatal diabetes mellitus. Hum Mol Genet. 2001;10:1475–83.
Temple IK, Gardner RJ, Mackay DJ, Barber JC, Robinson DO, Shield JP. Transient neonatal diabetes: widening the understanding of the etiopathogenesis of diabetes. Diabetes. 2000;49:1359–66.
Kuhl C. Insulin secretion and insulin resistance in pregnancy and GDM. Implications for diagnosis and management. Diabetes. 1991;40(Suppl 2):18–24.
Lobner K, Knopff A, Baumgarten A, Mollenhauer U, Marienfeld S, Garrido-Franco M, Bonifacio E, Ziegler AG. Predictors of postpartum diabetes in women with gestational diabetes mellitus. Diabetes. 2006;55:792–7.
HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan, Hadden, McCance, Hod M, McIntyre HD, Oats JJ, Persson B, Rogers, Sacks DA. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002.
Blumer I, Hadar E, Hadden DR, Jovanovic L, Mestman JH, Murad MH, Yogev Y. Diabetes and pregnancy: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2013;98:4227–49.
Watanabe RM. Inherited destiny? Genetics and gestational diabetes mellitus. Genome Med. 2011;18:99–103.
Shaat N, Lernmark A, Karlsson E, Ivarsson S, Parikh H, Berntorp K, Groop L. A variant in the transcription factor 7-like 2 (TCF7L2) gene is associated with an increased risk of gestational diabetes mellitus. Diabetologia. 2007;50:972–9.
Pappa KI, Gazouli M, Economou K, Daskalakis G, Anastasiou E, Anagnou NP, Antsaklis A. Gestational diabetes mellitus shares polymorphisms of genes associated with insulin resistance and type 2 diabetes in the Greek population. Gynecol Endocrinol. 2011;27:267–72.
Freathy RM, Hayes MG, Urbanek M, Lowe LP, Lee H, Ackerman C, Frayling TM, Cox NJ, Dunger DB, Dyer AR, Hattersley AT, Metzger BE, Lowe WL Jr, HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: common genetic variants in GCK and TCF7L2 are associated with fasting and postchallenge glucose levels in pregnancy and with the new consensus definition of gestational diabetes mellitus from the International Association of Diabetes and Pregnancy Study Groups. Diabetes. 2010;59:2682–9.
Chon SJ, Kim SY, Cho NR, Min DL, Hwang YJ, Mamura M. Association of variants in PPARgamma(2), IGF2BP2, and KCNQ1 with a susceptibility to gestational diabetes mellitus in a Korean population. Yonsei Med J. 2013;54:352–7.
Leipold H, Knoefler M, Gruber C, Huber A, Haslinger P, Worda C. Peroxisome proliferator-activated receptor gamma coactivator-1 alpha gene variations are not associated with gestational diabetes mellitus. J Soc Gynecol Investig. 2006;13:104–7.
Cho YM, Kim TH, Lim S, Choi SH, Shin HD, Lee HK, Park KS, Jang HC. Type 2 diabetes-associated genetic variants discovered in the recent genome-wide association studies are related to gestational diabetes mellitus in the Korean population. Diabetologia. 2009;52:253–61.
Mao H, Li Q, Gao S. Meta-analysis of the relationship between common type 2 diabetes risk gene variants with gestational diabetes mellitus. PLoS One. 2012;7:e45882.
Hayes MG, Urbanek M, Hivert MF, Armstrong LL, Morrison J, Guo C, Lowe LP, Scheftner DA, Pluzhnikov A, Levine DM, McHugh CP, Ackerman CM, Bouchard L, Brisson D, Layden BT, Mirel D, Doheny KF, Leya MV, Lown-Hecht RN, Dyer AR, Metzger BE, Reddy TE, Cox NJ, Lowe WL Jr, HAPO Study Cooperative Research Group. Identification of HKDC1 and BACE2 as genes influencing glycemic traits during pregnancy through genome-wide association studies. Diabetes. 2013;62:3282–91.
Fajans SS, Bell GI, Polonsky KS. Molecular mechanisms and clinical pathophysiology of maturity-onset diabetes of the young. N Engl J Med. 2001;345:971–80.
Hattersley AT, Beards F, Ballantyne E, Appleton M, Harvey R, Ellard S. Mutations in the glucokinase gene of the fetus result in reduced birth weight. Nat Genet. 1998;19:268–70.
Hattersley AT, Tooke JE. The fetal insulin hypothesis: an alternative explanation of the association of low birthweight with diabetes and vascular disease. Lancet. 1999;353:1789–92.
Terauchi Y, Kubota N, Tamemoto H, Sakura H, Nagai R, Akanuma Y, Kimura S, Kadowaki T. Insulin effect during embryogenesis determines fetal growth: a possible molecular link between birth weight and susceptibility to type 2 diabetes. Diabetes. 2000;49:82–6.
Spyer G, Hattersley AT, Sykes JE, Sturley RH, MacLeod KM. Influence of maternal and fetal glucokinase mutations in gestational diabetes. Obstet Gynecol. 2001;185:240–1.
Saker PJ, Hattersley AT, Barrow B, Hammersley MS, McLellan JA, Lo YM, Olds RJ, Gillmer MD, Holman RR, Turner RC. High prevalence of a missense mutation of the glucokinase gene in gestational diabetic patients due to a founder-effect in a local population. Diabetologia. 1996;39:1325–8.
Kousta E, Ellard S, Allen LI, Saker PJ, Huxtable SJ, Hattersley AT, McCarthy MI. Glucokinase mutations in a phenotypically selected multiethnic group of women with a history of gestational diabetes. Diabet Med. 2001;18:683–4.
Stoffel M, Bell KL, Blackburn CL, Powell KL, Seo TS, Takeda J, Vionnet N, Xiang KS, Gidh-Jain M, Pilkis SJ. Identification of glucokinase mutations in subjects with gestational diabetes mellitus. Diabetes. 1993;42:937–40.
Ellard S, Beards F, Allen LI, Shepherd M, Ballantyne E, Harvey R, Hattersley AT. A high prevalence of glucokinase mutations in gestational diabetic subjects selected by clinical criteria. Diabetologia. 2000;43:250–3.
• Chakera AJ, Spyer G, Vincent N, Ellard S, Hattersley AT, Dunne FP. The 0.1% of the population with glucokinase monogenic diabetes can be recognized by clinical characteristics in pregnancy: the atlantic diabetes in pregnancy cohort. Diabetes Care. 2014. A population-based study in Ireland identified criteria that may be useful in selecting women with GDM for GCK mutation analysis.
Gabbe SG, Gregory RP, Power ML, Williams SB, Schulkin J. Management of diabetes mellitus by obstetrician-gynecologists. Obstet Gynecol. 2004;103:1229–34.
Harper PS. Practical Genetic Counseling. 6th ed. London: Hodder Arnold; 2004.
Moller AM, Dalgaard LT, Pociot F, Nerup J, Hansen T, Pedersen O. Mutations in the hepatocyte nuclear factor-1 alpha gene in Caucasian families originally classified as having type I diabetes. Diabetologia. 1998;41:1528–31.
•• Kanakatti Shankar R, Pihoker C, Dolan LM, Standiford D, Badaru A, Dabelea D, Rodriguez B, Black MH, Imperatore G, Hattersley A, Ellard S, Gilliam LK, SEARCH for Diabetes in Youth Study Group. Permanent neonatal diabetes mellitus: prevalence and genetic diagnosis in the SEARCH for Diabetes in Youth Study. Pediatr Diabetes. 2013;14:174–80. Reveals the prevalence and underdiagnoses of genetic forms of permanent neonatal diabetes.
• Bonnefond A, Durand E, Sand O, De Graeve F, Gallina S, Busiah K, Lobbens S, Simon A, Bellanne-Chantelot C, Letourneau L, Scharfmann R, Delplanque J, Sladek R, Polak M, Vaxillaire M, Froguel P. Molecular diagnosis of neonatal diabetes mellitus using next-generation sequencing of the whole exome. PLoS One. 2010:e13630. Next generation sequencing panel developed in France.
• Ellard S, Lango Allen H, De Franco E, Flanagan SE, Hysenaj G, Colclough K, Houghton JAL, Shepherd M, Hattersley AT, Weedon MN, Caswell R. Improved genetic testing for monogenic diabetes using targeted next-generation sequencing. Diabetologia. 2013. This is the first reported use of a next-generation sequencing panel to diagnose monogenic diabetes, in this case in the UK. Such panels have the potential to decrease cost and increase access to testing.
• Gao R, Liu Y, Gjesing AP, Hollensted M, Wan X, He S, Pedersen O, Yi X, Wang J, Hansen T. Evaluation of a target region capture sequencing platform using monogenic diabetes as a study-model. BMC Genet. 2014:13. Next generation sequencing panel for monogenic diabetes developed in China.
Hattersley A, Bruining J, Shield J, Njolstad P, Donaghue KC. The diagnosis and management of monogenic diabetes in children and adolescents. Pediatr Diabetes. 2009;10:33–42.
•• Thanabalasingham G, Pal A, Selwood MP, Dudley C, Fisher K, Bingley PJ, Ellard S, Farmer AJ, McCarthy MI, Owen KR. Systematic assessment of etiology in adults with a clinical diagnosis of young-onset type 2 diabetes is a successful strategy for identifying maturity-onset diabetes of the young. Diabetes Care. 2012:1206–1212. Population-based study leading to the proposal that MODY be considered in individuals diagnosed with T2DM before age 30, regardless of family history.
Mackay D, Bens S, Perez de Nanclares G, Siebert R, Temple IK. Clinical utility gene card for: transient neonatal diabetes mellitus, 6q24-related. Eur J Hum Genet. 2014;9:e86940.
Mitchell BD, Pollin TI. Genomic imprinting in diabetes. Genome Med. 2010;2:55.
Brickwood S, Bonthron DT, Al-Gazali LI, Piper K, Hearn T, Wilson DI, Hanley NA. Wolcott-Rallison syndrome: pathogenic insights into neonatal diabetes from new mutation and expression studies of EIF2AK3. J Med Genet. 2003;40:685–9.
Hannibal MC, Torgerson T. IPEX Syndrome. In: Pagon RA, Adam MP, Bird TD, Dolan CR, Fong CT, Stephens K, editors. GeneReviews. Seattle: University of Washington; 1993.
Gloyn AL, Diatloff-Zito C, Edghill EL, Bellanné-Chantelot C, Nivot S, Coutant R, Ellard S, Hattersley AT, Robert JJ. KCNJ11 activating mutations are associated with developmental delay, epilepsy and neonatal diabetes syndrome and other neurological features. Eur J Hum Genet. 2006;14:824–30.
Rendtorff ND, Lodahl M, Boulahbel H, Johansen IR, Pandya A, Welch KO, Norris VW, Arnos KS, Bitner-Glindzicz M, Emery SB, Mets MB, Fagerheim T, Eriksson K, Hansen L, Bruhn H, Möller C, Lindholm S, Ensgaard S, Lesperance MM, Tranebjaerg L. Identification of p.A684V missense mutation in the WFS1 gene as a frequent cause of autosomal dominant optic atrophy and hearing impairment. Am J Med Genet A. 2011:1298–1313.
Tranebjaerg L, Barrett T, Rendtorff ND. WFS1-Related Disorders. In: Pagon RA, Adam MP, Bird TD, Dolan CR, Fong CT, Smith RJH, Stephens K, editors. GeneReviews. Seattle: University of Washington; 1993.
Neufeld EJ, Fleming JC, Tartaglini E, Steinkamp MP. Thiamine-responsive megaloblastic anemia syndrome: a disorder of high-affinity thiamine transport. Blood Cells Mol Dis. 2001;27:135–8.
Bergmann AK, Sahai I, Falcone JF, Fleming J, Bagg A, Borgna-Pignati C, Casey R, Fabris L, Hexner E, Mathews L, Ribeiro ML, Wierenga KJ, Neufeld EJ. Thiamine-responsive megaloblastic anemia: identification of novel compound heterozygotes and mutation update. J Pediatr. 2009;155:888–92.
Edghill EL, Bingham C, Ellard S, Hattersley AT. Mutations in hepatocyte nuclear factor-1 beta and their related phenotypes. J Med Genet. 2006;43:84–90.
Maassen JA, Janssen GM, Hart LM. Molecular mechanisms of mitochondrial diabetes (MIDD). Ann Med. 2005;37:213–21.
Senda M, Ogawa S, Nako K, Okamura M, Sakamoto T, Ito S. The glucagon-like peptide-1 analog liraglutide suppresses ghrelin and controls diabetes in a patient with Prader–Willi syndrome. Endocr J. 2012;59:889–94.
Seetho IW, Jones G, Thomson GA, Fernando DJS. Treating diabetes mellitus in Prader–Willi syndrome with Exenatide. Diabetes Res Clin Pract. 2011;92:e1–2.
Deal CL, Tony M, Höybye C, Allen DB, Tauber M, Christiansen JS, Ambler GR, Battista R, Beauloye V, Berall G, Biller BMK, Butler MG, Cassidy SB, Chihara K, Cohen P, Craig M, Farholt S, Goetghebeur M, Goldstone AP, Greggi T, Grugni G, Hokken-Koelega AC, Johannsson G, Johnson K, Kemper A, Kopchick JJ, Malozowski S, Miller J, Mogul HR, Muscatelli F, Nergårdh R, Nicholls RD, Radovick S, Rosenthal MS, Sipilä I, Tarride J, Vogels A, Waters MJ. Growth hormone research society workshop summary: consensus guidelines for recombinant human growth hormone therapy in Prader–Willi Syndrome. J Clin Endocrinol Metab. 2013;98:E1072–87.
Hegele RA. Familial partial lipodystrophy: a monogenic form of the insulin resistance syndrome. Mol Genet Metab. 2000;71:539–44.
Cochran E, Young JR, Sebring N, DePaoli A, Oral EA, Gorden P. Efficacy of recombinant methionyl human leptin therapy for the extreme insulin resistance of the Rabson–Mendenhall syndrome. J Clin Endocrinol Metab. 2004;89:1548–54.
Parveen BA, Sindhuja R. Rabson-Mendenhall syndrome. Int J Dermatol. 2008;47:839–41.
Bathi RJ, Parveen S, Mutalik S, Rao R. Rabson–Mendenhall syndrome: two case reports and a brief review of the literature. Odontology. 2010;98:89–96.
Torley D, Bellus GA, Munro CS. Genes, growth factors and acanthosis nigricans. Br J Dermatol. 2002;147:1096–101.
Kuzuya H, Matsuura N, Sakamoto M, Makino H, Sakamoto Y, Kadowaki T, Suzuki Y, Kobayashi M, Akazawa Y, Nomura M, Yoshimasa Y, Kasuga M, Goji K, Nagataki S, Oyasu H, Imura H. Trial of insulin like growth factor i therapy for patients with extreme insulin resistance syndromes. Diabetes. 1993;42:696–705.
Elsas LJ, Endo F, Strumlauf E, Elders J, Priest JH. Leprechaunism: an inherited defect in a high-affinity insulin receptor. Am J Hum Genet. 1985;37:73–88.
Nakae J, Kato M, Murashita M, Shinohara N, Tajima T, Fujieda K. Long-term effect of recombinant human insulin-like growth factor I on metabolic and growth control in a patient with leprechaunism. J Clin Endocrinol Metab. 1998;83:542–9.
Acknowledgments
We thank Dr. Alan Shuldiner, Ms. Kathleen Palmer and the Personalized Diabetes Medicine Program (PDMP) staff and participants for making the PDMP and insights gained from it possible.
Disclosure
SA Stein declares no conflicts of interest. KA Maloney declares no conflicts of interest. TI Pollin has received a speaker honorarium and reimbursed travel expenses from the American Diabetes Association.
Human and Animal Rights and Informed Consent
All studies by the authors involving animal and/or human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stein, S.A., Maloney, K.A. & Pollin, T.I. Genetic Counseling for Diabetes Mellitus. Curr Genet Med Rep 2, 56–67 (2014). https://doi.org/10.1007/s40142-014-0039-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40142-014-0039-5