Abstract
Purpose of Review
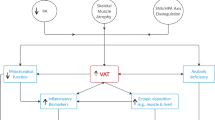
Spinal cord injury (SCI)-induced changes in neurological function have significant impact on the metabolism and subsequent metabolic-related disease risk in injured individuals. Although alterations in body composition, particularly excess adiposity and its anatomical distribution in the visceral depot or ectopic location in nonadipose organs, are known to significantly contribute to metabolic disease risk, changes in fat mass and fat-free mass do not fully account for this elevated disease risk in subjects with SCI.
Recent Findings
There are other negative adaptations in body composition including reductions in skeletal muscle mass and alterations in muscle fiber type, in addition to significant reduction in physical activity, which contribute to a decline in metabolic rate and increased metabolic disease risk following SCI. Recent studies in adult humans suggest that cold- and diet-induced thermogenesis through brown adipose tissue (BAT) metabolism may be important for energy balance and substrate metabolism, and particularly sensitive to sympathetic nervous signaling.
Summary
Considering the physiologic and metabolic phenotypes observed with SCI, particularly across varying anatomic levels, understanding BAT function and impairment with SCI may help improve clinical practice for subjects with SCI while bringing clarity to a broader understanding of the metabolic significance of BAT in adult humans.

Similar content being viewed by others
References
Recently published papers of particular interest have been highlighted as: ∙ Of importance
Spinal cord injury (SCI) facts and figures at a glance. J Spinal Cord Med. 2016;39:243–4. https://www.nscisc.uab.edu/Public/Facts%202015%20Aug.pdf.
Jensen MP, Molton IR, Groah SL, Campbell ML, Charlifue S, Chiodo A, Forchheimer M, Krause JS, Tate D. Secondary health conditions in individuals aging with SCI: terminology, concepts and analytic approaches. Spinal Cord. 2012;50:373–8.
Duckworth WC, Solomon SS, Jallepalli P, Heckemeyer C, Finnern J, Powers A. Glucose intolerance due to insulin resistance in patients with spinal cord injuries. Diabetes. 1980;29:906–10.
Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43:749–56.
Bauman WA, Adkins RH, Spungen AM, Waters RL. The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord. 1999;37:765–71.
• Bauman WA, Spungen AM. Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med. 2001;24:266–77. Demonstrates that when compared with the able-bodied population, people with spinal cord injury are more likely to have oral carbohydrate and lipid disorders which are associated with increased prevalences of diabetes mellitus and cardiovascular disease.
Bauman WA, Spungen AM. Coronary heart disease in individuals with spinal cord injury: assessment of risk factors. Spinal Cord. 2008;46:466–76.
Kressler J, Cowan RE, Bigford GE, Nash MS. Reducing cardiometabolic disease in spinal cord injury. Phys Med Rehabil Clin N Am. 2014;25:573–604, viii.
Banerjea R, Sambamoorthi U, Weaver F, Maney M, Pogach LM, Findley T. Risk of stroke, heart attack, and diabetes complications among veterans with spinal cord injury. Arch Phys Med Rehabil. 2008;89:1448–53.
Bluvshtein V, Korczyn AD, Pinhas I, Vered Y, Gelernter I, Catz A. Insulin resistance in tetraplegia but not in mid-thoracic paraplegia: Is the mid-thoracic spinal cord involved in glucose regulation? Spinal Cord. 2011;49:648–52.
Karlsson AK. Insulin resistance and sympathetic function in high spinal cord injury. Spinal Cord. 1999;37:494–500.
Buchholz AC, Pencharz PB. Energy expenditure in chronic spinal cord injury. Curr Opin Clin Nutr Metab Care. 2004;7:635–9.
Raymond J, Harmer AR, Temesi J, van Kemenade C. Glucose tolerance and physical activity level in people with spinal cord injury. Spinal Cord. 2010;48:591–6.
Schmid A, Halle M, Stutzle C, Konig D, Baumstark MW, Storch MJ, Schmidt-Trucksass A, Lehmann M, Berg A, Keul J. Lipoproteins and free plasma catecholamines in spinal cord injured men with different injury levels. Clin Physiol. 2000;20:304–10.
Monroe MB, Tataranni PA, Pratley R, Manore MM, Skinner JS, Ravussin E. Lower daily energy expenditure as measured by a respiratory chamber in subjects with spinal cord injury compared with control subjects. Am J Clin Nutr. 1998;68:1223–7.
Storch MJ, Konig D, Bultermann D, Blum A, Vogt S, Baumstark M, Berg A, Schmid A. Lipid profile in spinal cord-injured women with different injury levels. Prev Med. 2005;40:321–5.
Myers J, Lee M, Kiratli J. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil. 2007;86:142–52.
Schmid A, Huonker M, Stahl F, Barturen JM, Konig D, Heim M, Lehmann M, Keul J. Free plasma catecholamines in spinal cord injured persons with different injury levels at rest and during exercise. J Auton Nerv Syst. 1998;68:96–100.
Menard MR, Hahn G. Acute and chronic hypothermia in a man with spinal cord injury: environmental and pharmacologic causes. Arch Phys Med Rehabil. 1991;72:421–4.
Colachis SC III. Hypothermia associated with autonomic dysreflexia after traumatic spinal cord injury. Am J Phys Med Rehabil. 2002;81:232–5.
Khan S, Plummer M, Martinez-Arizala A, Banovac K. Hypothermia in patients with chronic spinal cord injury. J Spinal Cord Med. 2007;30:27–30.
Landsberg L, Saville ME, Young JB. Sympathoadrenal system and regulation of thermogenesis. Am J Physiol. 1984;247:E181–9.
Duale H, Hou S, Derbenev AV, Smith BN, Rabchevsky AG. Spinal cord injury reduces the efficacy of pseudorabies virus labeling of sympathetic preganglionic neurons. J Neuropathol Exp Neurol. 2009;68:168–78.
Lucin KM, Sanders VM, Popovich PG. Stress hormones collaborate to induce lymphocyte apoptosis after high level spinal cord injury. J Neurochem. 2009;110:1409–21.
Lucin KM, Sanders VM, Jones TB, Malarkey WB, Popovich PG. Impaired antibody synthesis after spinal cord injury is level dependent and is due to sympathetic nervous system dysregulation. Exp Neurol. 2007;207:75–84.
Attia M, Engel P. Thermoregulatory set point in patients with spinal cord injuries (spinal man). Paraplegia. 1983;21:233–48.
Chu A, Burnham RS. Reliability and validity of tympanic temperature measurement in persons with high spinal cord injuries. Paraplegia. 1995;33:476–9.
Garstang SV, Miller-Smith SA. Autonomic nervous system dysfunction after spinal cord injury. Phys Med Rehabil Clin N Am. 2007;18:275-96.
Hagen EM, Rekand T, Gronning M, Faerestrand S. Cardiovascular complications of spinal cord injury. Tidsskr Nor Laegeforen. 2012;132:1115–20.
Koeppen AH. Subnormal body temperatures in spinal cord injury. Neurology. 1985;35:1259–60.
Taylor RG. Spinal cord injury: its many complications. Am Fam Physician. 1973;8:138–46.
Thijssen DH, Eijsvogels TM, Hesse M, Ballak DB, Atkinson G, Hopman MT. The effects of thoracic and cervical spinal cord lesions on the circadian rhythm of core body temperature. Chronobiol Int. 2011;28:146–54.
Weaver LC, Fleming JC, Mathias CJ, Krassioukov AV. Disordered cardiovascular control after spinal cord injury. Handb Clin Neurol. 2012;109:213–33.
Castro MJ, Apple DF Jr., Staron RS, Campos GE, Dudley GA. Influence of complete spinal cord injury on skeletal muscle within 6 mo of injury. J Appl Physiol. (1985). 1999;86:350–8.
Kocina P. Body composition of spinal cord injured adults. Sports Med. 1997;23:48–60.
Spungen AM, Bauman WA, Wang J, Pierson RN Jr.. Measurement of body fat in individuals with tetraplegia: a comparison of eight clinical methods. Paraplegia. 1995;33:402–8.
Chen Y, Cao Y, Allen V, Richards JS. Weight matters: physical and psychosocial well being of persons with spinal cord injury in relation to body mass index. Arch Phys Med Rehabil. 2011;92:391–8.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond.). 2008;32:959–66.
Gater Jr. DR. Obesity after spinal cord injury. Phys Med Rehabil Clin N Am. 2007;18:333–51, vii.
Gupta N, White KT, Sandford PR. Body mass index in spinal cord injury—a retrospective study. Spinal Cord. 2006;44:92–4.
Yarar-Fisher C, Chen Y, Jackson AB, Hunter GR. Body mass index underestimates adiposity in women with spinal cord injury. Obesity (Silver Spring). 2013;21:1223–5.
Buchholz AC, Bugaresti JM. A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal Cord. 2005;43:513–8.
Laughton GE, Buchholz AC, Martin Ginis KA, Goy RE. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord. 2009;47:757–62.
Edwards LA, Bugaresti JM, Buchholz AC. Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with than in those without spinal cord injury, despite matching waist circumferences. Am J Clin Nutr. 2008;87:600–7.
Gorgey AS, Wells KM, Austin TL. Adiposity and spinal cord injury. World J. Orthop. 2015;6:567–76.
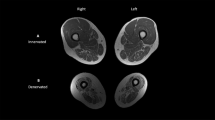
Hu HH, Chen J, Shen W. Segmentation and quantification of adipose tissue by magnetic resonance imaging. MAGMA 2016;29:259–76.
Machann J, Horstmann A, Born M, Hesse S, Hirsch FW. Diagnostic imaging in obesity. Best Pract Res Clin Endocrinol Metab. 2013;27:261–77.
Castro MJ, Apple DF Jr., Hillegass EA, Dudley GA. Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol. 1999;80:373–8.
McCully KK, Mulcahy TK, Ryan TE, Zhao Q. Skeletal muscle metabolism in individuals with spinal cord injury. J Appl Physiol. (1985). 2011;111:143–8.
Bickel CS, Yarar-Fisher C, Mahoney ET, McCully KK. Neuromuscular electrical stimulation-induced resistance training after SCI: a review of the Dudley protocol. Top Spinal Cord Inj Rehabil. 2015;21:294–302.
Breda E, Cavaghan MK, Toffolo G, Polonsky KS, Cobelli C. Oral glucose tolerance test minimal model indexes of beta-cell function and insulin sensitivity. Diabetes. 2001;50:150–8.
Bickel CS, Slade JM, VanHiel LR, Warren GL, Dudley GA. Variable-frequency-train stimulation of skeletal muscle after spinal cord injury. J Rehabil Res Dev. 2004;41:33–40.
Zierath JR, Krook A, Wallberg-Henriksson H. Insulin action in skeletal muscle from patients with NIDDM. Mol Cell Biochem. 1998;182:153–60.
Albers PH, Pedersen AJ, Birk JB, Kristensen DE, Vind BF, Baba O, Nohr J, Hojlund K, Wojtaszewski JF. Human muscle fiber type-specific insulin signaling: impact of obesity and type 2 diabetes. Diabetes. 2015;64:485–97.
Yarar-Fisher C, Bickel CS, Windham ST, McLain AB, Bamman MM. Skeletal muscle signaling associated with impaired glucose tolerance in spinal cord-injured men and the effects of contractile activity. J Appl Physiol. (1985). 2013;115:756–64.
Martinez JA, Fruhbeck G. Regulation of energy balance and adiposity: a model with new approaches. Rev Esp Fisiol. 1996;52:255–8.
Krassioukov AV, Karlsson AK, Wecht JM, Wuermser LA, Mathias CJ, Marino RJ. Assessment of autonomic dysfunction following spinal cord injury: rationale for additions to International Standards for Neurological Assessment. J Rehabil Res Dev. 2007;44:103–12.
Alexander MS, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S, Creasey G, Dietz V, Ditunno J, Donovan W, Elliott SL, Estores I, Graves DE, Green B, Gousse A, Jackson AB, Kennelly M, Karlsson AK, Krassioukov A, Krogh K, Linsenmeyer T, Marino R, Mathias CJ, Perkash I, Sheel AW, Schilero G, Schurch B, Sonksen J, Stiens S, Wecht J, Wuermser LA, Wyndaele JJ. International standards to document remaining autonomic function after spinal cord injury. Spinal Cord. 2009;47:36–43.
Wecht JM, La Fountaine MF, Handrakis JP, West CR, Phillips A, Ditor DS, Sharif H, Bauman WA, Krassioukov AV. Autonomic nervous system dysfunction following spinal cord injury: cardiovascular, cerebrovascular, and thermoregulatory effects. Curr Phys Med Rehabil Rep. 2015;3:197–205.
Cabanac M. Temperature regulation. Annu Rev Physiol. 1975;37:415–39.
Yilmaz B, Yasar E, Goktepe S, Alaca R, Yazicioglu K, Dal U, Mohur H. Basal metabolic rate and autonomic nervous system dysfunction in men with spinal cord injury. Obesity (Silver Spring). 2007;15:2683–7.
Jequier E, Schutz Y. Long-term measurements of energy expenditure in humans using a respiration chamber. Am J Clin Nutr. 1983;38:989–98.
Raven PB, Wilkerson JE, Horvath SM, Bolduan NW. Thermal, metabolic, and cardiovascular responses to various degrees of cold stress. Can J Physiol Pharmacol. 1975;53:293–8.
Dauncey MJ. Influence of mild cold on 24 h energy expenditure, resting metabolism and diet-induced thermogenesis. Br J Nutr. 1981;45:257–67.
van Marken Lichtenbelt WD, Daanen HA. Cold-induced metabolism. Curr Opin Clin Nutr Metab Care. 2003;6:469–75.
van Ooijen AM, van Marken Lichtenbelt WD, van Steenhoven AA, Westerterp KR. Seasonal changes in metabolic and temperature responses to cold air in humans. Physiol Behav. 2004;82:545–53.
Wijers SL, Saris WH, van Marken Lichtenbelt WD. Individual thermogenic responses to mild cold and overfeeding are closely related. J Clin Endocrinol Metab. 2007;92:4299–305.
Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev. 2004;84:277–359.
Steiner G, Loveland M, Schonbaum E. Effect of denervation on brown adipose tissue metabolism. Am J Physiol. 1970;218:566–70.
Mollinger LA, Spurr GB, el Ghatit AZ, Barboriak JJ, Rooney CB, Davidoff DD, Bongard RD. Daily energy expenditure and basal metabolic rates of patients with spinal cord injury. Arch Phys Med Rehabil. 1985;66:420–6.
Alexander LR, Spungen AM, Liu MH, Losada M, Bauman WA. Resting metabolic rate in subjects with paraplegia: the effect of pressure sores. Arch Phys Med Rehabil. 1995;76:819–22.
Jeon JY, Steadward RD, Wheeler GD, Bell G, McCargar L, Harber V. Intact sympathetic nervous system is required for leptin effects on resting metabolic rate in people with spinal cord injury. J Clin Endocrinol Metab. 2003;88:402–7.
Bauman WA, Spungen AM, Wang J, Pierson RN Jr. The relationship between energy expenditure and lean tissue in monozygotic twins discordant for spinal cord injury. J Rehabil Res Dev. 2004;41:1–8.
Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. 2003;77:371–8.
Aksnes AK, Brundin T, Hjeltnes N, Maehlum S, Wahren J. Meal-induced rise in resting energy expenditure in patients with complete cervical spinal cord lesions. Paraplegia. 1993;31:462–72.
Nevin AN, Steenson J, Vivanti A, Hickman IJ. Investigation of measured and predicted resting energy needs in adults after spinal cord injury: a systematic review. Spinal Cord. 2016;54:248–53.
Song YG, Won YH, Park SH, Ko MH, Seo JH. Changes in body temperature in incomplete spinal cord injury by digital infrared thermographic imaging. Ann Rehabil Med. 2015;39:696–704.
Guttmann L, Silver J, Wyndham CH. Thermoregulation in spinal man. J Physiol. 1958;142:406–19.
Downey JA, Chiodi HP, Darling RC. Central temperature regulation in the spinal man. J Appl Physiol. 1967;22:91–4.
Downey JA, Huckaba CE, Myers SJ, Darling RC. Thermoregulation in the spinal man. J Appl Physiol. 1973;34:790–4.
Cinti S. The adipose organ. Prostaglandins Leukot Essent Fatty Acids. 2005;73:9–15.
Cinti S. The role of brown adipose tissue in human obesity. Nutr Metab Cardiovasc Dis. 2006;16:569–74.
Bartness TJ, Vaughan CH, Song CK. Sympathetic and sensory innervation of brown adipose tissue. Int J Obes (Lond.). 2010;34(Suppl 1):S36–42.
Foster DO, Depocas F, Zaror-Behrens G. Unilaterality of the sympathetic innervation of each pad of rat interscapular brown adipose tissue. Can J Physiol Pharmacol. 1982;60:107–13.
Dulloo AG, Miller DS. Energy balance following sympathetic denervation of brown adipose tissue. Can J Physiol Pharmacol. 1984;62:235–40.
Bartness TJ, Wade GN. Effects of interscapular brown adipose tissue denervation on body weight and energy metabolism in ovariectomized and estradiol-treated rats. Behav Neurosci. 1984;98:674–85.
Nedergaard J, Bengtsson T, Cannon B. Three years with adult human brown adipose tissue. Ann NY Acad S Bci. 2010;1212:E20–36.
Cannon B, Nedergaard J. Yes, even human brown fat is on fire! J Clin Investig. 2012;122:486–9.
Cohade C, Mourtzikos KA, Wahl RL. “USA-Fat”: prevalence is related to ambient outdoor temperature-evaluation with 18F-FDG PET/CT. J Nucl Med. 2003;44:1267–70.
Cohade C, Osman M, Pannu HK, Wahl RL. Uptake in supraclavicular area fat (“USA-Fat”): description on 18F-FDG PET/CT. J Nucl Med. 2003;44:170–6.
Lee P, Greenfield JR, Ho KK, Fulham MJ. A critical appraisal of the prevalence and metabolic significance of brown adipose tissue in adult humans. Am J Physiol Endocrinol Metab. 2010;299:E601–6.
Richard D, Monge-Roffarello B, Chechi K, Labbe SM, Turcotte EE. Control and physiological determinants of sympathetically mediated brown adipose tissue thermogenesis. Front Endocrinol (Lausanne). 2012;3:36.
Carey AL, Formosa MF, Van Every EB, Bertovic D, Eikelis N, Lambert GW, Kalff V, Duffy SJ, Cherk MH, Kingwell BA. Ephedrine activates brown adipose tissue in lean but not obese humans. Diabetologia. 2013;56:147–55.
Zingaretti MC, Crosta F, Vitali A, Guerrieri M, Frontini A, Cannon B, Nedergaard J, Cinti S. The presence of UCP1 demonstrates that metabolically active adipose tissue in the neck of adult humans truly represents brown adipose tissue. FASEB J. 2009;23:3113–20.
van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, Drossaerts JM, Kemerink GJ, Bouvy ND, Schrauwen P, Teule GJ. Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009;360:1500–8.
Virtanen KA, Lidell ME, Orava J, Heglind M, Westergren R, Niemi T, Taittonen M, Laine J, Savisto NJ, Enerback S, Nuutila P. Functional brown adipose tissue in healthy adults. N Engl J Med. 2009;360:1518–25.
Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB, Kuo FC, Palmer EL, Tseng YH, Doria A, Kolodny GM, Kahn CR. Identification and importance of brown adipose tissue in adult humans. N Engl J Med. 2009;360:1509–17.
Heaton JM. The distribution of brown adipose tissue in the human. J Anat. 1972;112:35–9.
Nedergaard J, Cannon B. The changed metabolic world with human brown adipose tissue: therapeutic visions. Cell Metab. 2010;11:268–72.
Nedergaard J, Bengtsson T, Cannon B. New powers of brown fat: fighting the metabolic syndrome. Cell Metab. 2011;13:238–40.
Landsberg L, Krieger DR. Obesity, metabolism, and the sympathetic nervous system. Am J Hypertens. 1989;2:125S–32S.
Orava J, Nuutila P, Noponen T, Parkkola R, Viljanen T, Enerback S, Rissanen A, Pietilainen KH, Virtanen KA. Blunted metabolic responses to cold and insulin stimulation in brown adipose tissue of obese humans. Obesity (Silver Spring). 2013;21(11):2279–87.
Vijgen GH, Bouvy ND, Teule GJ, Brans B, Schrauwen P, van Marken Lichtenbelt WD. Brown adipose tissue in morbidly obese subjects. PLoS One. 2011;6:e17247.
• Admiraal WM, Holleman F, Bahler L, Soeters MR, Hoekstra JB, Verberne HJ. Combining 123I-metaiodobenzylguanidine SPECT/CT and 18F-FDG PET/CT for the assessment of brown adipose tissue activity in humans during cold exposure. J Nucl Med. 2013;54:208–12. Demonstrated with imaging modalities a positive correlation between brown adipose tissue activity and sympathetic nervous system markers in cold-stimulated, health human subjects.
Blondin DP, Labbe SM, Christian TH, Noll C, Kunach M, Phoenix S, Guerin B, Turcotte EE, Carpentier AC, Richard D, Haman F. Increased brown adipose tissue oxidative capacity in cold-acclimated humans. J Clin Endocrinol Metab. 2014;99:E438–46.
Chen KY, Brychta RJ, Linderman JD, Smith S, Courville A, Dieckmann W, Herscovitch P, Millo CM, Remaley A, Lee P, Celi FS. Brown fat activation mediates cold-induced thermogenesis in adult humans in response to a mild decrease in ambient temperature. J Clin Endocrinol Metab. 2013;98:E1218–23.
Cypess AM, Chen YC, Sze C, Wang K, English J, Chan O, Holman AR, Tal I, Palmer MR, Kolodny GM, Kahn CR. Cold but not sympathomimetics activates human brown adipose tissue in vivo. Proc Natl Acad Sci USA. 2012;109:10001–5.
Gilsanz V, Smith ML, Goodarzian F, Kim M, Wren TA, Hu HH. Changes in brown adipose tissue in boys and girls during childhood and puberty. J Pediatr. 2012;160:604–9.
Hadi M, Chen CC, Whatley M, Pacak K, Carrasquillo JA. Brown fat imaging with (18)F-6-fluorodopamine PET/CT, (18)F-FDG PET/CT, and (123)I-MIBG SPECT: a study of patients being evaluated for pheochromocytoma. J Nucl Med. 2007;48:1077–83.
• Matsushita M, Yoneshiro T, Aita S, Kameya T, Sugie H, Saito M. Impact of brown adipose tissue on body fatness and glucose metabolism in healthy humans. Int J Obes. (Lond.) 2014;38:812–7. Provides support for the relationship between brown adipose tissue and glucose metabolism in healthy humans.
Nuutila P. Brown adipose tissue thermogenesis in humans. Diabetologia. 2013;56:2110–2.
Saito M, Okamatsu-Ogura Y, Matsushita M, Watanabe K, Yoneshiro T, Nio-Kobayashi J, Iwanaga T, Miyagawa M, Kameya T, Nakada K, Kawai Y, Tsujisaki M. High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes. 2009;58:1526–31.
van Marken LW. Brown adipose tissue and the regulation of nonshivering thermogenesis. Curr Opin Clin Nutr Metab Care. 2012;15:547–52.
van Rooijen BD, van der Lans AA, Brans B, Wildberger JE, Mottaghy FM, Schrauwen P, Backes WH, van Marken Lichtenbelt WD. Imaging cold-activated brown adipose tissue using dynamic T2*-weighted magnetic resonance imaging and 2-deoxy-2-[18F]fluoro-d-glucose positron emission tomography. Investig Radiol. 2013;48:708–14.
Vijgen GH, Bouvy ND, Teule GJ, Brans B, Hoeks J, Schrauwen P, van Marken Lichtenbelt WD. Increase in brown adipose tissue activity after weight loss in morbidly obese subjects. J Clin Endocrinol Metab. 2012;97:E1229–33.
Virtanen KA, van Marken Lichtenbelt WD, Nuutila P. Brown adipose tissue functions in humans. Biochim Biophys Acta. 2013;1831:1004–8.
Yoneshiro T, Aita S, Matsushita M, Kameya T, Nakada K, Kawai Y, Saito M. Brown adipose tissue, whole-body energy expenditure, and thermogenesis in healthy adult men. Obesity (Silver Spring). 2011;19:13–6.
Yoneshiro T, Aita S, Matsushita M, Okamatsu-Ogura Y, Kameya T, Kawai Y, Miyagawa M, Tsujisaki M, Saito M. Age-related decrease in cold-activated brown adipose tissue and accumulation of body fat in healthy humans. Obesity (Silver Spring). 2011;19:1755–60.
Trayhurn P. Brown adipose-tissue—from thermal physiology to bioenergetics. J Biosci. 1993;18:161–73.
Cannon B, Nedergaard J. Metabolic consequences of the presence or absence of the thermogenic capacity of brown adipose tissue in mice (and probably in humans). Int J Obes (Lond.). 2010;34(Suppl 1):S7–16.
Bakker LE, Boon MR, van der Linden RA, Arias-Bouda LP, van Klinken JB, Smit F, Verberne HJ, Jukema JW, Tamsma JT, Havekes LM, van Marken Lichtenbelt WD, Jazet IM, Rensen PC. Brown adipose tissue volume in healthy lean south Asian adults compared with white Caucasians: a prospective, case-controlled observational study. Lancet Diabetes Endocrinol. 2014;2:210–7.
• Hanssen MJ, Wierts R, Hoeks J, Gemmink A, Brans B, Mottaghy FM, Schrauwen P, van Marken Lichtenbelt WD. Glucose uptake in human brown adipose tissue is impaired upon fasting-induced insulin resistance. Diabetologia 2015;58:586–95. Provides support for the relationship between brown adipose tissue function and insulin sensitivity, and its contribution to normothermia under cold exposure.
Raiko J, Holstila M, Virtanen KA, Orava J, Saunavaara V, Niemi T, Laine J, Taittonen M, Borra RJ, Nuutila P, Parkkola R. Brown adipose tissue triglyceride content is associated with decreased insulin sensitivity, independently of age and obesity. Diabetes Obes Metab. 2015;17:516–9.
Zhang Q, Ye H, Miao Q, Zhang Z, Wang Y, Zhu X, Zhang S, Zuo C, Zhang Z, Huang Z, Xue R, Zeng M, Huang H, Jin W, Tang Q, Guan Y, Li Y. Differences in the metabolic status of healthy adults with and without active brown adipose tissue. Wien Klin Wochenschr. 2013;125:687–95.
• Lee P, Smith S, Linderman J, Courville AB, Brychta RJ, Dieckmann W, Werner CD, Chen KY, Celi FS. Temperature-acclimated brown adipose tissue modulates insulin sensitivity in humans. Diabetes 2014;63:3686–98. Provides support for a role of inducible brown adipose tissue in insulin sensitivity and glucose metabolism in healthy adults.
Bray GA. Obesity, a disorder of nutrient partitioning: the MONA LISA hypothesis. J Nutr. 1991;121:1146–62.
Bray GA. Endocrine disturbances and reduced sympathetic activity in the development of obesity. Infusionstherapie. 1990;17:124–30.
Bray GA. Obesity—a state of reduced sympathetic activity and normal or high adrenal activity (the autonomic and adrenal hypothesis revisited). Int J Obes. 1990;14(Suppl 3):77–91.
Astrup A, Andersen T, Christensen NJ, Bulow J, Madsen J, Breum L, Quaade F. Impaired glucose-induced thermogenesis and arterial norepinephrine response persist after weight reduction in obese humans. Am J Clin Nutr. 1990;51:331–7.
Astrup A, Buemann B, Christensen NJ, Madsen J. 24-Hour energy expenditure and sympathetic activity in postobese women consuming a high-carbohydrate diet. Am J Physiol. 1992;262:E282–8.
Astrup AV, Christensen NJ, Breum L. Reduced plasma noradrenaline concentrations in simple-obese and diabetic obese patients. Clin Sci (Lond.). 1991;80:53–8.
Bessard T, Schutz Y, Jequier E. Energy expenditure and postprandial thermogenesis in obese women before and after weight loss. Am J Clin Nutr. 1983;38:680–93.
Jequier E, Schutz Y. New evidence for a thermogenic defect in human obesity. Int J Obes. 1985;9(Suppl 2):1–7.
Jequier E. Carbohydrate-induced thermogenesis in man. Int J Vitam Nutr Res. 1986;56:193–6.
Jequier E. Energy expenditure in obesity. Clin Endocrinol Metab. 1984;13:563–80.
Jequier E, Munger R, Felber JP. Thermogenic effects of various beta-adrenoceptor agonists in humans: their potential usefulness in the treatment of obesity. Am J Clin Nutr. 1992;55:249S–51S.
Schutz Y, Bessard T, Jequier E. Diet-induced thermogenesis measured over a whole day in obese and nonobese women. Am J Clin Nutr. 1984;40:542–52.
Kush RD, Young JB, Katzeff HL, Danforth E Jr., Garrow JS, Scheidegger K, Ravussin E, Howard BV, Sims EA, Horton ES. Effect of diet on energy expenditure and plasma norepinephrine in lean and obese Pima Indians. Metabolism. 1986;35:1110–20.
Lean ME, James WP, Jennings G, Trayhurn P. Brown adipose tissue in patients with phaeochromocytoma. Int J Obes. 1986;10:219–27.
Fukuchi K, Tatsumi M, Ishida Y, Oku N, Hatazawa J, Wahl RL. Radionuclide imaging metabolic activity of brown adipose tissue in a patient with pheochromocytoma. Exp Clin Endocrinol Diabetes. 2004;112:601–3.
Dundamadappa SK, Shankar S, Danrad R, Singh A, Vijayaraghavan G, Kim Y, Perugini R. Imaging of brown fat associated with adrenal pheochromocytoma. Acta Radiol. 2007;48:468–72.
Yamaga LY, Thom AF, Wagner J, Baroni RH, Hidal JT, Funari MG. The effect of catecholamines on the glucose uptake in brown adipose tissue demonstrated by (18)F-FDG PET/CT in a patient with adrenal pheochromocytoma. Eur J Nucl Med Mol Imaging. 2008;35:446–7.
Kuji I, Imabayashi E, Minagawa A, Matsuda H, Miyauchi T. Brown adipose tissue demonstrating intense FDG uptake in a patient with mediastinal pheochromocytoma. Ann Nucl Med. 2008;22:231–5.
Sekizawa N, Yoshimoto T, Izumiyama H, Hirata Y. Distinct uptake of 18F-fluorodeoxyglucose by brown adipose tissue with a catecholamine-secreting tumor. Intern Med. 2010;49:2363.
Wang Q, Zhang M, Ning G, Gu W, Su T, Xu M, Li B, Wang W. Brown adipose tissue in humans is activated by elevated plasma catecholamines levels and is inversely related to central obesity. PLoS One. 2011;6:e21006.
Wallin BG, Stjernberg L. Sympathetic activity in man after spinal cord injury. Outflow to skin below the lesion. Brain. 1984;107(Pt 1):183–98.
Karlsson AK, Attvall S, Jansson PA, Sullivan L, Lonnroth P. Influence of the sympathetic nervous system on insulin sensitivity and adipose tissue metabolism: a study in spinal cord-injured subjects. Metabolism. 1995;44:52–8.
Astrup A. Thermogenesis in human brown adipose tissue and skeletal muscle induced by sympathomimetic stimulation. Acta Endocrinol Suppl (Copenh.). 1986;278:1–32.
van Marken Lichtenbelt WD, Schrauwen P. Implications of nonshivering thermogenesis for energy balance regulation in humans. Am J Physiol Regul Integr Comp Physiol. 2011;301:R285–96.
Jequier E. Thermogenesis induced by nutrients in man: its role in weight regulation. J Physiol (Paris). 1985;80:129–40.
Smith DL Jr., Yang Y, Hu HH, Zhai G, Nagy TR. Measurement of interscapular brown adipose tissue of mice in differentially housed temperatures by chemical-shift-encoded water-fat MRI. J Magn Reson Imaging. 2013;38:1425–33.
Primeaux SD, Tong M, Holmes GM. Effects of chronic spinal cord injury on body weight and body composition in rats fed a standard chow diet. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1102–9.
Acknowledgments
We thank UAB Center for Clinical and Translational Science (1KL2TR001419, Yarar-Fisher) and the University of Alabama at Birmingham. The opinions expressed herein are those of the authors and do not necessarily reflect the official position of any of organization with which they are affiliated.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Daniel L. Smith, Jr. and Ceren Yarar-Fisher declare they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This review article does not contain any new, primary data of studies with human or animal subjects performed by the authors.
Additional information
This article is part of the Topical collection on Spinal Cord Injury Rehabilitation.
Rights and permissions
About this article
Cite this article
Smith, D.L., Yarar-Fisher, C. Contributors to Metabolic Disease Risk Following Spinal Cord Injury. Curr Phys Med Rehabil Rep 4, 190–199 (2016). https://doi.org/10.1007/s40141-016-0124-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-016-0124-7