Abstract
Purpose of Review
This review article summarizes the advantages and potential uses of focused transesophageal echocardiography (TEE) in the perioperative period for trauma patients. We suggest a locally developed TEE protocol for trauma and provide strategies to achieve widespread use of TEE in the anesthesia care of trauma patients.
Recent Findings
In recent years, TEE has gained interest as an additional modality as point-of-care ultrasound (POCUS) for the resuscitation of acutely ill patients in whom transthoracic echocardiography is not feasible or non-diagnostic. Nevertheless, its use among non-cardiac anesthesiologists is still limited compared to the more traditional POCUS applications.
Summary
A goal-directed, focused TEE can be performed at the bedside in different locations and mechanically ventilated patients. TEE provides relevant diagnostic information to guide the resuscitation of acutely injured patients, particularly to identify life-threatening hidden thoracic injuries in the scenario of patients with multi-system trauma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its introduction more than 40 years ago [1], transesophageal echocardiography (TEE) was initially adopted by cardiovascular anesthesiologists for use during cardiovascular surgery. More recently, training programs have expanded to include non-cardiac anesthesiologists and TEE is employed in a number of different clinical settings. Starting a decade ago, point-of-care ultrasound (POCUS) has become even more widespread in perioperative, critical care and other areas of acute care medicine. With respect to trauma, a recent review from Kuo et al. highlights different POCUS applications relevant for the initial management of trauma patients incorporating transthoracic echocardiography (TTE) as the primary modality for focused cardiac ultrasound in POCUS [2].
Nevertheless, it is not a secret that TEE offers many advantages over TTE, particularly in critically ill patients as well as the intraoperative setting [3]. First, the quality of the TTE images can be limited by the positive pressure mechanical ventilation, body habitus, and position with limited access to the chest given the sterility of the surgical field. TEE overcomes most of these challenges, offering improved visualization of cardiac anatomy, hemodynamic assessment, diagnostic accuracy, and real-time assessment during resuscitation. Second, it has a favorable safety profile in critically ill patients [4]. Finally, the images are quick and easy to acquire given the anatomical location. Competency in TEE to perform a successful hemodynamics assessment can be reached after approximately thirty-five examinations, while a minimum of one hundred studies is recommended for advanced TTE [5, 6]. Recently, the use of focused TEE has been demonstrated to be feasible and have a significant clinical impact in the management of patients with undifferentiated shock, acute respiratory failure, and cardiac arrest in the emergency department and the intensive care unit (ICU) [7•, 8, 9]. During the current COVID-19 pandemic, TEE has also been employed in the management of prone patients in the ICU when TTE views cannot be acquired [10].
This review article aims to summarize the role of TEE in the management of acutely injured patients.
TEE in Hemorrhagic Shock
Hemorrhagic shock is common in trauma patients, and its early recognition is fundamental for the outcomes of these patients. TEE is an essential diagnostic tool to help differentiate the etiology of shock. TEE accurately provides valuable real-time information regarding volume status, left ventricle (LV) and right ventricle (RV) function, causes of obstructive shock such as cardiac tamponade or massive pulmonary embolism, evaluation of LV size and filling as well as dynamic evaluation of the superior vena cava (SVC) and inferior vena cava (IVC) to estimate volume status.
There is no general standard definition of hypovolemia in TEE, but a qualitative assessment of the end-diastolic size of the LV in the transgastric short-axis view is commonly accepted in resuscitation TEE. An underfilled LV is identified qualitatively when the papillary muscles touch each other (“kissing papillary muscles”). A retrospective review study by Burns et al. [11] where TEE was performed to optimize the resuscitation of acutely injured patients had demonstrated that 79% of patients had abnormal TEE findings resulting in the change of clinical management in 64%. Of note, ten patients (40%) with signs of hypovolemia by TEE had acceptable pulmonary artery occlusion pressure (PAOP). The most common finding on these patients was hypovolemia (52%) despite vigorous fluid therapy.
Another similar retrospective study by Griffe et al. included trauma patients who underwent a rescue TEE for shock assessment where the most common finding was decreased preload (62%) [12]. In 49% of the patients, there were management changes based on the TEE findings with the most common being a fluid challenge and the second being initiation of inotropic support.
The use of TEE as a hemodynamic monitoring modality (hTEE) has been described in critical care patients who could benefit from continuous TEE monitoring. It offers the advantage of having a smaller probe and more compact monitors than the conventional TEE, which can be left indwelling for 72 h [13•]. The hTEE exam includes three views: the SVC view to assess size and collapsibility, the mid-esophageal four chamber view to assess identification of right and left ventricular size as well as systolic function, and the transgastric short-axis view to assess LV end-diastolic area (LVEDA) and LV contractility. Veillard-Baron et al. [14] found a direct therapeutic impact of hTEE on critical care patient management in 66% of the cases. Currently, there are no studies regarding the use of hTEE in non-ICU patients although it could be a more portable alternative in the perioperative setting. The simplicity of this scanning protocol makes it easy and fast to perform.
TEE in Blunt and Open Chest Trauma
Injury to the heart and great vessels due to blunt chest trauma can be challenging to identify in the critically injured patient that require immediate surgical intervention. Contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) are the traditionally preferred diagnostic modalities for these types of injuries; however, unstable clinical conditions can be a challenge for transportation and positioning required for these studies. The use of POCUS-focused TTE offers the advantage bedside performance, but imaging of aortic injuries can be technically challenging. TEE’s role in diagnosing blunt traumatic aortic injuries (BTAI) has been described for the last two decades, initially by Smith et al., who found a sensitivity of 100% and specificity of 98% for traumatic aortic rupture [15]. A meta-analysis by Shiga et al. found comparable diagnostic accuracy of TEE compared with the cross-sectional imaging modalities with a sensitivity of 98–100% and specificity of 95–98% for the diagnosis of BTAI [16].
Osman et al. [17•] described a case series of five patients where they performed focused TEE in the emergency department trauma room for the evaluation of BTAI in hemodynamically unstable patients. They observed that bedside point-of-care TEE provided relevant clinical information in patients that were not clinically stable to have other diagnostic modalities.
In addition to the diagnosis of BTAI, TEE in blunt trauma is relevant for the diagnosis of other cardiac injuries, such as cardiac rupture [18], papillary muscle avulsion [19], aortic valve rupture [20, 21], and cardiac contusions [22]. Similarly, Artnfield et al. presented a case where bedside TEE was performed by an emergency physician in a trauma patient with evidence of shock of unclear etiology where the TEE demonstrated a significant BTAI with a significant hematoma causing cardiac tamponade physiology [23].
For patients with open chest trauma, there are also case reports highlighting the role of TEE in the diagnosis of intracardiac shunts [24, 25] and identification of fragmented projectiles and their trajectory [26, 27]. Mollod et al. reported a retrospective observational study on sixteen patients with chest trauma, ten with penetrating trauma and six with blunt trauma, where there were a myriad of heart and aortic injuries including proximal aortic rupture, intracardiac nail, aortic transection, flail on the mitral leaflet due to papillary muscle rupture, minor intimal tears to the descending aorta and RV infarction secondary to coronary artery lacerations [28]. Importantly, one of the well-known limitations of TEE is that the distal portion of the ascending aorta is technically challenging to visualize due to the presence of air in the trachea located between the ultrasound probe and these structures. In these cases, a CT would provide better diagnostic information.
TEE in Severe Burn Injury
Critically ill burned patients are a particular subset of acute trauma patients that pose unique clinical challenges in resuscitation and fluid management due to translocations in volume distribution and fluid shifts resulting in severe shock during the acute phase [29]. Several resuscitation strategies based on mathematical models that consider a patient’s weight and burn size have been suggested to determine the amount of fluid required for adequate volume resuscitation although there is still debate on its standardization [30]. Additionally, severe burn patients may present with myocardial dysfunction (both systolic and diastolic) [31, 32] and have a higher risk of infections, sepsis, and infective endocarditis. Patients with severe burns have additional limitations with TTE beyond those previously described. They can have an extensive area of burns, large dressings, and wound grafts that can make TTE technically challenging.
For these reasons, severe burn injury patients are ideal candidates for TEE assessment, both as a diagnostic tool to assess the bi-ventricular function, contractility, and valves and monitoring tool for hemodynamic assessments. It can help with the dynamic assessment to guide volume resuscitation and fluid management in the ICU offering the additional advantage of direct evaluation of cardiac valve competency.
There is limited literature on the role of TEE in critically ill burned patients. In a retrospective study, Etherington et al. presented seventeen patients in a burn center using conventional TEE to assess hypotension and bacteremia [33]. The main findings included hypovolemia, mitral valve vegetations, pulmonary hypertension, pericardial effusion, fluid overload, and RV dysfunction where two patients had changes in their management based on TEE findings.
Of interest, Held et al. performed a retrospective study in a burn intensive care unit using hTEE for monitoring of resuscitation and evaluation of patient’s clinical status [30]. Eleven patients were evaluated with hTEE with cardiac dysfunction identified in seven patients (right ventricular dysfunction in three patients, left ventricular dysfunction in three patients, and biventricular dysfunction in one patient). Three of these patients were found to have hypovolemia despite fluid resuscitation and one was found with fluid overload. The bedside interpretation was made by the critical care physician and reviewed by a cardiac anesthesiologist with good agreement in the results suggesting hTEE can be competently performed at the bedside by trained critical care providers and used as an adjunct during resuscitation of the burn patient.
Finally, it is essential to outweigh the risk vs benefit of TEE probe placement on patients with thermal burns of the mouth and pharynx, potentially leading to bleeding or perforation in edematous tissue [29].
TEE in Cardiac Arrest
POCUS can guide the diagnosis of reversible causes of cardiac arrest like pulmonary embolism and pericardial tamponade [34]. TTE views are limited during cardiac arrest due to the presence of defibrillation pads and continuous compressions that make imaging acquisition challenging. On the contrary, TEE can overcome these limitations. TEE has been reported to be associated with shorter compression pauses during cardiopulmonary resuscitation (CPR) in comparison to TTE for POCUS ultrasonography [35]. TEE provides continuous imaging during resuscitation and gives feedback related to the quality of CPR. During CPR, the mid-esophageal long axis view is recommended to provide real-time feedback of chest compression quality, determine the area of maximal compression, and avoid obstruction of the left ventricle outflow tract that can lead to ineffective compressions [36].
TEE Protocol in Trauma Patients
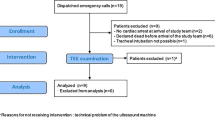
Up to this date, there are very few focused TEE protocols described specifically for trauma patients [13•, 37]. Teranhas described a focused TEE protocol for resuscitation in the emergency department and critical care; it includes four basic TEE views (mid-esophageal four-chamber, mid-esophageal long axis, bi-caval and trans-gastric short axis) that are quick and easy to obtain and interpret during resuscitation [7•]. We suggest using a similar resuscitation TEE approach adapted to fit the specific needs of the unstable trauma patient, including the basic four views with additional views of the ascending and descending aorta and basic Doppler applications (Fig. 1).
Special Considerations of TEE in Trauma Patients
TEE is contraindicated in patients with diagnosed or suspected esophageal injury and should be used with precautions in patients with unstable cervical spine injury [38]; these types of injuries must be ruled out before placing a TEE probe.
It also should be performed with caution (relative contraindication) on patients with severe coagulopathy, history of esophageal disease, recent upper gastrointestinal surgery, severe coagulopathy, and suspected bowel injury or those patients in whom the cervical spine has not been cleared [38]
Conclusions—Is There a Future for the Use of TEE in Trauma Among Non-cardiac Anesthesiologists?
There is no doubt TEE can be a valuable tool for the perioperative management of the acutely injured patient to properly clarify and address the cause of hypotension, guide resuscitation management, and diagnose hidden chest injuries that could explain hemodynamic instability. It offers the additional advantage that it can be done at the bedside; even during surgery, it provides better imaging, especially in mechanically ventilated patients and will be performed and interpreted by the clinician themself (usually the anesthesiologist in the OR or intensivist in the ICU) who will guide resuscitation. It is also essential to recognize and rule out the contraindications and relative contraindications to TEE imaging before performing it. Nevertheless, it is important to point out that TEE, as any ultrasound imaging application in point of care, is operator-dependent and requires formal training and experience to ensure appropriate imaging and diagnosis.
There are indeed some obstacles to overcome if we ever want to see widespread use of TEE in anesthesia practice for the evaluation and management of trauma patients. First, basic TEE training needs to be introduced to non-cardiac anesthesiologists who work in trauma and high complexity centers. This can be accomplished with continuing learning courses, but defined certification objectives must be in-place to maintain hands-on practice and learning curves, especially considering TEE will not be performed regularly by all providers. Also, the teaching of basic TEE concepts during residency training and its use for non-cardiac surgery and the implementation of hands-on training into the POCUS educational program will allow an early introduction of TEE among residents and future anesthesiologists. A study in critical care has shown that TEE is feasible, safe, and effectively performed by fellows and residents within their training with supervision [39]. Trenton et al. reported their 5-year experience on a level I trauma center with TEE performed by critical care and emergency physicians [40]. A structured training and credentialing program was defined with three levels of TEE training (Resuscitative TEE, Basic Critical TEE, and Advanced Critical Care TEE). The number of trained physicians increased over the years with a parallel increase in the number of TEE exams performed. They report a change in management based on TEE in 89% of the cases with a complication rate of only 2%. This experience supports the importance of structured training among physicians and the positive impact in clinical management that can be achieved among critical patients. There is no reason why this cannot be extrapolated to trauma anesthesia care.
The use of simulation in TEE training has been reported among emergency residents in simulated cardiac arrest cases with a high degree of accuracy [41]. Additionally, a 4-h simulator-based course on focused TEE among emergency physicians has proven to be a practical and safe learning method, leading to a success rate of 99.3% in image acquisition during focused TEE in actual patients [42]. Those are promising results and encourage the use of TEE simulation at the introductory course level.
Moreover, with the continuing development of biomedical devices in conjunction with the emerging interest of TEE in different medical fields like anesthesia, critical care, and emergency medicine, it might be possible to have novel and affordable designs of portable TEE ultrasound machines without losing image quality. One example of innovation in this field is the introduction of the hTEE mentioned above, with a more portable device that allows continuous monitoring for up to 72 h in critical care patients [13•].
These types of initiatives could be the start point to expand the role of focused TEE among anesthesiologists. TEE can evolve from being an application primarily used by cardiac anesthesia into a modality as available and popular as other POCUS applications in the trauma patient—helping and guiding in the diagnosis and management of this unique subset of patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Frazin L, Talano JSL. Esophageal echocardiography. Circulation. 1976;54:102–8.
Kuo FH, Baumann HM, d’Empaire PP, Deng Y. Role of Point-of-Care Ultrasound in the Early Stages of Trauma Care. Curr Anesthesiol Rep. 2020;10:69–79.
Vignon P, Merz TM, Vieillard-Baron A. Ten reasons for performing hemodynamic monitoring using transesophageal echocardiography. Intensive Care Med. 2017;43:1048–51.
Jaidka A, Hobbs H, Koenig S, Millington SJ, Arntfield RT. Better with ultrasound: transesophageal echocardiography. Chest. 2019;155:194–201.
Vieillard-Baron A, Mayo PH, Vignon P, et al. International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med. 2014;40:654–66.
Charron C, Vignon P, Prat G, Tonnelier A, Aegerter P, Boles JM, Amiel JB, Vieillard-Baron A. Number of supervised studies required to reach competence in advanced critical care transesophageal echocardiography. Intensive Care Med. 2013;39:1019–24.
• Teran F. Resuscitative cardiopulmonary ultrasound and transesophageal echocardiography in the emergency department. Emerg Med Clin North Am. 2019;37:409–30. This article explains the use of TEE in the emergency department and proposes a focused TEE protocol for emergency physicians. This protocol is the foundation from the trauma protocol we describe in out article.
Teran F, Dean AJ, Centeno C, Panebianco NL, Zeidan AJ, Chan W, Abella BS. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140–7.
Arntfield R, Pace J, Hewak M, Thompson D. Focused transesophageal echocardiography by emergency physicians is feasible and clinically influential: observational results from a novel ultrasound program. J Emerg Med. 2016;50:286–94.
Teran F, Burns KM, Narasimhan M, et al. Critical care transesophageal echocardiography in patients during the COVID-19 pandemic. J Am Soc Echocardiogr. 2020. https://doi.org/10.1016/j.echo.2020.05.022.
Burns JM, Sing RF, Mostafa G, et al. The role of transesophageal echocardiography in optimizing resuscitation in acutely injured patients. J Trauma Inj Infect Crit Care. 2005;59:36–42.
Griffee MJ, Singleton A, Zimmerman JM, Morgan DE, Nirula R. The effect of perioperative rescue transesophageal echocardiography on the management of trauma patients. A A Case Rep. 2016;6:387–90.
• Nowack T, Christie DB. Ultrasound in trauma resuscitation and critical care with hemodynamic transesophageal echocardiography guidance. J Trauma Acute Care Surg. 2019;87:234–9. This article proposes a different protocol for focused TEE and also includes the use of hTEE for continuous evaluation of the patients in the critical care setting.
Vieillard-Baron A, Slama M, Mayo P, Charron C, Amiel JB, Esterez C, Leleu F, Repesse X, Vignon P. A pilot study on safety and clinical utility of a single-use 72-hour indwelling transesophageal echocardiography probe. Intensive Care Med. 2013;39:629–35.
Smith M, Cassidy M, Souther S, Morris E, Sapin P, Johnson S. Transesophageal echocardiography in the diagnosis of traumatic rupture of the aorta. N Engl J Med. 1995;332:356–62.
Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: Systematic review and meta-analysis. Arch Intern Med. 2006;166:1350–6.
• Osman A, Fong CP, Wahab SFA, Panebianco N, Teran F. Transesophageal echocardiography at the golden hour: identification of blunt traumatic aortic injuries in the emergency department. J Emerg Med. 2020;59:418–23. This is one of the most recents articles on the use of TEE in diagnosis of aortic injuries performed by the clinician itself.
Gerlach R, Mark D, Poologaindran A, Tanzola R. Cardiac rupture from blunt chest trauma diagnosed on transesophageal echocardiography. Anesth Analg. 2015;120:293–5.
McCauley R, Shariff F, Steinberg M, Bemenderfer TB, Davis P, Thompson M, Lesh C, Walsh M, Evans E. Blunt thoracic trauma-induced mitral papillary muscle avulsion with pericardial rupture and cardiac herniation: difficult and delayed diagnoses. Case Rep Surg. 2020;2020:1–4.
Zhao QM, Lai LY, He L, Liu F. Case Report: Lessons learned from aortic valve rupture after blunt chest trauma. Front Pediatr. 2021;9:1–6.
de Manna ND, Hoxha S, Cerrito LF, Monica C, Faggian G, Luciani GB. Late aortic valve rupture after blunt chest trauma. Hear Lung Circ. 2020;29:e279–80.
Weiss RL, Brier JA, O’Connor W, Ross S, Brathwaite CM. The usefulness of transesophageal echocardiography in diagnosing cardiac contusions. Chest. 1996;109:73–7.
Landau JH, Power AH, Leeper WR, Arntfield RT. Bedside identification of blunt thoracic aortic injury with point-of-care transesophageal echocardiography. Trauma (United Kingdom). 2016;18:287–90.
Faloye AO, Gershon RY. Traumatic ventricular septal defect after stab wound to the chest missed by transthoracic echocardiography: A case report. 100 Sel Case Reports from Anesth Analg. 2018;9:65–68.
Nandate K, Krishnamoorthy V, McIntyre LK, Verrier ED, Mackensen GB. Gunshot-induced aorto-left atrial fistula diagnosed by intraoperative transesophageal echocardiography. Ann Thorac Surg. 2016;101:771–3.
Goeddel LA, Fraser CD, Daly RJ, Sciortino CM, Sheinberg RB. A bullet in the aortic root: utility of transesophageal echocardiography in penetrating thoracic trauma. Anesth Analg. 2019;129:E69–72.
Imada T, Shibata SC, Sawamizu C, Okitsu K, Iritakenishi T, Fujino Y. Anesthetic management of a crossbow bolt injury to the heart. J Cardiothorac Vasc Anesth. 2018;32:1325–8.
Mollod M, Felner JM. Transesophageal echocardiography in the evaluation of cardiothoracic trauma. Am Heart J. 1996;132:841–9.
Maybauer MO, Asmussen S, Platts DG, Fraser JF, Sanfilippo F, Maybauer DM. Transesophageal echocardiography in the management of burn patients. Burns. 2014;40:630–5.
Held JM, Litt J, Kennedy JD, McGrane S, Gunter OL, Rae L, Kahn SA. Surgeon-performed hemodynamic transesophageal echocardiography in the Burn Intensive Care Unit. J Burn Care Res. 2016;37:e63–8.
Howard TS, Hermann DG, McQuitty AL, Woodson LC, Kramer GC, Herndon DN, Ford PM, Kinsky MP. Burn-induced cardiac dysfunction increases length of stay in pediatric burn patients. J Burn Care Res. 2013;34:413–9.
Kuwagata Y, Sugimoto H, Yoshioka T, Sugimoto T. Left ventricular performance in patients with thermal injury or multiple trauma: a clinical study with echocardiography. J Trauma Inj Infect Crit Care. 1992;32:158–64.
Etherington L, Saffle J, Cochran A. Use of transesophageal echocardiography in burns:a retrospective review. J Burn Care Res. 2010;31:36–9.
Labovitz AJ, Noble VE, Bierig M, Goldstein SA, Jones R, Kort S, Porter TR, Spencer KT, Tayal VS, Wei K. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225–30.
Fair J, Mallin MP, Adler A, Ockerse P, Steenblik J, Tonna J, Youngquist ST. Transesophageal echocardiography during cardiopulmonary resuscitation is associated with shorter compression pauses compared with transthoracic echocardiography. Ann Emerg Med. 2019;73:610–6.
Teran F, Prats MI, Nelson BP, Kessler R, Blaivas M, Peberdy MA, Shillcutt SK, Arntfield RT, Bahner D. Focused transesophageal echocardiography during cardiac arrest resuscitation: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76:745–54.
Leichtle SW, Singleton A, Singh M, Griffee MJ, Tobin JM. Transesophageal echocardiography in the evaluation of the trauma patient: A trauma resuscitation transesophageal echocardiography exam. J Crit Care. 2017;40:202–6.
Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D’Ambra MN, Eltzschig HK. Safety of transesophageal echocardiography. J Am Soc Echocardiogr. 2010;23:1115–27.
Garcia YA, Quintero L, Singh K, Lakticova V, Iakovou AM, Koenig SJ, Narasimhan M, Mayo PH. Feasibility, safety, and utility of advanced critical care transesophageal echocardiography performed by pulmonary/critical care fellows in a medical ICU. Chest. 2017;152:736–41.
Wray TC, Johnson M, Cluff S, et al. Transesophageal echocardiography performed by intensivist and emergency physicians—a 5-year, single-center experience. J Intensive Care Med. 2021. https://doi.org/10.1177/08850666211042522.
Byars DV, Tozer J, Joyce JM, Vitto MJ, Taylor L, Kayagil T, Jones M, Bishop M, Knapp B, Evans D. Emergency physician-performed transesophageal echocardiography in simulated cardiac arrest. West J Emerg Med. 2017;18:830–4.
Reardon RF, Chinn E, Plummer D, et al. Feasibility, utility, and safety of fully incorporating transesophageal echocardiography into emergency medicine practice. Acad Emerg Med. 2021;1–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Laura Giron-Arango and Pablo Perez d’Empaire declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Anesthesia for Trauma
Rights and permissions
About this article
Cite this article
Girón-Arango, L., D’Empaire, P.P. Is There a Role for Transesophageal Echocardiography in the Perioperative Trauma Patient?. Curr Anesthesiol Rep 12, 210–216 (2022). https://doi.org/10.1007/s40140-022-00526-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-022-00526-0