Abstract
Purpose of Review
We will present some relevant concepts on the preoperative evaluation of patients with end-stage liver disease and describe some new intraoperative management strategies for liver transplantation. This review is limited to three topics: cardiac issues, pulmonary issues, and coagulation issues.
Recent Findings
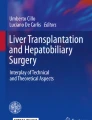
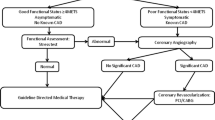
While dobutamine stress echocardiography and myocardial perfusion scintigraphy are the most common screening methods for coronary artery disease, computed tomography techniques are gaining popularity although their value is still unclear. Positive screening tests should be followed by coronary angiography and revascularization. Severe valvular heart disease has to be corrected before transplantation is attempted; percutaneous techniques virtually eliminate the risk of acute hepatic failure frequently associated with cardiopulmonary bypass in patients with severe liver disease. Extracorporeal membrane oxygenation is a viable treatment option when severe pulmonary and cardiac complications develop. Patients with severe hepatopulmonary syndrome can undergo successful liver transplantation, but portopulmonary hypertension remains challenging. Perioperative coagulation management will likely evolve with the availability of prothrombin complex concentrate and fibrinogen concentrate.
Summary
Rather than trying to provide a complete discussion, we emphasize new and interesting findings with significant clinical significance.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fouad TR, Abdel-Razek WM, Burak KW, Bain VG, Lee SS. Prediction of cardiac complications after liver transplantation. Transplantation. 2009;87(5):763–70.
Møller S, Henriksen JH, Bendtsen F. Extrahepatic complications to cirrhosis and portal hypertension: haemodynamic and homeostatic aspects. World J Gastroenterol. 2014;20(42):15499–517.
An J, Shim JH, Kim SO, Kim SO, Lee D, Kim KM, et al. Prevalence and prediction of coronary artery disease in patients with liver cirrhosis: a registry-based matched case-control study. Circulation. 2014;130(16):1353–62.
Di Carli MF, Blankstein R. Low yield of routine preoperative coronary computed tomography angiography in patients evaluated for liver transplantation. Circulation. 2014;130(16):1337–9.
Friedrich-Rust M, Schoetzel F, Maier S, Seeger F, Rey J, Fichtlscherer S, et al. Severity of coronary artery disease is associated with non-alcoholic fatty liver disease: a single-blinded prospective mono-center study. PLoS One. 2017;12(10):e0186720.
Plotkin JS, Scott VL, Pinna A, Dobsch BP, De Wolf AM, Kang Y. Morbidity and mortality in patients with coronary artery disease undergoing orthotopic liver transplantation. Liver Transpl Surg. 1996;2(6):426–30.
Wray C, Scovotti JC, Tobis J, Niemann CU, Planinsic R, Walia A, et al. Liver transplantation outcome in patients with angiographically proven coronary artery disease: a multi-institutional study. Am J Transplant. 2013;13(1):184–91.
Ehtisham J, Altieri M, Salamé E, Saloux E, Ollivier I, Hamon M. Coronary artery disease in orthotopic liver transplantation: pretransplant assessment and management. Liver Transpl. 2010;16(5):550–7.
• Baker S, Chambers C, McQuillan P, Janicki P, Kadry Z, Bowen D, et al. Myocardial perfusion imaging is an effective screening test for coronary artery disease in liver transplant candidates. Clin Transplant. 2015;29(4):319–26. Myocardial perfusion imaging is an acceptable screening test for coronary artery disease in patients with liver disease.
• Choi JM, Kong YG, Kang JW, Kim YK. Coronary computed tomography angiography in combination with coronary artery calcium scoring for the preoperative evaluation of liver transplant recipients. Biomed Res Int. 2017;2017:4081525. These CT-based techniques may have promise in the preoperative screening of liver transplant candidates for coronary artery disease.
Puchner SB, Lu MT, Mayrhofer T, Liu T, Pursnani A, Ghoshhajra BB, et al. High-risk coronary plaque at coronary CT angiography is associated with nonancoholic fatty liver disease, independent of coronary plaque and stenosis burden: results from the ROMICAT II trial. Radiology. 2015;274(3):693–701.
Russo MW, Pierson J, Narang T, Montegudo A, Eskind L, Gulati S. Coronary artery stents and antiplatelet therapy in patients with cirrhosis. J Clin Gastroenterol. 2012;46(4):339–44.
•• Raval Z, Harinstein ME, Flaherty JD. Role of cardiovascular intervention as a bridge to liver transplantation. World J Gastroenterol. 2014;20(31):10651–7. Most cardiology interventions in patients with end-stage liver disease are presented and discussed.
Gopaldas RR, Chu D, Cornwell LD, Dao TK, LeMaire SA, Coselli JS, et al. Cirrhosis as a moderator of outcomes in coronary artery bypass grafting and off-pump coronary artery bypass operations: a 12-year population-based study. Ann Thorac Surg. 2013;96(4):1310–5.
Axelrod D, Koffron AL, DeWolf A, Baker A, Fryer J, Baker T, et al. Safety and efficacy of combined orthotopic liver transplantation and coronary artery bypass grafting. Liver Transpl. 2004;10(11):1386–90.
•• Markin NW, Sharma A, Grant W, Shillcutt SK. The safety of transesophageal echocardiography in patients undergoing orthotopic liver transplantation. J Cardiothor Vasc Anesth. 2015;29(3):588–93. This study confirms that intraoperative transesophageal echocardiography has a low complication rate.
•• Lee M, Weinberg L, Pearce B, Scurrah N, Story DA, Pillai P, et al. Agreement between radial and femoral arterial blood pressure measurements during liver transplantation. Crit Care Resusc. 2015;17(2):101–7. During liver transplantation femoral arterial pressures better reflect central aortic pressure and therefore perfusion pressure of the essential organs as compared to radial arterial pressures.
•• Skaro AI, Gallon LG, Lyuksemburg V, Jay CL, Zhao L, Ladner DP, et al. The impact of coronary artery disease on outcomes after liver transplantation. J Cardiovasc Med. 2016;17(12):875–85. Appropriately treated coronary artery disease is not a contraindication to liver transplantation.
Møller S, Henriksen JH. Cirrhotic cardiomyopathy (review). J Hepatol. 2010;53(1):179–90.
Zardi EM, Zardi DM, Chin D, Sonnino C, Dobrina A, Abbate A. Cirrhotic cardiomyopathy in the pre- and post-liver transplantation phase. (review) J Cardiol. 2016;67(2):125–30.
Saner FH, Neumann T, Canbay A, Treckmann JW, Hartmann M, Goerlinger K, et al. High brain-natriuretic peptide level predicts cirrhotic cardiomyopathy in liver transplant patients. Transpl Int. 2011;24(5):425–32.
• Tandon M, Karna ST, Pandey CK, Chaturvedi R. Diagnostic and Therapeutic challenge of heart failure after liver transplant: case series. World J Hepatol. 2017;9(33):1253–60. Cirrhotic cardiomyopathy remains difficult to diagnose and treat.
Cywinski JB, Argalious M, Marks TN, Parker BM. Dynamic left ventricular outflow tract obstruction in an orthotopic liver transplant recipient. Liver Transpl. 2005;11(6):692–5.
Kia L, Shah SJ, Wang E, Sharma D, Selvaraj S, Medina C, et al. Role of pretransplant echocardiographic evaluation in predicting outcomes following liver transplantation. Am J Transplant. 2013;13(9):2395–401.
Bushyhead D, Kirkpatrick JN, Goldberg D. Pretransplant echocardiographic parameters as markers of posttransplant outcomes in liver transplant recipients. Liver Transpl. 2016;22(3):316–23.
• Araujo L, Dombrovskiy V, Kamran W, Lemaire A, Chiricolo A, Lee LY, et al. The effect of preoperative liver dysfunction on cardiac surgery outcomes. J Cardiothorac Surg. 2017;12(1):73. Cardiac surgery in patients with significant liver disease is associated with a high morbidity and mortality rate.
Filsoufi F, Salzberg SP, Rahmanian PB, Schiano TD, Elsiesy H, Squire A, et al. Early and late outcome of cardiac surgery in patients with liver cirrhosis. Liver Transpl. 2007;13(7):990–5.
Harrison JD, Selzman CH, Thiesset HF, Box T, Hutson WR, Lu JK, et al. Minimally invasive aortic valve replacement with orthotopic liver transplantation: report of a case. Surg Today. 2014;44(3):546–9.
Coverstone E, Korenblat K, Crippin JS, Chapman WC, Kates AM, Zajarias A. Aortic balloon valvuloplasty prior to orthotopic liver transplantation: a novel approach to aortic stenosis and end-stage liver disease. Case Rep Cardiol. 2014;2014:325136.
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597–607.
Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tazcu EM, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015;385(9986):2477–84.
Cabasa AS, Eleid MF, Suri RM. Transcatheter aortic valve replacement for native aortic valve regurgitation as a bridge to liver transplantation. Catheter Cardiovasc Interv. 2016;88(4):665–70.
Maddur H, Bourdillon PD, Liangpunsakul S, Tector AJ, Fridell JA, Ghabril M, et al. Role of cardiac catheterization and percutaneous coronary intervention in the preoperative assessment and management of patients before orthotopic liver transplantation. Liver Transpl. 2014;20(6):664–72.
Moreno R, Delcán JL, García E, Villacastín J, Ortega A, Pérez E. Emergent mitral percutaneous valvuloplasty before emergent liver transplantation. Catheter Cardiovasc Diagn. 1997;41(2):229–30.
Puri R, Abdul-Jawad Altisent O, del Trigo M, Campelo-Parada F, Regueiro A, Barbosa Ribeiro H, et al. Transcatheter mitral valve implantation for inoperable severely calcified native mitral valve disease: a systematic review. Catheter Cardiovasc Interv. 2016;87(3):540–8.
Velazquez EJ, Samad Z, Al-Khalidi HR, Sangli C, Grayburn PA, Massaro JM, et al. The MitraClip and survival in patients with mitral regurgitation at high risk for surgery: a propensity-matched comparison. Am Heart J. 2015;170(5):1050–9.
Kim WR, Lake JR, Smith JM, Skeans MA, Schladt DP, Edwards EB, et al. OPTN/SRTR 2013 annual data report: liver. Am J Transplant. 2015;15:1–28.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2014;64(21):e1–76.
• Bargehr J, Trejo-Gutierrez JF, Patel T, Rosser B, Aranda-Michel J, Yataco ML, et al. Preexisting atrial fibrillation and cardiac complications after liver transplantation. Liver Transpl. 2015;21(3):314–20. Despite a higher perioperative morbidity, atrial fibrillation did not affect overall graft and patient survival.
• Vannucci A, Rathor R, Vachharajani N, Chapman W, Kangrga I. Atrial fibrillation in patients undergoing liver transplantation - a single-center experience. Transplant Proc. 2014;46(5):1432–7. But these authors report a higher postoperative mortality.
• Xia VW, Worapot A, Huang S, Dhillon A, Gudzenko V, Backon A, et al. Postoperative atrial fibrillation in liver transplantation. Am J Transplant. 2015;15(3):687–94. And these authors also found an increased mortality and graft failure with atrial fibrillation.
Fleming GM, Cornell TT, Welling TH, Magee JC, Annich GM. Hepatopulmonary syndrome: use of extracorporeal life support for life-threatening hypoxia following liver transplantation. Liver Transpl. 2008;14(7):966–70.
Monsel A, Mal H, Brisson H, Luo R, Eyraud D, Vézinet C, et al. Extracorporeal membrane oxygenation as a bridge to liver transplantation for acute respiratory distress syndrome-induced life-threatening hypoxaemia aggravated by hepatopulmonary syndrome. Crit Care. 2011;15(5):R234.
Park YH, Hwang S, Park HW, Lee HJ, Namgoong JM, Yoon SY, et al. Effect of pulmonary support using extracorporeal membrane oxygenation for adult liver transplant recipients with respiratory failure. Transplant Proc. 2012;44(3):757–61.
Auzinger G, Willars C, Loveridge R, Best T, Vercueil A, Prachalias A, et al. Extracorporeal membrane oxygenation for refractory hypoxemia after liver transplantation in severe hepatopulmonary syndrome: a solution with pitfalls. Liver Transpl. 2014;20(9):1141–4.
Aufhauser DD Jr, Rose T, Levine M, Barnett R, Ochroch EA, Aukburg S, et al. Cardiac arrest associated with reperfusion of the liver during transplantation: incidence and proposal for a management algorithm. Clin Transpl. 2013;27(2):185–92.
Bittner HB, Binner C, Lehmann S, Kuntze T, Rastan A, Mohr FW. Replacing cardiopulmonary bypass with extracorporeal membrane oxygenation in lung transplantation operations. Eur J Cardiothorac Surg. 2007;31(3):462–7.
Tejani M, Yi SY, Eudailey KW, George I, Guarrera JV, Wagener G. Extracorporeal membrane oxygenation as a rescue device for postreperfusion cardiac arrest during liver transplantation. Liver Transpl. 2015;21(3):410–4.
Pasha AK, Elder MD, Khurram D, Snyder BA, Movahed MR. Successful management of acute massive pulmonary embolism using Angiovac suction catheter technique in a hemodynamically unstable patient. Cardiovasc Revasc Med. 2014;15(4):240–3.
Szocik J, Rudich S, Csete C. ECMO resuscitation after massive pulmonary embolism during liver transplantation. Anesthesiology. 2002;97(3):763–4.
Dell'Amore A, Botta L, Gallieri S, Arpesella G. Extracorporeal membrane oxygenator assistance as “bridge” to combined heart and liver transplantation. Transplant Proc. 2006;38(9):3004–5.
Ceulemans LJ, Vos R, Neyrinck A, Pirenne J, Warnecke G, Van Raemdonck D. Liver-first versus lung-first: a new dilemma in combined organ transplantation. Transpl Int. 2018;31(2):230–1.
Scheiermann P, Czerner S, Kaspar M, Schramm R, Winter H, Wimmer CD, et al. Combined lung and liver transplantation with extracorporeal membrane oxygenation instead of cardiopulmonary bypass. J Cardiothor Vasc Anesth. 2016;30(2):437–42.
• Ravikumar R, Jassem W, Mergental H, Heaton N, Mirza D, Perera MP, et al. Liver transplantation after ex vivo normothermic machine preservation: a phase 1 (first-in-man) clinical trial. Am J Transplant. 2016;16(6):1779–87. Normothermic machine preservation appears to be both safe and feasible.
Schön MR, Kollmar O, Wolf S, Schrem H, Matthes M, Akkoc N, et al. Liver transplantation after organ preservation with normothermic extracorporeal perfusion. Ann Surg. 2001;233(1):114–23.
Foley DP, Fernandez LA, Leverson G, Anderson M, Mezrich J, Sollinger HW, et al. Biliary complications after liver transplantation from donation after cardiac death donors: an analysis of risk factors and long-term outcomes from a single center. Ann Surg. 2011;253(4):817–25.
Shapey IM, Muiesan P. Regional perfusion by extracorporeal membrane oxygenation of abdominal organs from donors after circulatory death: a systematic review. Liver Transpl. 2013;19(12):1292–303.
Pascasio J, Grilo I, López-Pardo F, Ortega-Ruiz F, Tirado JL, Sousa JM, et al. Prevalence and severity of hepatopulmonary syndrome and its influence on survival in cirrhotic patients evaluated for liver transplantation. Am J Transplant. 2014;14(6):1391–9.
•• Krowka MJ, Fallon MB, Kawut SM, Fuhrmann V, Heimbach JK, Ramsay MA, et al. International liver transplant society practice guidelines: diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Transplantation. 2016;100(7):1440–52. A thorough discussion of both pulmonary complications of liver disease.
Saigal S, Choudhary N, Saraf N, Kotecha H, Kakodkar R, Mohanka R, et al. Excellent outcome of living donor liver transplantation in patients with hepatopulmonary syndrome: a single Centre experience. Clin Transpl. 2013;27(4):530–4.
Gupta S, Castel H, Rao RV, Picard M, Lilly L, Faughnan ME, et al. Improved survival after liver transplantation in patients with hepatopulmonary syndrome. Am J Transplant. 2010;10(2):354–63.
Rodriguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome—a liver-induced lung vascular disorder. N Engl J Med. 2008;358(22):2378–87.
• Nayyar D, Man HSJ, Granton J, Lilly LB, Gupta S. Proposed management algorithm for severe hypoxemia after liver transplantation in the hepatopulmonary syndrome. Am J Transplant. 2015;15(4):903–13. Excellent presentation of all treatment options for hepatopulmonary syndrome.
Chihara Y, Egawa H, Tsuboi T, Oga T, Handa T, Yamomoto K, et al. Immediate noninvasive ventilation may improve mortality in patients with hepatopulmonary syndrome after liver transplantation. Liver Transpl. 2011;17(2):144–8.
Udoji TN, Berkowitz DM, Bechara RI, Hanish S, Subramanian RM. The use of transtracheal oxygen therapy in the management of severe hepatopulmonary syndrome after liver transplantation. Transplant Proc. 2013;45(9):3316–9.
Schiffer E, Majno P, Mentha G, Giostra E, Burri H, Klopfenstein CE, et al. Hepatopulmonary syndrome increases the postoperative mortality rate following liver transplantation: a prospective study in 90 patients. Am J Transplant. 2006;6(6):1430–7.
Ramsay M. Portopulmonary hypertension and right heart failure in patients with cirrhosis. Curr Opin Anaesthesiol. 2010;23(2):145–50.
•• Bozbas SS, Bozbas H. Pulmonary hypertension in liver transplant candidates. World J Gastroenterol. 2016;22(6):2024–9. A review article that discusses all aspects of portopulmonary hypertension.
Afifi S, Shayan S, Al-Qamari A. Pulmonary hypertension and right ventricular function: interdependence in pathophysiology and management. Int Anesthesiol Clin. 2009;47(1):97–120.
Paulsen AW, Whitten CW, Ramsay MAE, Klintmalm GB. Considerations for anesthetic management during veno-venous bypass in adult hepatic transplantation. Anesth Analg. 1989;68(4):489–96.
Swanson KL, Wiesner RH, Nyberg SL, Rosen CB, Krowka MJ. Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups. Am J Transplant. 2008;8(11):2445–53.
Burger-Klepp U, Karatosic R, Thum M, Schwarzer R, Fuhrmann V, Hetz H, et al. Transesophageal echocardiography during orthotopic liver transplantation in patients with esophagogastric varices. Transplantation. 2012;94(2):192–6.
Lu SY, Matsusaki T, Abuelkasem E, Sturdevant ML, Humar A, Hilmi IA, et al. Complications related to invasive hemodynamic monitors during adult liver transplantation. Clin Transpl. 2013;27(6):823–8.
•• Pai SL, Aniskevich SIII, Feinglass NG, Ladlie BL, Crawford CC, Peiris P, et al. Complications related to intraoperative transesophageal echocardiography in liver transplantation. SpringerPlus. 2015;4(4):480. TEE is remarkably safe in patients undergoing liver transplantation.
Tripodi A, Salerno F, Chantarangkul V, Clerici M, Cazzaniga M, Primignani M, et al. Evidence of normal thrombin generation in cirrhosis despite abnormal conventional coagulation tests. Hepatology. 2005;41(3):553–8.
Lisman T, Bakhtiari K, Pereboom ITA, Hendriks HGD, Meijers JCM, Porte RJ. Normal to increased thrombin generation in patients undergoing liver transplantation despite prolonged conventional coagulation tests. J Hepatol. 2010;52(3):355–61.
Lisman T, Porte RJ. Rebalanced hemostasis in patients with liver disease: evidence and clinical consequences. Blood. 2010;116(6):878–85.
Warnaar N, Lisman T, Porte RJ. The two tales of coagulation in liver transplantation. Curr Opin Organ Transplant. 2008;13(3):298–303.
• Abuelkasem E, Hasan S, Mazzeffi MA, Planinsic RM, Sakai T, Tanaka KA. Reduced requirement for prothrombin complex concentrate for the restoration of thrombin generation in plasma from liver transplant recipients. Anesth Analg. 2017;125(2):609–15. This work provides further insight into the rebalanced hemostasis in patients with severe liver disease.
Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. 2011;365(2):147–56.
Senzolo M, Rodriguez-Castro KI, Rossetto V, Radu C, Gavasso S, Carraro P, et al. Increased anticoagulant response to low-molecular-weight heparin in plasma from patients with advanced cirrhosis. J Thromb Haemost. 2012;10(9):1823–9.
•• Lisman T, Porte RJ. Value of preoperative hemostasis testing in patients with liver disease for perioperative hemostatic management. Anesthesiology. 2017;126(2):338–44. Routine preoperative coagulation tests poorly predict transfusion requirements.
Cywinski JB, Alster JM, Miller C, Vogt DP, Parker BM. Prediction of intraoperative transfusion requirements during orthotopic liver transplantation and the influence on postoperative patient survival. Anesth Analg. 2014;118(2):428–37.
Findlay JY, Rettke SR. Poor prediction of blood transfusion requirements in adult liver transplantations from preoperative variables. J Clin Anesth. 2000;12(4):319–23.
Massicotte L, Sassine MP, Lenis S, Roy A. Transfusion predictors in liver transplant. Anesth Analg. 2004;98(5):1245–51.
Massicotte L, Thibeault L, Roy A. Classical notions of coagulation revisited in relation with blood losses, transfusion rate for 700 consecutive liver transplantations. Semin Thromb Hemost. 2015;41(5):538–46.
de Boer MT, Molenaar IQ, Hendriks HG, Slooff MJ, Porte RJ. Minimizing blood loss in liver transplantation: progress through research and evolution of techniques. Dig Surg. 2005;22(4):265–75.
Porte RJ, Caldwell SH. The role of recombinant factor VIIa in liver transplantation. Liver Transpl. 2005;11(8):872–4.
Tripodi A, Primignani M, Chantarangkul V, Lemma L, Jovani M, Rebulla P, et al. Global hemostasis tests in patients with cirrhosis before and after prophylactic platelet transfusion. Liver Int. 2013;33(3):362–7.
Tripodi A, Chantarangkul V, Primignani M, Clerici M, Dell’era A, Aghemo A, et al. Thrombin generation in plasma from patients with cirrhosis supplemented with normal plasma: considerations on the efficacy of treatment with fresh-frozen plasma. Intern Emerg Med. 2012;7(2):139–44.
Haas T, Fries D, Tanaka KA, Asmis L, Curry NS, Schöchl H. Usefulness of standard plasma coagulation tests in the management of perioperative coagulopathic bleeding: is there any evidence? Br J Anaesth. 2015;114(2):217–24.
Pustavoitau A, Lesley M, Ariyo P, Latif A, Villamayor AJ, Franks SM, et al. Predictive modeling of massive transfusion requirements during liver transplantation and its potential to reduce utilization of blood bank resources. Anesth Analg. 2017;124(5):1644–52.
Pereboom ITA, de Boer MT, Haagsma EB, Hendriks HGD, Lisman T, Porte RJ. Platelet transfusion during liver transplantation is associated with increased postoperative mortality due to acute lung injury. Anesth Analg. 2009;108(4):1083–91.
de Boer MT, Christensen MC, Asmussen M, van der Hilst CS, Hendriks HG, Slooff MJ, et al. The impact of intraoperative transfusion of platelets and red blood cells on survival after liver transplantation. Anesth Analg. 2008;106(1):32–44.
•• Chin JL, Hisamuddin SH, O’Sullivan A, Chan G, PA MC. Thrombocytopenia, Platelet transfusion, and outcome following liver transplantation. Clin Appl Thromb Hemost. 2016;22(4):351–60. Transfusion of blood products has real consequences.
Toy P, Gajic O, Bacchetti P, Looney MR, Gropper MA, Hubmayr R, et al. Transfusion-related acute lung injury: incidence and risk factors. Blood. 2012;119(7):1757–67.
Wang SC, Shieh JF, Chang KY, Chu YC, Liu CS, Loong CC, et al. Thromboelastography-guided transfusion decreases intraoperative blood transfusion during orthotopic liver transplantation: randomized clinical trial. Transplant Proc. 2010;42(7):2590–3.
Alamo JM, León A, Mellado P, Bernal C, Marín LM, Cepeda C, et al. Is “intra-operating room” thromboelastometry useful in liver transplantation? A case-control study in 303 patients. Transplant Proc. 2013;45(10):3637–9.
Roullet S, Freyburger G, Cruc M, Quinart A, Stecken L, Audy M, et al. Management of bleeding and transfusion during liver transplantation before and after the introduction of a rotational thromboelastometry-based algorithm. Liver Transpl. 2015;21(2):169–79.
Fayed N, Mourad W, Yassen K, Görlinger K. Preoperative thromboelastometry as a predictor of transfusion requirements during adult living donor liver transplantation. Transfus Med Hemother. 2015;42(2):99–108.
Debernardi Venon W, Ponzo P, Sacco M, Mengozzi G, Raso S, Valpreda A, et al. Usefulness of thromboelastometry in predicting the risk of bleeding in cirrhotics who undergo invasive procedures. Eur J Gastroenterol Hepatol. 2015;27(11):1313–9.
De Pietri L, Bianchini M, Montalti R, De Maria N, Di Maira T, Begliomini B, et al. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: a randomized, controlled trial. Hepatology. 2016;63:566–73.
Abuelkasem E, Mazzeffi MA, Lu SY, Planinsic RM, Sakai T, Tanaka KA. Ex-vivo evaluation of 4 different viscoelastic assays for detecting moderate to severe coagulopathy during liver transplantation. Liver Transpl. 2016;22(4):468–75.
Abuelkasem E, Lu S, Tanaka K, Planinsic R, Sakai T. Comparison between thrombelastography and thromboelastometry in hyperfibrinolysis detection during adult liver transplantation. Br J Anaesth. 2016;116(4):507–12.
Müller MCA, Straat M, Meijers JCM, Klinkspoor JH, de Jonge E, Arbous MS, et al. Fresh frozen plasma transfusion fails to influence the hemostatic balance in critically ill patients with a coagulopathy. J Thromb Haemost. 2015;13(6):989–97.
• Marshall AL, Levine M, Howell ML, Chang Y, Riklin E, Parry BA, et al. Dose-associated pulmonary complication rates after fresh frozen plasma administration for warfarin reversal. J Thromb Haemost. 2016;14(2):324–30. Administration of large volumes of fresh frozen plasma can result in volume overload.
Goldstein JN, Refaai MA, Milling TJ Jr, Lewis B, Goldberg-Alberts R, Hug BA, et al. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet. 2015;385(9982):2077–87.
Refaai MA, Goldstein JN, Lee ML, Durn BL, Milling TJ Jr, Sarode R. Increased risk of volume overload with plasma compared with four-factor prothrombin complex concentrate for urgent vitamin K antagonist reversal. Transfusion. 2015;55(11):2722–9.
Lorenz R, Kienast J, Otto U, Egger K, Kiehl M, Schreiter D, et al. Efficacy and safety of a prothrombin complex concentrate with two virus-inactivation steps in patients with severe liver damage. Eur J Gastroenterol Hepatol. 2003;15(1):15–20.
• Kirchner C, Dirkmann D, Treckmann JW, Paul A, Hartmann M, Saner FH, et al. Coagulation management with factor concentrates in liver transplantation: a single-center experience. Transfusion. 2014;54(10):2760–8. Fibrinogen concentrate and prothrombin complex concentrate do not appear to be associated with thrombosis and ischemic events.
Arshad F, Ickx B, van Beem RT, Polak W, Grüne F, Nevens F, et al. Prothrombin complex concentrate in the reduction of blood loss during orthotopic liver transplantation: PROTON-trial. BMC Surg. 2013;13:22.
Karri JV, Cardenas JC, Johansson PI, Matijevic N, Cotton BA, Wade CE, et al. In vitro efficacy of RiaSTAP after rapid reconstitution. J Surg Res. 2014;190(2):655–61.
• Sabate A, Gutierrez R, Beltran J, Mellado P, Blasi A, Acosta F, et al. Impact of preemptive fibrinogen concentrate on transfusion requirements in liver transplantation: a multicenter, randomized, double-blind, placebo-controlled trial. Am J Transplant. 2016;16(8):2421–9. Pre-emptive administration of fibrinogen concentrate did not influence transfusion requirements.
Groeneveld DJ, Adelmeijer J, Hugenholtz GCG, Ariëns RAS, Porte RJ, Lisman T. Ex vivo addition of fibrinogen concentrate improves the fibrin network structure in plasma samples taken during liver transplantation. J Thromb Haemost. 2015;13(12):2192–201.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Joshua Herborn has received speaker’s honoraria from Edwards Lifesciences.
Choy Lewis declares that she has no conflict of interest.
Andre De Wolf declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Transplantation Anesthesia
Rights and permissions
About this article
Cite this article
Herborn, J., Lewis, C. & De Wolf, A. Liver Transplantation: Perioperative Care and Update on Intraoperative Management. Curr Anesthesiol Rep 8, 186–196 (2018). https://doi.org/10.1007/s40140-018-0270-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-018-0270-9