Abstract
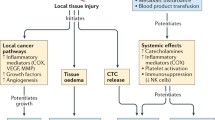
The perioperative period of cancer surgery and its impact on patients’ long-term cancer outcomes is of increasing research interest. The physiological changes coincident with surgery are characterized by a stress response manifesting as activation of inflammatory pathways and immunosuppression. These changes are potentially deleterious to a patient’s capacity to control residual or released tumor cells. Of particular relevance to anesthesiologists is the role of available adjuncts that may offset these changes to improve patients' recovery from surgery and their long-term cancer outcomes. Animal and human evidence indicates a potential therapeutic benefit for β-adrenergic receptor antagonists, selective cyclooxygenase inhibitors, and anti-fibrinolytics administered through the perioperative period. In addition to reducing the surgical stress response, these agents may effect the cancer-host tissue interface to reduce cancer invasion and dissemination. Future research will focus on defining the role of these agents as integral perioperative adjuncts for cancer surgery.

Similar content being viewed by others
Notes
REACT: A phase III multicentre double-blind randomized trial of celecoxib versus placebo in primary breast cancer patients, http://www1.imperial.ac.uk/surgeryandcancer/divisionofcancer/cancer/ccb/iccg/react/.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Marik PE, Zaloga GP. Immunonutrition in high-risk surgical patients: a systematic review and analysis of the literature. J Parenter Enter Nutr. 2010;34:378–86.
Fearon KC, Jenkins JT, Carli F, Lassen K. Patient optimization for gastrointestinal cancer surgery. Br J Surg. 2013;100:15–27.
Sloan EK, Capitanio JP, Tarara RP, Mendoza SP, Mason WA, Cole SW. Social stress enhances sympathetic innervation of primate lymph nodes: mechanisms and implications for viral pathogenesis. J Neurosci. 2007;27:8857–65.
•• Sloan EK, Priceman SJ, Cox BF, Yu S, Pimentel MA, Tangkanangnukul V, et al. The sympathetic nervous system induces a metastatic switch in primary breast cancer. Cancer Res. 2010;70:7042–52. Beta-blocker administration demonstrated a reduction in metastatic burden in mouse model of breast cancer.
Lutgendorf SK, DeGeest K, Sung CY, Arevalo JM, Penedo F, Lucci J, et al. Depression, social support, and beta-adrenergic transcription control in human ovarian cancer. Brain Behav Immun. 2009;23:176–83.
Powe DG, Voss MJ, Zanker KS, Habashy HO, Green AR, Ellis IO, et al. Beta-blocker drug therapy reduces secondary cancer formation in breast cancer and improves cancer specific survival. Oncotarget. 2010;1:628–38.
Benish M, Bartal I, Goldfarb Y, Levi B, Avraham R, Raz A, et al. Perioperative use of beta-blockers and COX-2 inhibitors may improve immune competence and reduce the risk of tumor metastasis. Ann Surg Oncol. 2008;15:2042–52.
Glasner A, Avraham R, Rosenne E, Benish M, Zmora O, Shemer S, et al. Improving survival rates in two models of spontaneous postoperative metastasis in mice by combined administration of a beta-adrenergic antagonist and a cyclooxygenase-2 inhibitor. J Immunol. 2010;184:2449–57.
Akiyoshi S, Mimori K, Sudo T, Tanaka F, Shibata K, Mori M. Laparoscopic surgery minimizes the surgical manipulation of isolated tumor cells leading to decreased metastasis compared to open surgery for colorectal cancer. Surg Today. 2013;43:20–5.
Eguchi H, Ohigashi H, Takahashi H, Yano M, Motoori M, Miyashiro I, et al. Presence of minute cancer cell dissemination in peritoneal lavage fluid detected by reverse transcription PCR is an independent prognostic factor in patients with resectable pancreatic cancer. Surgery. 2009;146:888–95.
Katoh H, Yamashita K, Sato T, Ozawa H, Nakamura T, Watanabe M. Prognostic significance of peritoneal tumour cells identified at surgery for colorectal cancer. Br J Surg. 2009;96:769–77.
Warltier DC, Pagel PS, Kersten JR. Approaches to the prevention of perioperative myocardial ischemia. Anesthesiology. 2000;92:253–9.
Horowitz M, Neeman E, Sharon E, Ben-Eliyahu S. Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat Rev Clin Oncol. 2015;12(4):213–26.
Magnon C, Hall SJ, Lin J, Xue X, Gerber L, Freedland SJ, et al. Autonomic nerve development contributes to prostate cancer progression. Science. 2013;341:1236361.
Shi M, Liu D, Duan H, Qian L, Wang L, Niu L, et al. The β2-adrenergic receptor and Her2 comprise a positive feedback loop in human breast cancer cells. Breast Cancer Res Treat. 2011;125:351–62.
Moretti S, Massi D, Farini V, Baroni G, Parri M, Innocenti S, et al. β-adrenoceptors are upregulated in human melanoma and their activation releases pro-tumorigenic cytokines and metalloproteases in melanoma cell lines. Lab Invest. 2013;93:279–90.
Yang EV, Kim S-J, Donovan EL, Chen M, Gross AC, Webster Marketon JI, et al. Norepinephrine upregulates VEGF, IL-8, and IL-6 expression in human melanoma tumor cell lines: implications for stress-related enhancement of tumor progression. Brain Behav Immun. 2009;23:267–75.
Raju B, Haug SR, Ibrahim SO, Heyeraas KJ. Sympathectomy decreases size and invasiveness of tongue cancer in rats. Neuroscience. 2007;149:715–25.
Raju B, Hultström M, Haug SR, Ibrahim SO, Heyeraas KJ. Sympathectomy suppresses tumor growth and alters gene-expression profiles in rat tongue cancer. Eur J Oral Sci. 2009;117:351–61.
Brown P. Lymphatic system: unlocking the drains. Nature. 2005;436(7050):456–8.
Mallick A, Bodenham AR. Disorders of the lymph circulation: their relevance to anaesthesia and intensive care. Br J Anaesth. 2003;91:265–72.
Solinas G, Germano G, Mantovani A, Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J Leukoc Biol. 2009;86:1065–73.
Schoppmann SF, Birner P, Stöckl J, Kalt R, Ullrich R, Caucig C, et al. Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am J Pathol. 2002;161:947–56.
Thaker PH, Han LY, Kamat AA, Arevalo JM, Takahashi R, Lu C, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12:939–44.
Lutgendorf SK, Cole S, Costanzo E, Bradley S, Coffin J, Jabbari S, et al. Stress-related mediators stimulate vascular endothelial growth factor secretion by two ovarian cancer cell lines. Clin Cancer Res. 2003;9:4514–21.
Bingle L, Brown NJ, Lewis CE. The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J Pathol. 2002;196:254–65.
Schäper J, Wagner A, Enigk F, Brell B, Mousa SA, Habazettl H, et al. Regional sympathetic blockade attenuates activation of intestinal macrophages and reduces gut barrier failure. Anesthesiology. 2013;118:134–42.
•• Hao N-B, Lü M-H, Fan Y-H, Cao Y-L, Zhang Z-R, Yang S-M. Macrophages in tumor microenvironments and the progression of tumors. Clin. Dev. Immunol. 2012;2012:948098. Excellent summary and overview of the role of macrophages in the tumor microenvironment and their sensitivity to hormonal and inflammatory cytokine influences.
Sayfan J, Averbuch F, Koltun L, Benyamin N. Effect of rectal stump washout on the presence of free malignant cells in the rectum during anterior resection for rectal cancer. Dis Colon Rectum. 2000;43:1710–2.
Tvedskov TF, Jensen M-B, Kroman N, Balslev E. Iatrogenic displacement of tumor cells to the sentinel node after surgical excision in primary breast cancer. Breast Cancer Res Treat. 2012;131:223–9.
Sawabata N, Okumura M, Utsumi T, Inoue M, Shiono H, Minami M, et al. Circulating tumor cells in peripheral blood caused by surgical manipulation of non-small-cell lung cancer: pilot study using an immunocytology method. Gen Thorac Cardiovasc Surg. 2007;55:189–92.
Camara O, Kavallaris A, Nöschel H, Rengsberger M, Jörke C, Pachmann K. Seeding of epithelial cells into circulation during surgery for breast cancer: the fate of malignant and benign mobilized cells. World J Surg Oncol. 2006;4:67.
Shakhar G, Ben-Eliyahu S. Potential prophylactic measures against postoperative immunosuppression: could they reduce recurrence rates in oncological patients? Ann Surg Oncol. 2003;10:972–92.
Moore CM, Cross MH, Desborough JP, Burrin JM, Macdonald IA, Hall GM. Hormonal effects of thoracic extradural analgesia for cardiac surgery. Br J Anaesth. 1995;75:387–93.
Moore CM, Desborough JP, Powell H, Burrin JM, Hall GM. Effects of extradural anaesthesia on interleukin-6 and acute phase response to surgery. Br J Anaesth. 1994;72:272–9.
Ahlers O, Nachtigall I, Lenze J, Goldmann A, Schulte E, Höhne C, et al. Intraoperative thoracic epidural anaesthesia attenuates stress-induced immunosuppression in patients undergoing major abdominal surgery. Br J Anaesth. 2008;101:781–7.
Enigk F, Wagner A, Samapati R, Rittner H, Brack A, Mousa SA, et al. Thoracic epidural anesthesia decreases endotoxin-induced endothelial injury. BMC Anesthesiol. 2014;14:23.
Tønnesen E, Wahlgreen C. Influence of extradural and general anaesthesia on natural killer cell activity and lymphocyte subpopulations in patients undergoing hysterectomy. Br J Anaesth. 1988;60:500–7.
Rigg JRA, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, et al. Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet. 2002;359:1276–82.
Biki B, Mascha E, Moriarty DC, Fitzpatrick JM, Sessler DI, Buggy DJ. Anesthetic technique for radical prostatectomy surgery affects cancer recurrence: a retrospective analysis. Anesthesiology. 2008;109:180–7.
Hiller J, Silvers A, McIlroy DR, Niggemeyer L, White S. A retrospective observational study examining the admission arterial to end-tidal carbon dioxide gradient in intubated major trauma patients. Anaesth Intensive Care. 2010;38:302–6.
de Oliveira GSJ, Ahmad S, Schink JC, Singh DK, Fitzgerald PC, McCarthy RJ. Intraoperative neuraxial anesthesia but not postoperative neuraxial analgesia is associated with increased relapse-free survival in ovarian cancer patients after primary cytoreductive surgery. Reg Anesth Pain Med. 2011;36:271–7.
Riedel BJ, Wright IG. Epidural anesthesia in coronary artery bypass grafting surgery. Curr Opin Cardiol. 1997;12:515–21.
Kurosawa S, Matsuzaki G, Harada M, Ando T, Nomoto K. Early appearance and activation of natural killer cells in tumor-infiltrating lymphoid cells during tumor development. Eur J Immunol. 1993;23:1029–33.
Kurosawa S. Anesthesia in patients with cancer disorders. Curr Opin Anaesthesiol. 2012;25:376–84.
Kurosawa S, Harada M, Matsuzaki G, Shinomiya Y, Terao H, Kobayashi N, et al. Early-appearing tumour-infiltrating natural killer cells play a crucial role in the generation of anti-tumour T lymphocytes. Immunology. 1995;85:338–46.
Vallejo R, Hord ED, Barna SA, Santiago-Palma J, Ahmed S. Perioperative immunosuppression in cancer patients. J Environ Pathol Toxicol Oncol. 2003;22:139–46.
Greenfeld K, Avraham R, Benish M, Goldfarb Y, Rosenne E, Shapira Y, et al. Immune suppression while awaiting surgery and following it: dissociations between plasma cytokine levels, their induced production, and NK cell cytotoxicity. Brain Behav Immun. 2007;21:503–13.
Elenkov IJ, Chrousos GP. Stress hormones, proinflammatory and antiinflammatory cytokines, and autoimmunity. Ann N Y Acad Sci. 2002;966:290–303.
Ishikawa M, Nishioka M, Hanaki N, Miyauchi T, Kashiwagi Y, Ioki H, et al. Perioperative immune responses in cancer patients undergoing digestive surgeries. World J Surg Oncol. 2009;7:7.
Zhou D, Gu F-M, Gao Q, Li Q-L, Zhou J, Miao C-H. Effects of anesthetic methods on preserving anti-tumor T-helper polarization following hepatectomy. World J Gastroenterol. 2012;18:3089–98.
Nowarski R, Gagliani N, Huber S, Flavell RA. Innate immune cells in inflammation and cancer. Cancer Immunol Res. 2013;1:77–84.
Dong H, Zhang Y, Xi H. The effects of epidural anaesthesia and analgesia on natural killer cell cytotoxicity and cytokine response in patients with epithelial ovarian cancer undergoing radical resection. J Int Med Res. 2012;40:1822–9.
Rao VSR, Dyer CE, Jameel JKA, Drew PJ, Greenman J. Potential prognostic and therapeutic roles for cytokines in breast cancer (Review). Oncol Rep. 2006;15:179–85.
•• Xu YJ, Chen WK, Zhu Y, Wang SL, Miao CH. Effect of thoracic epidural anaesthesia on serum vascular endothelial growth factor C and cytokines in patients undergoing anaesthesia and surgery for colon cancer. Br J Anaesth. 2014;113(Suppl 1):49–55. Demonstration of the utility of perioperative thoracic epidural analgesia to minimise the surgical stress response and hormones known to stimulate lymphangiogenesis.
Yokoyama M, Itano Y, Katayama H, Morimatsu H, Takeda Y, Takahashi T, et al. The effects of continuous epidural anesthesia and analgesia on stress response and immune function in patients undergoing radical esophagectomy. Anesth Analg. 2005;101:1521–7.
Kawasaki T, Ogata M, Kawasaki C, Okamoto K, Sata T. Effects of epidural anaesthesia on surgical stress-induced immunosuppression during upper abdominal surgery. Br J Anaesth. 2007;98:196–203.
Fant F, Tina E, Sandblom D, Andersson S-O, Magnuson A, Hultgren-Hörnkvist E, et al. Thoracic epidural analgesia inhibits the neuro-hormonal but not the acute inflammatory stress response after radical retropubic prostatectomy. Br J Anaesth. 2013;110(5):747–57.
Volk T, Döpfmer UR, Schmutzler M, Rimpau S, Schnitzler H, Konertz W, et al. Stress induced IL-10 does not seem to be essential for early monocyte deactivation following cardiac surgery. Cytokine. 2003;24:237–43.
Gajewski TF, Schreiber H, Fu Y-X. Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol. 2013;14:1014–22.
Robertson MJ, Ritz J. Biology and clinical relevance of human natural killer cells. Blood. 1990;76:2421–38.
Madden KS, Sanders VM, Felten DL. Catecholamine influences and sympathetic neural modulation of immune responsiveness. Annu Rev Pharmacol Toxicol. 1995;35:417–48.
Ramirez MF, Ai D, Bauer M, Vauthey J-N, Gottumukkala V, Kee S, et al. Innate immune function after breast, lung, and colorectal cancer surgery. J Surg Res. 2015;194:185–93.
Le CP, Karnezis T, Achen MG, Stacker SA, Sloan EK. Lymphovascular and neural regulation of metastasis: shared tumour signalling pathways and novel therapeutic approaches. Best Pract Res Clin Anaesthesiol. 2013;27:409–25.
Melhem-Bertrandt A, Chavez-Macgregor M, Lei X, Brown EN, Lee RT, Meric-Bernstam F, et al. Beta-blocker use is associated with improved relapse-free survival in patients with triple-negative breast cancer. J Clin Oncol. 2011;29:2645–52.
Antoni MH, Lutgendorf SK, Blomberg B, Carver CS, Lechner S, Diaz A, et al. Cognitive-behavioral stress management reverses anxiety-related leukocyte transcriptional dynamics. Biol Psychiatry. 2012;71:366–72.
Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol. 2008;5:466–75.
Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006;24:1105–11.
Lillberg K, Verkasalo PK, Kaprio J, Teppo L, Helenius H, Koskenvuo M. Stressful life events and risk of breast cancer in 10,808 women: a cohort study. Am J Epidemiol. 2003;157:415–23.
Li J, Johansen C, Hansen D, Olsen J. Cancer incidence in parents who lost a child: a nationwide study in Denmark. Cancer. 2002;95:2237–42.
Kvikstad A, Vatten LJ, Tretli S, Kvinnsland S. Widowhood and divorce related to cancer risk in middle-aged women. A nested case-control study among Norwegian women born between 1935 and 1954. Int J Cancer. 1994;58:512–6.
Levav I, Kohn R, Iscovich J, Abramson JH, Tsai WY, Vigdorovich D. Cancer incidence and survival following bereavement. Am J Public Health. 2000;90:1601–7.
Ell K, Nishimoto R, Mediansky L, Mantell J, Hamovitch M. Social relations, social support and survival among patients with cancer. J Psychosom Res. 1992;36:531–41.
Soler-Vila H, Kasl SV, Jones BA. Prognostic significance of psychosocial factors in African-American and white breast cancer patients: a population-based study. Cancer. 2003;98:1299–308.
Barraclough J, Pinder P, Cruddas M, Osmond C, Taylor I, Perry M. Life events and breast cancer prognosis. BMJ. 1992;304:1078–81.
Nelson CJ, Lysle DT. Severity, time, and beta-adrenergic receptor involvement in surgery-induced immune alterations. J Surg Res. 1998;80:115–22.
Woiciechowsky C, Asadullah K, Nestler D, Eberhardt B, Platzer C, Schöning B, et al. Sympathetic activation triggers systemic interleukin-10 release in immunodepression induced by brain injury. Nat Med. 1998;4:808–13.
Oberbeck R, van Griensven M, Nickel E, Tschernig T, Wittwer T, Pape H-C. Influence of beta-adrenoceptor antagonists on hemorrhage-induced cellular immune suppression. Shock. 2002;18:331–5.
Moselli NM, Baricocchi E, Ribero D, Sottile A, Suita L, Debernardi F. Intraoperative epidural analgesia prevents the early proinflammatory response to surgical trauma. Results from a prospective randomized clinical trial of intraoperative epidural versus general analgesia. Ann Surg Oncol. 2011;18:2722–31.
Zaugg M, Tagliente T, Lucchinetti E, Jacobs E, Krol M, Bodian C, et al. Beneficial effects from beta-adrenergic blockade in elderly patients undergoing noncardiac surgery. Anesthesiology. 1999;91:1674–86.
Mostafaie K, Bedenis R, Harrington D. Beta-adrenergic blockers for perioperative cardiac risk reduction in people undergoing vascular surgery. Cochrane Database Syst Rev. 2015;1:CD006342.
Blessberger H, Kammler J, Domanovits H, Schlager O, Wildner B, Azar D, et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2014;9:CD004476.
London MJ, Hur K, Schwartz GG, Henderson WG. Association of perioperative β-blockade with mortality and cardiovascular morbidity following major noncardiac surgery. JAMA. 2013;309:1704–13.
Friedell ML, Van Way CW, Freyberg RW, Almenoff PL. β-blockade and operative mortality in noncardiac surgery: harmful or helpful? JAMA Surg. 2015. doi:https://doi.org/10.1001/jamasurg.2015.86.
POISE Study Group, Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371:1839–47.
Ashes C, Judelman S, Wijeysundera DN, Tait G, Mazer CD, Hare GMT, et al. Selective β1-antagonism with bisoprolol is associated with fewer postoperative strokes than atenolol or metoprolol: a single-center cohort study of 44,092 consecutive patients. Anesthesiology. 2013;119:777–87.
Kalish BT, Kieran MW, Puder M, Panigrahy D. The growing role of eicosanoids in tissue regeneration, repair, and wound healing. Prostaglandins Other Lipid Mediat. 2013;104–105:130–8.
Salvemini D, Kim SF, Mollace V. Reciprocal regulation of the nitric oxide and cyclooxygenase pathway in pathophysiology: relevance and clinical implications. Am J Physiol Regul Integr Comp Physiol. 2013;304:R473–87.
Menter DG, Schilsky RL, DuBois RN. Cyclooxygenase-2 and cancer treatment: understanding the risk should be worth the reward. Clin Cancer Res. 2010;16:1384–90.
Wang D, DuBois RN. Eicosanoids and cancer. Nat Rev Cancer. 2010;10:181–93.
Salvado MD, Alfranca A, Haeggström JZ, Redondo JM. Prostanoids in tumor angiogenesis: therapeutic intervention beyond COX-2. Trends Mol Med. 2012;18:233–43.
Forget P, Tombal B, Scholtes JL, Nzimbala J, Meulders C, Legrand C, et al. Do intraoperative analgesics influence oncological outcomes after radical prostatectomy for prostate cancer? Eur J Anaesthesiol. 2011;28:830–5.
Gottschalk A, Sharma S, Ford J, Durieux ME, Tiouririne M. Review article: the role of the perioperative period in recurrence after cancer surgery. Anesth Analg. 2010;110:1636–43.
Xin X, Majumder M, Girish GV, Mohindra V, Maruyama T, Lala PK. Targeting COX-2 and EP4 to control tumor growth, angiogenesis, lymphangiogenesis and metastasis to the lungs and lymph nodes in a breast cancer model. Lab Invest. 2012;92:1115–28.
Ruan D, So S-P. Prostaglandin E2 produced by inducible COX-2 and mPGES-1 promoting cancer cell proliferation in vitro and in vivo. Life Sci. 2014;116:43–50.
Iwata C, Kano MR, Komuro A, Oka M, Kiyono K, Johansson E, et al. Inhibition of cyclooxygenase-2 suppresses lymph node metastasis via reduction of lymphangiogenesis. Cancer Res. 2007;67:10181–9.
Timoshenko AV, Chakraborty C, Wagner GF, Lala PK. COX-2-mediated stimulation of the lymphangiogenic factor VEGF-C in human breast cancer. Br J Cancer. 2006;94:1154–63.
Sica A, Schioppa T, Mantovani A, Allavena P. Tumour-associated macrophages are a distinct M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. Eur J Cancer. 2006;42:717–27.
Ungefroren H, Sebens S, Seidl D, Lehnert H, Hass R. Interaction of tumor cells with the microenvironment. Cell Commun Signal. 2011;9:18.
Mantovani A, Sica A. Macrophages, innate immunity and cancer: balance, tolerance, and diversity. Curr Opin Immunol. 2010;22:231–7.
•• Karnezis T, Shayan R, Caesar C, Roufail S, Harris NC, Ardipradja K, et al. VEGF-D promotes tumor metastasis by regulating prostaglandins produced by the collecting lymphatic endothelium. Cancer Cell. 2012;21:181–95. Seminal research demonstrating the significance of VEGFD and prostaglandin induced dilation of collecting lymphatic vessels draining malignant tumors. COX-2 inhibitors reduced lymphatic dilation and metastasis.
Karnezis T, Shayan R, Fox S, Achen MG, Stacker SA. The connection between lymphangiogenic signalling and prostaglandin biology: a missing link in the metastatic pathway. Oncotarget. 2012;3:893–906.
Hashimoto I, Kodama J, Seki N, Hongo A, Yoshinouchi M, Okuda H, et al. Vascular endothelial growth factor-C expression and its relationship to pelvic lymph node status in invasive cervical cancer. Br J Cancer. 2001;85:93–7.
Gou H-F, Chen X-C, Zhu J, Jiang M, Yang Y, Cao D, et al. Expressions of COX-2 and VEGF-C in gastric cancer: correlations with lymphangiogenesis and prognostic implications. J Exp Clin Cancer Res. 2011;30:14.
Kopfstein L, Veikkola T, Djonov VG, Baeriswyl V, Schomber T, Strittmatter K, et al. Distinct roles of vascular endothelial growth factor-D in lymphangiogenesis and metastasis. Am J Pathol. 2007;170:1348–61.
Yan M, Myung S-J, Fink SP, Lawrence E, Lutterbaugh J, Yang P, et al. 15-Hydroxyprostaglandin dehydrogenase inactivation as a mechanism of resistance to celecoxib chemoprevention of colon tumors. Proc Natl Acad Sci USA. 2009;106:9409–13.
Song HJ, Myung S-J, Kim I-W, Jeong J-Y, Park YS, Lee SM, et al. 15-hydroxyprostaglandin dehydrogenase is downregulated and exhibits tumor suppressor activity in gastric cancer. Cancer Invest. 2011;29:257–65.
Guo Y-C, Chang C-M, Hsu W-L, Chiu S-J, Tsai Y-T, Chou Y-H, et al. Indomethacin inhibits cancer cell migration via attenuation of cellular calcium mobilization. Molecules. 2013;18:6584–96.
Yoshinaka R, Shibata M-A, Morimoto J, Tanigawa N, Otsuki Y. COX-2 inhibitor celecoxib suppresses tumor growth and lung metastasis of a murine mammary cancer. Anticancer Res. 2006;26:4245–54.
Roche-Nagle G, Connolly EM, Eng M, Bouchier-Hayes DJ, Harmey JH. Antimetastatic activity of a cyclooxygenase-2 inhibitor. Br J Cancer. 2004;91:359–65.
Qadri SSA, Wang J-H, Coffey JC, Alam M, O’Donnell A, Aherne T, et al. Surgically induced accelerated local and distant tumor growth is significantly attenuated by selective COX-2 inhibition. Ann Thorac Surg. 2005;79:990–5 discussion990–5.
Tanaka T, Delong PA, Amin K, Henry A, Kruklitis R, Kapoor V, et al. Treatment of lung cancer using clinically relevant oral doses of the cyclooxygenase-2 inhibitor rofecoxib: potential value as adjuvant therapy after surgery. Ann Surg. 2005;241:168–78.
Fisher JC, Gander JW, Haley MJ, Hernandez SL, Huang J, Chang Y-J, et al. Inhibition of cyclo-oxygenase 2 reduces tumor metastasis and inflammatory signaling during blockade of vascular endothelial growth factor. Vasc Cell. 2011;3:22.
Diperna CA, Bart RD, Sievers EM, Ma Y, Starnes VA, Bremner RM. Cyclooxygenase-2 inhibition decreases primary and metastatic tumor burden in a murine model of orthotopic lung adenocarcinoma. J Thorac Cardiovasc Surg. 2003;126:1129–33.
Zhang M, Xu Z-G, Shi Z, Shao D, Li O, Li W, et al. Inhibitory effect of celecoxib in lung carcinoma by regulation of cyclooxygenase-2/cytosolic phospholipase A2 and peroxisome proliferator-activated receptor gamma. Mol Cell Biochem. 2011;355:233–40.
Frick VO, Justinger C, Rubie C, Graeber S, Schilling MK, Lindemann W. Thoracotomy procedures effect cytokine levels after thoracoabdominal esophagectomy. Oncol Rep. 2012;27:258–64.
Zhao H, Feng Y, Wang Y, Yang B, Xing Z. Comparison of different loading dose of celecoxib on postoperative anti-inflammation and analgesia in patients undergoing endoscopic nasal surgery-200 mg is equivalent to 400 mg. Pain Med. 2011;12:1267–75.
Buvanendran A, Kroin JS, Berger RA, Hallab NJ, Saha C, Negrescu C, et al. Upregulation of prostaglandin E2 and interleukins in the central nervous system and peripheral tissue during and after surgery in humans. Anesthesiology. 2006;104:403–10.
Costa C, Soares R, Reis-Filho JS, Leitão D, Amendoeira I, Schmitt FC. Cyclo-oxygenase 2 expression is associated with angiogenesis and lymph node metastasis in human breast cancer. J Clin Pathol. 2002;55:429–34.
Khuri FR, Wu H, Lee JJ, Kemp BL, Lotan R, Lippman SM, et al. Cyclooxygenase-2 overexpression is a marker of poor prognosis in stage I non-small cell lung cancer. Clin Cancer Res. 2001;7:861–7.
Liu H, Xiao J, Yang Y, Liu Y, Ma R, Li Y, et al. COX-2 expression is correlated with VEGF-C, lymphangiogenesis and lymph node metastasis in human cervical cancer. Microvasc Res. 2011;82:131–40.
Steinbach G, Lynch PM, Phillips RK, Wallace MH, Hawk E, Gordon GB, et al. The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. N Engl J Med. 2000;342:1946–52.
Bertagnolli MM, Eagle CJ, Zauber AG, Redston M, Breazna A, Kim K, et al. Five-year efficacy and safety analysis of the adenoma prevention with celecoxib trial. Cancer Prev Res. 2009;2:310–21.
•• Mao JT, Fishbein MC, Adams B, Roth MD, Goodglick L, Hong L, et al. Celecoxib decreases Ki-67 proliferative index in active smokers. Clin. Cancer Res. 2006;12:314–20. Demonstration, using biomarkers of cell turnover and cancer development, of the chemoprevention role of celecoxib in patients at high risk of developing lung cancer.
Mao JT, Roth MD, Fishbein MC, Aberle DR, Zhang Z-F, Rao JY, et al. Lung cancer chemoprevention with celecoxib in former smokers. Cancer Prev Res. 2011;4:984–93.
Khuri FR. The dawn of a revolution in personalized lung cancer prevention. Cancer Prev Res. 2011;4:949–53.
Slatore CG, Au DH, Littman AJ, Satia JA, White E. Association of nonsteroidal anti-inflammatory drugs with lung cancer: results from a large cohort study. Cancer Epidemiol Biomark Prev. 2009;18:1203–7.
Brabender J, Park J, Metzger R, Schneider PM, Lord RV, Hölscher AH, et al. Prognostic significance of cyclooxygenase 2 mRNA expression in non-small cell lung cancer. Ann Surg. 2002;235:440–3.
Altorki NK, Keresztes RS, Port JL, Libby DM, Korst RJ, Flieder DB, et al. Celecoxib, a selective cyclo-oxygenase-2 inhibitor, enhances the response to preoperative paclitaxel and carboplatin in early-stage non-small-cell lung cancer. J Clin Oncol. 2003;21:2645–50.
Edelman MJ, Watson D, Wang X, Morrison C, Kratzke RA, Jewell S, et al. Eicosanoid modulation in advanced lung cancer: cyclooxygenase-2 expression is a positive predictive factor for celecoxib + chemotherapy–Cancer and Leukemia Group B Trial 30203. J Clin Oncol. 2008;26:848–55.
Groen HJM, Sietsma H, Vincent A, Hochstenbag MMH, van Putten JWG, van den Berg A, et al. Randomized, placebo-controlled phase III study of docetaxel plus carboplatin with celecoxib and cyclooxygenase-2 expression as a biomarker for patients with advanced non-small-cell lung cancer: the NVALT-4 study. J Clin Oncol. 2011;29:4320–6.
Mutter R, Lu B, Carbone DP, Csiki I, Moretti L, Johnson DH, et al. A phase II study of celecoxib in combination with paclitaxel, carboplatin, and radiotherapy for patients with inoperable stage IIIA/B non-small cell lung cancer. Clin Cancer Res. 2009;15:2158–65.
Koch A, Bergman B, Holmberg E, Sederholm C, Ek L, Kosieradzki J, et al. Effect of celecoxib on survival in patients with advanced non-small cell lung cancer: a double blind randomised clinical phase III trial (CYCLUS study) by the Swedish Lung Cancer Study Group. Eur J Cancer. 2011;47:1546–55.
Csiki I. Targeting cyclooxygenase-2 in recurrent non-small cell lung cancer: a phase II trial of celecoxib and docetaxel. Clin Cancer Res. 2005;11:6634–40.
Bar-Yosef S, Melamed R, Page GG, Shakhar G, Shakhar K, Ben-Eliyahu S. Attenuation of the tumor-promoting effect of surgery by spinal blockade in rats. Anesthesiology. 2001;94:1066–73.
Melamed R, Rosenne E, Shakhar K, Schwartz Y, Abudarham N, Ben-Eliyahu S. Marginating pulmonary-NK activity and resistance to experimental tumor metastasis: suppression by surgery and the prophylactic use of a beta-adrenergic antagonist and a prostaglandin synthesis inhibitor. Brain Behav Immun. 2005;19:114–26.
Yakar I, Melamed R, Shakhar G, Shakhar K, Rosenne E, Abudarham N, et al. Prostaglandin e(2) suppresses NK activity in vivo and promotes postoperative tumor metastasis in rats. Ann Surg Oncol. 2003;10:469–79.
Backhus LM, Sievers E, Lin GY, Castanos R, Bart RD, Starnes VA, et al. Perioperative cyclooxygenase 2 inhibition to reduce tumor cell adhesion and metastatic potential of circulating tumor cells in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2006;132:297–303.
Goldfarb Y, Sorski L, Benish M, Levi B, Melamed R, Ben-Eliyahu S. Improving postoperative immune status and resistance to cancer metastasis: a combined perioperative approach of immunostimulation and prevention of excessive surgical stress responses. Ann Surg. 2011;253:798–810.
Retsky M, Rogers R, Demicheli R, Hrushesky WJ, Gukas I, Vaidya JS, et al. NSAID analgesic ketorolac used perioperatively may suppress early breast cancer relapse: particular relevance to triple negative subgroup. Breast Cancer Res. Treat. 2012;134(2):881–8.
Retsky M, Demicheli R, Hrushesky WJ, Forget P, De Kock M, Gukas I, et al. Promising development from translational or perhaps anti-translational research in breast cancer. Clin Transl Med. 2012;1:17.
Demicheli R, Biganzoli E, Boracchi P, Greco M, Retsky MW. Recurrence dynamics does not depend on the recurrence site. Breast Cancer Res. 2008;10:R83.
Demicheli R, Ardoino I, Boracchi P, Lozza L, Biganzoli E. Ipsilateral breast tumour recurrence (IBTR) dynamics in breast conserving treatments with or without radiotherapy. Int J Radiat Biol. 2010;86:542–7.
Forget P, Vandenhende J, Berliere M, Machiels J-P, Nussbaum B, Legrand C, et al. Do intraoperative analgesics influence breast cancer recurrence after mastectomy? A retrospective analysis. Anesth Analg. 2010;110:1630–5.
Forget P, Bentin C, Machiels JP, Berliere M, Coulie PG, De Kock M. Intraoperative use of ketorolac or diclofenac is associated with improved disease-free survival and overall survival in conservative breast cancer surgery. Br J Anaesth. 2014;113(Suppl 1):i82–7.
Zhu Y, Wang S, Wu H, Wu Y. Effect of perioperative parecoxib on postoperative pain and local inflammation factors PGE2 and IL-6 for total knee arthroplasty: a randomized, double-blind, placebo-controlled study. Eur J Orthop Surg Traumatol. 2013;24(3):395–401.
O’Riain SC, Buggy DJ, Kerin MJ, Watson RW, Moriarty DC. Inhibition of the stress response to breast cancer surgery by regional anesthesia and analgesia does not affect vascular endothelial growth factor and prostaglandin E2. Anesth Analg. 2005;100:244–9.
Wu Q, Purusram G, Wang H, Yuan R, Xie W, Gui P, et al. The efficacy of parecoxib on systemic inflammatory response associated with cardiopulmonary bypass during cardiac surgery. Br J Clin Pharmacol. 2013;75:769–78.
Wattchow DA, De Fontgalland D, Bampton PA, Leach PL, McLaughlin K, Costa M. Clinical trial: the impact of cyclooxygenase inhibitors on gastrointestinal recovery after major surgery—a randomized double blind controlled trial of celecoxib or diclofenac vs. placebo. Aliment Pharmacol Ther. 2009;30:987–98.
Ng A, Smith G, Davidson AC. Analgesic effects of parecoxib following total abdominal hysterectomy. Br J Anaesth. 2003;90:746–9.
Riest G, Peters J, Weiss M, Dreyer S, Klassen PD, Stegen B, et al. Preventive effects of perioperative parecoxib on post-discectomy pain. Br J Anaesth. 2008;100:256–62.
Dhawan D, Craig BA, Cheng L, Snyder PW, Mohammed SI, Stewart JC, et al. Effects of short-term celecoxib treatment in patients with invasive transitional cell carcinoma of the urinary bladder. Mol Cancer Ther. 2010;9:1371–7.
Sooriakumaran P, Coley HM, Fox SB, Macanas-Pirard P, Lovell DP, Henderson A, et al. A randomized controlled trial investigating the effects of celecoxib in patients with localized prostate cancer. Anticancer Res. 2009;29:1483–8.
Liu J-F, Zhang S-W, Jamieson GG, Zhu G-J, Wu T-C, Zhu T-N, et al. The effects of a COX-2 inhibitor meloxicam on squamous cell carcinoma of the esophagus in vivo. Int J Cancer. 2008;122:1639–44.
Liu J-F, Jamieson GG, Wu T-C, Zhu G-J, Drew PA. A preliminary study on the postoperative survival of patients given aspirin after resection for squamous cell carcinoma of the esophagus or adenocarcinoma of the cardia. Ann Surg Oncol. 2009;16:1397–402.
ADAPT Research Group. Cardiovascular and cerebrovascular events in the randomized, controlled Alzheimer’s disease anti-inflammatory prevention trial (ADAPT). PLoS Clin Trials. 2006;1:e33.
Joshi GP, Gertler R, Fricker R. Cardiovascular thromboembolic adverse effects associated with cyclooxygenase-2 selective inhibitors and nonselective antiinflammatory drugs. Anesth Analg. 2007;105:1793–804 tableofcontents.
Huang Y-M, Wang C-M, Wang C-T, Lin W-P, Horng L-C, Jiang C-C. Perioperative celecoxib administration for pain management after total knee arthroplasty—a randomized, controlled study. BMC Musculoskelet Disord. 2008;9:77.
STARSurg Collaborative. Impact of postoperative non-steroidal anti-inflammatory drugs on adverse events after gastrointestinal surgery. Br J Surg. 2014;101:1413–23.
Lentschener C, Benhamou D, Mercier FJ, Boyer-Neumann C, Naveau S, Smadja C, et al. Aprotinin reduces blood loss in patients undergoing elective liver resection. Anesth Analg. 1997;84:875–81.
Lentschener C, Cottin P, Bouaziz H, Mercier FJ, Wolf M, Aljabi Y, et al. Reduction of blood loss and transfusion requirement by aprotinin in posterior lumbar spine fusion. Anesth Analg. 1999;89:590–7.
Fergusson DA, Hébert PC, Mazer CD, Fremes S, MacAdams C, Murkin JM, et al. A comparison of aprotinin and lysine analogues in high-risk cardiac surgery. N Engl J Med. 2008;358:2319–31.
Putnam JB, Royston D, Chambers AF, Dunbar S, Lemmer JH, Norman P, et al. Evaluating the role of serine protease inhibition in the management of tumor micrometastases. Oncology. 2003;17:9–30 quiz 31–2.
Mignatti P, Rifkin DB. Biology and biochemistry of proteinases in tumor invasion. Physiol Rev. 1993;73:161–95.
Tengborn L, Blombäck M, Berntorp E. Tranexamic acid—an old drug still going strong and making a revival. Thromb Res. 2014;135(2):231–42.
Vaporciyan AA, Putnam JB, Smythe WR. The potential role of aprotinin in the perioperative management of malignant tumors. J Am Coll Surg. 2004;198:266–78.
McCormack PL. Tranexamic acid: a review of its use in the treatment of hyperfibrinolysis. Drugs. 2012;72:585–617.
Latner AL, Longstaff E, Pradhan K. Inhibition of malignant cell invasion in vitro by a proteinase inhibitor. Br J Cancer. 1973;27:460–4.
Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9:239–52.
Dohadwala M, Batra RK, Luo J, Lin Y, Krysan K, Pold M, et al. Autocrine/paracrine prostaglandin E2 production by non-small cell lung cancer cells regulates matrix metalloproteinase-2 and CD44 in cyclooxygenase-2-dependent invasion. J Biol Chem. 2002;277:50828–33.
Stonelake PS, Jones CE, Neoptolemos JP, Baker PR. Proteinase inhibitors reduce basement membrane degradation by human breast cancer cell lines. Br J Cancer. 1997;75:951–9.
Suojanen J, Sorsa T, Salo T. Tranexamic acid can inhibit tongue squamous cell carcinoma invasion in vitro. Oral Dis. 2009;15:170–5.
•• Afsharimani B, Cabot PJ, Parat M-O. Effect of lysine antifibrinolytics and cyclooxygenase inhibitors on the proteolytic profile of breast cancer cells interacting with macrophages or endothelial cells. Br J Anaesth. 2014;113 Suppl 1:i22–i31. Demonstration of the role of anti-fibrinolytic agents to regulate the tumor microenvironment of breast cancer principally through matrix metalloproteinases and their tissue inhibitors.
Noriyuki M, Sumi T, Zhi X, Misugi F, Nobeyama H, Yoshida H, et al. Vascular endothelial growth factor, matrix metalloproteinases, and cyclooxygenase-2 influence prognosis of uterine cervical cancer in young women. Int. J. Oncol. 2007;31:531–6.
Perides G, Zhuge Y, Lin T, Stins MF, Bronson RT, Wu JK. The fibrinolytic system facilitates tumor cell migration across the blood-brain barrier in experimental melanoma brain metastasis. BMC Cancer. 2006;6:56.
Syrovets T, Simmet T. Novel aspects and new roles for the serine protease plasmin. Cell Mol Life Sci. 2004;61:873–85.
Peterson HI, Risberg B. Experimental studies on the effect of induced antifibrinolysis on per-operative tumour cell shedding. Z Krebsforsch Klin Onkol Cancer Res Clin Oncol. 1976;86:121–5.
Turner GA, Weiss L. Analysis of aprotinin-induced enhancement of metastasis of Lewis lung tumors in mice. Cancer Res. 1981;41:2576–80.
Uetsuji S, Yamamura M, Takai S, Hioki K, Yamamoto M. Effect of aprotinin on metastasis of Lewis lung tumor in mice. Surg Today. 1992;22:439–42.
Sawaya R, Mandybur T, Ormsby I, Tew JM. Antifibrinolytic therapy of experimentally grown malignant brain tumors. J Neurosurg. 1986;64:263–8.
Kirstein JM, Graham KC, Mackenzie LT, Johnston DE, Martin LJ, Tuck AB, et al. Effect of anti-fibrinolytic therapy on experimental melanoma metastasis. Clin Exp Metastasis. 2009;26:121–31.
Porta Della P, Soeltl R, Krell HW, Collins K, O’Donoghue M, Schmitt M, et al. Combined treatment with serine protease inhibitor aprotinin and matrix metalloproteinase inhibitor Batimastat (BB-94) does not prevent invasion of human esophageal and ovarian carcinoma cells in vivo. Anticancer Res. 1999;19:3809–16.
Dunbar SD, Ornstein DL, Zacharski LR. Cancer treatment with inhibitors of urokinase-type plasminogen activator and plasmin. Expert Opin Investig Drugs. 2000;9:2085–92.
Norman PH, Thall PF, Purugganan RV, Riedel BJCJ, Thakar DR, Rice DC, et al. A possible association between aprotinin and improved survival after radical surgery for mesothelioma. Cancer. 2009;115:833–41.
Mikhalkin IA, Iashvili ZG, Bykov VL. Thermoradiotherapy combined with a proteolysis inhibitor (contrical) in the treatment of head and neck cancer. Oncology. 1993;50:344–7.
Ulisse S, Baldini E, Sorrenti S, D’Armiento M. The urokinase plasminogen activator system: a target for anti-cancer therapy. Curr Cancer Drug Targets. 2009;9:32–71.
Acknowledgments
Jonathan G. Hiller and Marie-Odile Parat are the recipients of an Australian and New Zealand College of Anaesthetists Investigator Grant 13/002 and Project Grant 14/020, respectively. Dr. Bernhard Riedel wishes to thank Drs. Donal Buggy, Vijaya Gottumukkala, and Erica Sloan for their kind assistance in the development of this issue and the reviewing of the articles.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cancer Anesthesia.
Rights and permissions
About this article
Cite this article
Hiller, J.G., Parat, MO. & Ben-Eliyahu, S. The Role of Perioperative Pharmacological Adjuncts in Cancer Outcomes: Beta-Adrenergic Receptor Antagonists, NSAIDs and Anti-fibrinolytics. Curr Anesthesiol Rep 5, 291–304 (2015). https://doi.org/10.1007/s40140-015-0113-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-015-0113-x