Abstract
Purpose of Review
Our objective is to review important and recent clinical trials of systemic and local thrombolysis for acute venous thromboembolism (VTE).
Recent Findings
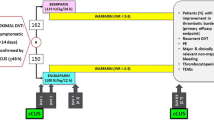
While anticoagulation is the cornerstone of VTE treatment, systemic thrombolysis is recommended for the highest risk pulmonary embolism (PE) patients who present with hypotension and also have a low bleeding risk. Utilization of low-dose, catheter-directed thrombolytic administration with or without ultrasound energy may minimize bleeding risk beyond systemic thrombolysis.
Summary
Venous thromboembolism (VTE), including deep-vein thrombosis (DVT) and pulmonary embolism (PE), is a common cardiovascular disease. Current guidelines recommend anticoagulation over catheter-directed thrombolysis in acute DVT primarily due to the limitations of available data. Clinical trial information is conflicting on whether catheter-directed thrombolysis reduces rates of post-thrombotic syndrome and improves rates of vessel patency. Stability data on alteplase in the catheter-directed setting are limited. Our mass spectrometry analysis indicates that a wide range of alteplase concentrations are stable for at least 24 h. These data can reassure pharmacists, nurses, and physicians that alteplase remains stable during infusion durations utilized in catheter-directed thrombolysis. Individual facilities can tailor their alteplase preparation to meet their own institutional needs.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–603.
Goldhaber SZ. Venous thromboembolism: epidemiology and magnitude of the problem. Best Pract Res Clin Haematol. 2012;25(3):235–42.
Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 SUPPL):419–96.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315–52.
Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379:1835–46. https://doi.org/10.1016/S0140-6736(11)61904-1.
Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med. 2014;370:1402–11. https://doi.org/10.1056/NEJMoa1302097.
Kline JA, Nordenholz KE, Courtney DM, Kabrhel C, Jones AE, Rondina MT, et al. Treatment of submassive pulmonary embolism with tenecteplase or placebo: cardiopulmonary outcomes at 3 months: multicenter double-blind, placebo-controlled randomized trial. J Thromb Haemost. 2014;12(4):459–68. https://doi.org/10.1111/jth.12521.
Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” trial). Am J Cardiol. 2013;111(2):273–7. https://doi.org/10.1016/j.amjcard.2012.09.027.
•• Piazza G, Hohlfelder B, Jaff MR, et al. A prospective, single-arm, multicenter trial of ultrasound-facilitated, catheter-directed, low-dose fibrinolysis for acute massive and submassive pulmonary embolism. JACC Cardiovasc Interv. 2015;8(10):1382–92. This study demonstrated the effects of ultrasound-facilitated, catheter-directed thrombolysis on pulmonary artery pressures in patients with acute pulmonary embolism
Engelberger RP, Kucher N. Ultrasound-assisted thrombolysis for acute pulmonary embolism: a systematic review. Eur Heart J. 2014;35(12):758–64.
Tapson V, Piazza G, Sterling K, Ouriel K, Liu P, Goldhaber S. Optimum duration and dose of r-tPA with the acoustic pulse thrombolysis procedure for submassive pulmonary embolism: OPTALYSE PE. Am J Respir Crit Care Med. 2017;195:A2835.
Elsharawy M, Elzayat E. Early results of thrombolysis vs anticoagulation in iliofemoral venous thrombosis. A randomised clinical trial. Eur J Vasc Endovasc Surg. 2002;24(3):209–14. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12217281. Accessed August 19, 2017
• Haig Y, Enden T, Grøtta O, Kløw NE, Slagsvold CE, Ghanima W, et al. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. Lancet Haematol. 2016;3(2):e64–71. https://doi.org/10.1016/S2352-3026(15)00248-3. This long-term follow-up study supports a significant benefit with respect to post-thrombotic syndrome for catheter-directed thrombolysis in the routine management of proximal deep-vein thrombosis
Enden T, Haig Y, Kløw N-E, Slagsvold CE, Sandvik L, Ghanima W, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet. 2012;379(9810):31–8. https://doi.org/10.1016/S0140-6736(11)61753-4.
Society of Interventional Radiology. ATTRACT Trial results provide insight into DVT therapy. 2017. Available at: http://www.sirtoday.org/attract-study/. Accessed 10 Sept 2017.
Activase. 2017. Available at: https://www.gene.com/download/pdf/activase_prescribing.pdf.
Chamsuddin A, Nazzal L, Kang B, Best I, Peters G, Panah S, et al. Catheter-directed thrombolysis with the Endowave system in the treatment of acute massive pulmonary embolism: a retrospective multicenter case series. J Vasc Interv Radiol. 2008;19(3):372–6.
Lin PH, Annambhotla S, Bechara CF, Athamneh H, Weakley SM, Kobayashi K, et al. Comparison of percutaneous ultrasound-accelerated thrombolysis versus catheter-directed thrombolysis in patients with acute massive pulmonary embolism. Vascular. 2009;17(Suppl 3):S137–47.
Engelhardt TC, Taylor AJ, Simprini LA, Kucher N. Catheter-directed ultrasound-accelerated thrombolysis for the treatment of acute pulmonary embolism. Thromb Res. 2011;128(2):149–54.
Kennedy RJ, Kenney HH, Dunfee BL. Thrombus resolution and hemodynamic recovery using ultrasound-accelerated thrombolysis in acute pulmonary embolism. J Vasc Interv Radiol. 2013;24(6):841–8.
Engelberger RP, Moschovitis A, Fahrni J, Willenberg T, Baumann F, Diehm N, et al. Fixed low-dose ultrasound-assisted catheter-directed thrombolysis for intermediate- and high-risk pulmonary embolism. Eur Heart J. 2013;36(10):597–604.
Quintana D, Salsamendi J, Fourzali R, Narayanan G. Ultrasound-assisted thrombolysis in submassive and massive pulmonary embolism: assessment of lung obstruction before and after catheter-directed therapy. Cardiovasc Intervent Radiol. 2014;37(2):420–6.
Kucher N, Boekstegers P, Müller OJ, et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014;129(4):479–86.
Siddiqi F, Odrljin TM, Fay PJ, Cox C, Francis CW. Binding of tissue-plasminogen activator to fibrin: effect of ultrasound. Blood. 1998;91(6):2019–25.
Soltani A, Prokop AF, Vaezy S. Stability of alteplase in presence of cavitation. Ultrasonics. 2008;48(2):109–16.
Soltani A, Soliday C. Effect of ultrasound on enzymatic activity of selected plasminogen activators. Thromb Res. 2007;119(2):223–8.
De Somer F, Van Landschoot A, Van Nooten G, Delanghe J. Interaction of plasma proteins with commercial protein repellent polyvinyl chloride (PVC): a word of caution. Perfusion. 2008;23(4):215–21. https://doi.org/10.1177/0267659108099814.
Funding
No specific funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
John Fanikos reports consultancy activities for Genentech, Inc. Gregory Piazza reports receipt of grants from BTG Interventional Medicine Ltd. Samuel Goldhaber reports grants from BTG/EKOS, BiO2 Medical, Boehringer Ingelheim, BMS, Daiichi, Janssen, personal fees from Agile, Bayer, Boehringer Ingelheim, BMS, Daiichi, eXIthera, Janssen, Portola, and Soleno.
Additional information
This article is part of the Topical Collection on Pharmacology Care
Rights and permissions
About this article
Cite this article
Hohlfelder, B., Marquis, K., Fanikos, J. et al. A Review of Thrombolysis in Venous Thromboembolism With an Analysis of Alteplase Admixture Stability. Curr Emerg Hosp Med Rep 6, 54–61 (2018). https://doi.org/10.1007/s40138-018-0156-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-018-0156-7