Abstract
Purpose of Review
This review provides in-depth insight into the recently published literature surrounding two new heart failure therapies, sacubitril/valsartan and ivabradine.
Recent Findings
Significant literature has emerged in the last few years supporting the use of both sacubitril/valsartan and ivabradine in patients with chronic heart failure. Both agents were recently approved and included in the 2016 American College of Cardiology, American Heart Association, and Heart Failure Society of America (ACC/AHA/HFSA) Focused Update on New Pharmacological Therapy for Heart Failure.
Summary
Sacubitril/valsartan was found to significantly reduce cardiovascular and all-cause mortality with an acceptable safety profile in those with reduced ejection fraction. Ongoing trials are evaluating sacubitril/valsartan’s role in the management of patients with preserved ejection fraction, but phase II trials have provided promising results. Ivabradine was found to have a potential role in patients with heart rates ≥70 bpm, despite receiving maximized beta blocker therapy. This recent literature provides support for a shift towards a new era in the management of the heart failure patient.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mozzafarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. On behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e360.
Entresto [package insert]. Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
•• McMurray JJV, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004. The PARADIGM-HF trial was the first to evaluate the long-term risk of morbidity and mortality with the use of sacubitril/valsartan in comparison to enalapril in patients with heart failure with reduced ejection fraction. The authors found that the composite of death from cardiovascular causes, and a first hospitalization for heart failure was significantly reduced in those who received sacubitril/valsartan versus enalapril. Importantly, there was no significantly increased risk of serious angioedema with the use of sacubitril/valsartan
• Fox K, Ford I, Steg PG, Tendera M, Ferrari R, on behalf of the BEAUTIFUL investigators. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double blind, placebo-controlled trial. Lancet. 2008;372:807–16. The BEAUTIFUL trial assessed the addition of the novel agent, ivabradine, to standard heart failure therapies in those with reduced ejection fraction. There was no difference between those who received ivabradine and those who did not in regards to the composite of cardiovascular death or hospitalization for MI or new onset or worsening heart failure. However, authors suggested that there may be an effect with the use of ivabradine in a subset of patients with heart rates ≥ 70 bpm and coronary artery disease
• Swedberg K, Komajda M, Bohm M, Borer JS, Ford I, Dubost-Brama A, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875–85. The SHIFT trial was developed after the BEAUTIFUL trial to focus further on symptomatic heart failure patients with reduced ejection fraction who were on standard therapies and had heart rates ≥ 70 bpm. When compared to placebo, ivabradine was found to reduce the incidence of the composite of cardiovascular death or hospital admissions for worsening heart failure. The most common adverse event was symptomatic or asymptomatic bradycardia
2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62(16):e147–239.
McMurray JJV, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Dual angiotensin receptor and neprilysin inhibition as an alternative to angiotensin-converting enzyme inhibition in patients with chronic systolic heart failure: rationale for and design of the prospective comparison of ARNI with ACEI to determine impact on global mortality and morbidity in heart failure trial (PARADIGM-HF). Eur J Heart Fail. 2013;15(9):1062–73.
Vardeny O, Miller R, Solomon SD. Combined neprilysin and renin-angiotensin system inhibition for the treatment of heart failure. JACC Heart Fail. 2014;2:663–70.
Braunwald E. The path to an angiotensin receptor antagonist- neprilysin inhibitor in the treatment of heart failure. J Am Coll Cardiol. 2015;65:1029–41.
Kostis JB, Packer M, Black HR, Schmieder R, Henry D, Levy E. Omapatrilat and enalapril in patients with hypertension: the omapatrilat cardiovascular treatment vs. enalapril (OCTAVE) trial. Am J Hypertens. 2004;17(2):103–11.
Packer M, Califf RM, Konstam MA, Krum H, McMurray JJ, Rouleau JL, et al. Comparison of omapatrilat and enalapril in patients with chronic heart failure: the omapatrilat versus enalapril randomized trial of utility in reducing events (OVERTURE). Circulation. 2002;106:920–6.
Packer M, McMurray JJV, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation. 2015;131:54–61.
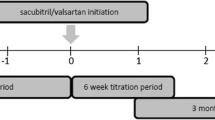
Senni M, McMurray JJV, Wachter R, McIntyre HF, Reyes A, Majercak I, et al. Initiating sacubitril/valsartan (LCZ696) in heart failure: results of TITRATION, a double-blind, randomised comparison of two up-titration regimens. Eur J Heart Fail. 2016; doi:10.1002/ejhf.548.
Lam CSP, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13(1):18–28.
Shah RV, Desai AS, Givertz MM. The effect of renin-angiotensin system inhibitors on mortality and heart failure hospitalization in patients with heart failure and preserved ejection fraction: a systematic review and meta-analysis. J Card Fail. 2010;16(3):260–7.
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012;380(9851):1387–95.
Masson S, Latini R, Anand IS, Barlera S, Angelici L, Vago T, et al. Prognostic value of changes in N-terminal pro-brain natriuretic peptide in val-HeFT (valsartan heart failure trial). J Am Coll Cardiol. 2008;52(12):997–1003.
Ivabradine [package insert]. Thousand Oaks, CA: Amgen; 2015.
Pocock SJ, Wang D, Pfeffer MA, Yusuf S, McMurray JJ, Swedberg KB, et al. Predictors of mortality and morbidity in patients with chronic heart failure. Eur Heart J. 2006;27:65–75.
Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R, on behalf of the BEAUTIFUL investigators. Heart rate as a prognostic risk factor in patients with coronary artery disease and leftventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet. 2008;372:817–21.
Gaziano TA, Fonarow GC, Claggett B, Chan WW, Deschaseaux-Voinet C, Turner SJ, et al. Cost-effectiveness analysis of sacubitril/valsartan vs enalapril in patients with heart failure and reduced ejection fraction. JAMA Cardiol Published online June. 2016;22
Kansal AR, Cowie MR, Kielhorn A, Krotneva S, Tafazzoli A, Zheng Y, et al. Cost‐effectiveness of ivabradine for heart failure in the United States. Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease. 2016;5(5):e003221.
King JB, Shah RU, Bress AP, Nelson RE, Bellows BK. Cost-effectiveness of sacubitril-valsartan combination therapy compared with enalapril for the treatment of heart failure with reduced ejection fraction. JACC Heart Fail. 2016;4(5):392–402.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectivenes —the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Rhoten, Malloy, and Stevens declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pharmacology of Acute Care
Rights and permissions
About this article
Cite this article
Rhoten, M.N., Malloy, R. & Stevens, C.A. A Change of Heart: the New Era of Heart Failure Management. Curr Emerg Hosp Med Rep 5, 21–27 (2017). https://doi.org/10.1007/s40138-017-0122-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-017-0122-9