Abstract
Purpose of review
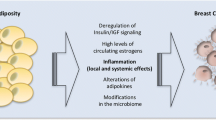
Obesity contributes to an estimated forty-percent, or 630,000 cases, of malignant neoplasms diagnosed in the United States, and higher body mass index (BMI) has been associated with at least seventeen types of solid tumors, including 9% of all breast cancer cases. In this review, we discuss the impact of obesity and consequences of obesity, including the metabolic syndrome and type 2 diabetes mellitus, on breast cancer risk and recurrence.
Recent findings
Recent work has identified multiple molecular mechanisms that may underlie the association between obesity and breast cancer. In particular, insulin resistance, increased inflammatory cytokines, leptin signaling, and adipokine signaling have been shown to affect breast cancer risk and outcomes. While obesity is associated with higher breast cancer incidences and worse breast cancer outcomes, several risk reduction methods have been shown to attenuate these risks. Both metformin and statins have been shown to improve disease-free survival and overall survival compared to non-users. Metformin also has been associated with lower risk of breast cancer incidence. Furthermore, increased physical activity and weight loss have been shown to decrease the risk of breast cancer, especially in post-menopausal women.
Summary
These studies have emphasized the potential impact that lifestyle changes can have on breast cancer risk and outcomes, and demonstrate the need for randomized control trials to evaluate the roles of metformin and statins for the treatment and chemoprevention of breast cancer.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
CDC. CDC Vital Signs [Internet]. 2017. Available from: https://www.cdc.gov/vitalsigns/.
Breast Cancer Risk Factors: Genetics.
Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet (London, England). Elsevier. 2014 [cited 2017 Nov 3];384:755–65. http://www.ncbi.nlm.nih.gov/pubmed/25129328.
Howell A, Anderson AS, Clarke RB, Duffy SW, Evans DG, Garcia-Closas M, et al. Risk determination and prevention of breast cancer. Breast Cancer Res. 2014;16(5):446.
Osaki Y, Taniguchi S, Tahara A, Okamoto M, Kishimoto T. Metabolic syndrome and incidence of liver and breast cancers in Japan. Cancer Epidemiol. 2012;36:141–7.
Bhandari R, Kelley GA, Hartley TA, Rockett IRH. Metabolic syndrome is associated with increased breast cancer risk: a systematic review with meta-analysis. Int J Breast Cancer. 2014;2014:1–13.
Health United States Report 2016. 2016.
Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington DC, 2007.
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult Weight change and risk of postmenopausal breast cancer. JAMA. 2006;296:193–201.
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005–2014. JAMA. 2016 [cited 2017 Dec 2];315:2284. http://www.ncbi.nlm.nih.gov/pubmed/27272580.
National Diabetes Statistics Report, 2017 estimates of diabetes and Its burden in the United States Background. 2017.
Harlan DM, Giovannucci E, Archer MC, Bergenstal RM, Gapstur SM, Habel LA. Diabetes and cancer: a consensus report. CA. 2010;60:207–21.
Larsson SC, Mantzoros CS, Wolk A. Diabetes mellitus and risk of breast cancer: a meta-analysis. Int J Cancer. 2007;121:856–62.
Boyle P, Boniol M, Koechlin A, Robertson C, Valentini F, Coppens K, et al. Diabetes and breast cancer risk: a meta-analysis. Br J Cancer. 2012;107:1608–17.
Michels KB, Solomon CG, Hu FB, Rosner BA, Hankinson SE, Colditz GA, et al. Type 2 diabetes and subsequent incidence of breast cancer in the Nurses’ Health Study. Diabetes Care. 2003;26:1752–8.
Mauro L, Naimo GD, Ricchio E, Panno ML, Andò S. Cross-talk between adiponectin and IGF-IR in breast cancer. Front Oncol. 2015;5:157.
• Huang J, Li L, Lian J, Schauer S, Vesely PW, Kratky D, et al. Tumor-induced hyperlipidemia contributes to tumor growth. Cell Rep. 2016 [cited 2017 Dec 3];15:336–48. http://www.ncbi.nlm.nih.gov/pubmed/27050512.
Sun K, Kusminski CM, Scherer PE. Adipose tissue remodeling and obesity. J Clin Invest. 2011 [cited 2017 Dec 3];121:2094–101. http://www.ncbi.nlm.nih.gov/pubmed/21633177.
Parsons DW, Jones S, Zhang X, Lin JC-H, Leary RJ, Angenendt P, et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008 [cited 2017 Dec 18];321:1807–12. http://www.ncbi.nlm.nih.gov/pubmed/18772396.
Chan LN, Chen Z, Braas D, Lee J-W, Xiao G, Geng H, et al. Metabolic gatekeeper function of B-lymphoid transcription factors. Nature. 2017 [cited 2017 Dec 18];542:479–83. http://www.nature.com/doifinder/10.1038/nature21076.
Vander Heiden MG. Targeting cancer metabolism: a therapeutic window opens. Nat. Rev. Drug Discov. 2011 [cited 2017 Dec 18];10:671–84. http://www.ncbi.nlm.nih.gov/pubmed/21878982.
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE, et al. Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Ins. 2009;101:48–60.
Khandekar MJ, Cohen P, Spiegelman BM. Molecular mechanisms of cancer development in obesity. Nat Rev Cancer. 2011 [cited 2017 Nov 25];11:886–95. http://www.nature.com/doifinder/10.1038/nrc3174.
• Freese KE, Kokai L, Edwards RP, Philips BJ, Sheikh MA, Kelley J, et al. Adipose-derived stems cells and their role in human cancer development, growth, progression, and metastasis: a systematic review. Cancer Res. 2015 [cited 2017 Dec 18];75:1161–8. http://www.ncbi.nlm.nih.gov/pubmed/25736688.
VanSaun MN. Molecular pathways: adiponectin and leptin signaling in cancer. Clin Cancer Res. 2013 [cited 2017 Dec 18];19:1926–32. http://www.ncbi.nlm.nih.gov/pubmed/23355630.
Saxena NK, Sharma D. Leptin-signaling pathways as therapeutic targets in cancer. Springer, Cham. 2017 [cited 2017 Nov 3]. p. 67–87. http://link.springer.com/10.1007/978-3-319-41677-9_4.
Erkasap N, Ozkurt M, Erkasap S, Yasar F, Uzuner K, Ihtiyar E, et al. Leptin receptor (Ob-R) mRNA expression and serum leptin concentration in patients with colorectal and metastatic colorectal cancer. Braz J Med Biol Res. 2013 [cited 2017 Nov 3];46:306–10. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-879X2013000300306&lng=en&tlng=en.
Teraoka N, Mutoh M, Takasu S, Ueno T, Nakano K, Takahashi M, et al. High susceptibility to azoxymethane-induced colorectal carcinogenesis in obese KK-Ay mice. Int J Cancer. 2011 [cited 2017 Nov 30];129:528–35. http://doi.wiley.com/10.1002/ijc.25711.
Arita S, Kinoshita Y, Ushida K, Enomoto A, Inagaki-Ohara K. High-fat diet feeding promotes stemness and precancerous changes in murine gastric mucosa mediated by leptin receptor signaling pathway. Arch Biochem Biophys. 2016 [cited 2017 Nov 30];610:16–24. http://www.ncbi.nlm.nih.gov/pubmed/27693038.
Tamakoshi K, Toyoshima H, Wakai K, Kojima M, Suzuki K, Watanabe Y, et al. Leptin Is Associated with an increased female colorectal cancer risk: a nested case-control study in Japan. Oncology. 2005 [cited 2017 Nov 30];68:454–61. http://www.ncbi.nlm.nih.gov/pubmed/16020976.
Park J, Kusminski CM, Chua SC, Scherer PE. Leptin receptor signaling supports cancer cell metabolism through suppression of mitochondrial respiration in Vivo. Am J Pathol. 2010 [cited 2017 Dec 1];177:3133–44. http://www.ncbi.nlm.nih.gov/pubmed/21056997.
Amemori S, Ootani A, Aoki S, Fujise T, Shimoda R, Kakimoto T, et al. Adipocytes and preadipocytes promote the proliferation of colon cancer cells in vitro. AJP Gastrointest Liver Physiol. 2006 [cited 2017 Dec 1];292:G923–9. http://www.ncbi.nlm.nih.gov/pubmed/17170030.
Deng T, Lyon CJ, Bergin S, Caligiuri MA, Hsueh WA. Obesity, inflammation, and cancer. Annu Rev Pathol Mech Dis. 2016 [cited 2017 Nov 3];11:421–49. http://www.annualreviews.org/doi/10.1146/annurev-pathol-012615-044359.
Goldacre MJ, Wotton CJ, Yeates D, Seagroatt V, Jewell D. Cancer in patients with ulcerative colitis, Crohnʼs disease and coeliac disease: record linkage study. Eur J Gastroenterol Hepatol. 2008 [cited 2017 Dec 3];20:297–304. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00042737-200804000-00009.
Frisch M, Biggar RJ, Engels EA, Goedert JJ, Group for the A-CMRS. Association of cancer with AIDS-related immunosuppression in adults. JAMA. American Medical Association. 2001 [cited 2017 Dec 3];285:1736. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.285.13.1736.
Durán HA, de Rey BM. Differential oxidative stress induced by two different types of skin tumor promoters, benzoyl peroxide and 12-O-tetradecanoylphorbol-13-acetate. Carcinogenesis. 1991 [cited 2017 Nov 3];12:2047–52. http://www.ncbi.nlm.nih.gov/pubmed/1934290.
McCreery MQ, Halliwill KD, Chin D, Delrosario R, Hirst G, Vuong P, et al. Evolution of metastasis revealed by mutational landscapes of chemically induced skin cancers. Nat Med. 2015 [cited 2017 Nov 3];21:1514–20. http://www.ncbi.nlm.nih.gov/pubmed/26523969.
Rehman I, Lowry DT, Adams C, Abdel-Fattah R, Holly A, Yuspa SH, et al. Frequent codon 12 Ki-ras mutations in mouse skin tumors initiated by N-methyl-N?-nitro-N-nitrosoguanidine and promoted by mezerein. Mol Carcinog. 2000 [cited 2017 Dec 1];27:298–307. http://doi.wiley.com/10.1002/%28SICI%291098-2744%28200004%2927%3A4%3C298%3A%3AAID-MC8%3E3.0.CO%3B2-4.
Dong Y, Sun Q, Zhang X. PD-1 and its ligands are important immune checkpoints in cancer. Oncotarget. 2017 [cited 2017 Nov 3];8:2171–86. http://www.ncbi.nlm.nih.gov/pubmed/27974689.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009 [cited 2017 Nov 3];360:765–73. http://www.ncbi.nlm.nih.gov/pubmed/19228619.
McTiernan A, Rajan KB, Tworoger SS, Irwin M, Bernstein L, Baumgartner R, et al. Adiposity and sex hormones in postmenopausal breast cancer survivors. J Clin Oncol. 2003;21:1961–6.
Key TJ, Appleby PN, Reeves GK, Roddam A, Dorgan JF, Longcope C, et al. Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J Natl Cancer Inst. 2003;95:1218–26.
Fuhrman BJ, Schairer C, Gail MH, Boyd-Morin J, Xu X, Sue LY, et al. Estrogen metabolism and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 2012;104:326–39.
Gershuni V, Li YR, Williams AD, So A, Steel L, Carrigan E, et al. Breast cancer subtype distribution is different in normal weight, overweight, and obese women. Breast Cancer Res Treat. 2017 [cited 2017 Mar 21];163. http://link.springer.com/10.1007/s10549-017-4192-x.
•• Ligibel JA, Cirrincione CT, Liu M, Citron M, Ingle JN, Gradishar W, et al. Body Mass Index, PAM50 subtype, and outcomes in node-positive breast cancer: CALGB 9741 (Alliance). J Natl Cancer Inst. Oxford University Press. 2015;107.
Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293:2479–86.
Irwin ML, Smith AW, McTiernan A, Ballard-Barbash R, Cronin K, Gilliland FD, et al. Influence of pre- and postdiagnosis physical activity on mortality in breast cancer survivors: the health, eating, activity, and lifestyle study. J Clin Oncol. 2008;26:3958–64.
Schmid D, Leitzmann MF. Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol. 2014;25:1293–311.
•• Sonnenblick A, Agbor-Tarh D, Bradbury I, Di Cosimo S, Azim HA, Fumagalli D, et al. Impact of diabetes, insulin, and metformin use on the outcome of patients with human epidermal growth factor receptor 2-positive primary breast cancer: analysis from the ALTTO Phase III Randomized Trial. J Clin Oncol, American Society of Clinical Oncology. 2017;35:1421–9.
Kaplan MA, Pekkolay Z, Kucukoner M, İnal A, Urakci Z, Ertugrul H, et al. Type 2 diabetes mellitus and prognosis in early stage breast cancer women. Med Oncol. 2012;29:1576–80.
Li CI, Daling JR, Tang MTC, Malone KE. Relationship between diabetes and risk of second primary contralateral breast cancer. Breast Cancer Res Treat. 2011;125:545–51.
Srokowski TP, Fang S, Hortobagyi GN, Giordano SH. Impact of diabetes mellitus on complications and outcomes of adjuvant chemotherapy in older patients with breast cancer. J Clin Oncol. 2009;27:2170–6.
Zhang Z-J, Li S. The prognostic value of metformin for cancer patients with concurrent diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2014;16:707–10.
Jiralerspong S, Palla SL, Giordano SH, Meric-Bernstam F, Liedtke C, Barnett CM, et al. Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol. 2009;27:3297–302.
Hadad S, Iwamoto T, Jordan L, Purdie C, Bray S, Baker L, et al. Evidence for biological effects of metformin in operable breast cancer: a pre-operative, window-of-opportunity, randomized trial. Breast Cancer Res Treat. 2011;128:783–94.
Ahern TP, Lash TL, Damkier P, Christiansen PM, Cronin-Fenton DP. Statins and breast cancer prognosis: evidence and opportunities. Lancet Oncol. 2014;15:461–8. https://doi.org/10.1016/S1470-2045(14)70119-6.
Murtola TJ, Visvanathan K, Artama M, Vainio H, Pukkala E. Statin use and breast cancer survival: a nationwide cohort study from Finland. PLoS ONE. 2014;9:e110231. https://doi.org/10.1371/journal.pone.0110231.
Ahern TP, Pedersen L, Tarp M, Cronin-Fenton DP, Garne JP, Silliman RA, et al. Statin prescriptions and breast cancer recurrence risk: a Danish nationwide prospective cohort study. J Natl Cancer Inst. 2011;103:1461–8. https://doi.org/10.1093/jnci/djr291.
•• Borgquist S, Giobbie-Hurder A, Ahern TP, Garber JE, Colleoni M, Láng I, et al. Cholesterol, cholesterol-lowering medication use, and breast cancer outcome in the BIG 1-98 Study. J Clin Oncol. 2017;35:1179–88.
Wang A, Aragaki AK, Tang JY, Kurian AW, Manson JE, Chlebowski RT, et al. Statin use and all-cancer survival: prospective results from the women’s health initiative. Br J Cancer. 2016;115:129–35.
Keyomarsi K, Sandoval L, Band V, Pardee AB. Synchronization of tumor and normal cells from G1 to multiple cell cycles by lovastatin. Cancer Res. 1991;51:3602–9.
Agarwal B, Bhendwal S, Halmos B, Moss SF, Ramey WG, Holt PR. Lovastatin augments apoptosis induced by chemotherapeutic agents in colon cancer cells. Clin Cancer Res. 1999;5:2223–9.
Padayatty SJ, Marcelli M, Shao TC, Cunningham GR. Lovastatin-induced apoptosis in prostate stromal cells. J Clin Endocrinol Metab. 1997;82:1434–9.
Kusama T, Mukai M, Iwasaki T, Tatsuta M, Matsumoto Y, Akedo H, et al. Inhibition of epidermal growth factor-induced RhoA translocation and invasion of human pancreatic cancer cells by 3-hydroxy-3-methylglutaryl-coenzyme a reductase inhibitors. Cancer Res. 2001;61:4885–91.
Seeger H, Wallwiener D, Mueck A. Statins can inhibit proliferation of human breast cancer cells in Vitro. Exp Clin Endocrinol. 2003;111:47–8.
Matthews SB, Thompson HJ. The obesity-breast cancer conundrum: an analysis of the issues. Int J Mol Sci. 2016;17.
• Hardefeldt PJ, Penninkilampi R, Edirimanne S, Eslick GD. Physical activity and weight loss reduce the risk of breast cancer: a meta-ANALYSIS of 139 prospective and retrospective studies. Clin. Breast Cancer. 2017
•• Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ. British Medical Journal Publishing Group. 2016;354:i3857.
Bardia A, Hartmann LC, Vachon CM, Vierkant RA, Wang AH, Olson JE, et al. Recreational physical activity and risk of postmenopausal breast cancer based on hormone receptor status. Arch Intern Med, American Medical Association. 2006;166:2478.
• Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? a harmonised meta-analysis of data from more than 1 million men and women. Lancet. Elsevier. 2016;388:1302–10.
• Moore SC, Lee I-M, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176:816.
McTiernan A, Tworoger SS, Ulrich CM, Yasui Y, Irwin ML, Rajan KB, et al. Effect of exercise on serum estrogens in postmenopausal women: a 12-month randomized clinical trial. Cancer Res. 2004;64:2923–8.
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, et al. Tamoxifen for the prevention of breast cancer: current status of the national surgical adjuvant breast and Bowel Project P-1 Study. JNCI J Natl Cancer Inst. 2005;97:1652–62.
Bodmer M, Meier C, Krahenbuhl S, Jick SS, Meier CR. Long-term metformin use is associated with decreased risk of breast cancer. Diabetes Care. 2010;33:1304–8.
Currie CJ, Poole CD, Gale EAM. The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia. 2009;52:1766–77.
Quinn BJ, Kitagawa H, Memmott RM, Gills JJ, Dennis PA. Repositioning metformin for cancer prevention and treatment. Trends Endocrinol Metab. 2013;24:469–80.
Chae YK, Arya A, Malecek M-K, Shin DS, Carneiro B, Chandra S, et al. Repurposing metformin for cancer treatment: current clinical studies. Oncotarget. 2016;7:40767–80.
Martinez JA, Chalasani P, Thomson CA, Roe D, Altbach M, Galons J-P, et al. Phase II study of metformin for reduction of obesity-associated breast cancer risk: a randomized controlled trial protocol. BMC Cancer. 2016;16:500.
Undela K, Srikanth V, Bansal D. Statin use and risk of breast cancer: a meta-analysis of observational studies. Breast Cancer Res Treat. 2012;135:261–9.
Bonovas S, Filioussi K, Tsavaris N, Sitaras NM. Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol. 2005;23:8606–12.
Kuoppala J, Lamminpää A, Pukkala E. Statins and cancer: a systematic review and meta-analysis. Eur J Cancer. 2008;44:2122–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Breast Cancer Surgery.
Rights and permissions
About this article
Cite this article
Li, Y.R., Ro, V. & Tchou, J.C. Obesity, Metabolic Syndrome, and Breast Cancer: From Prevention to Intervention. Curr Surg Rep 6, 7 (2018). https://doi.org/10.1007/s40137-018-0204-y
Published:
DOI: https://doi.org/10.1007/s40137-018-0204-y