Abstract
Purpose of Review
The purpose of this review was to summarize the current knowledge on parosmia and phantosmia and introduce support and treatment algorithms for the two qualitative olfactory disorders.
Recent Findings
Recent literature regarding parosmia has revealed that patients with the disorder are mainly triggered by certain substances, including thiols and pyrazines. In 2015, the existing “olfactory training” regimen was improved to more effectively treat post-infectious olfactory loss and was named “modified olfactory training” (MOT). It was also found in 2022 that MOT is also effective against COVID-19-induced parosmia.
Summary
Parosmia, the distortion of smells, is a symptom in qualitative olfactory disorders that severely affects patients’ mental well-being and enjoyment of their everyday lives. The condition was first documented in 1895 and can affect up to 5% of the general population. Etiologies of parosmia include sinonasal diseases, viruses, surgeries, traumatic brain injury, neurological and psychiatric conditions, toxic chemicals, and medications. Parosmia has seen a surge in cases since the onset of the COVID-19 pandemic and is linked to changes in brain structure following an infection. The evaluation of the symptom is done using surveys, smell identification tests, fMRI, MRI, PET/CT, and gas chromatography. Treatment for parosmia can vary in duration, which makes it essential to focus not only on helping the patients regain normosmia, but also on supporting the patient through the recovery journey. Parosmia should not be confused with phantosmia, in which the distortion of smells occurs in the absence of olfactory stimuli. The etiology of phantosmia can vary from infections and traumatic brain injury to psychiatric disorders like schizophrenia. Unlike parosmia, the treatment of phantosmia is less straightforward, with an emphasis on determining the etiology and providing symptomatic relief.
Similar content being viewed by others
Introduction: Defining Parosmia
Parosmia, while initially confused by researchers with other symptoms of qualitative smell disorders, thankfully has a well-established definition now. Today, scientists define parosmia as the distortion of smell detection in the presence of smell stimuli, unlike phantosmia, where distorted smell detection occurs without any smell stimuli to trigger it. Cases of loss of smell can be classified into two main categories: quantitative and qualitative smell disorders [1]. Cases of quantitative smell disorders mainly present as hyposmia and anosmia and can be diagnosed and managed more easily. Meanwhile, qualitative smell disorders that present mainly as parosmia and phantosmia are areas of research that are more open to interpretation and management by novel methods [2]. Parosmia also has two subtypes of symptoms with cacosmia being the detection of unpleasant smells and euosmia being the detection of pleasant ones [2, 3].
Prevalence
While previous literature calculated the prevalence of smell disorders to be 19.1% of the general population, the same researchers found that the prevalence of parosmia cases was 4–5% [4,5,6,7]. However, the prevalence among older adults may be as high as 62.5% [5, 8]. Regarding the prevalence of these disorders in cases of COVID-19 infections, these statistics were calculated to be up to 75% for smell disorders and up to 45% for parosmia [9, 10]. Among people with smell disorders, up to 35% were found to have symptoms of parosmia [11].
History of Parosmia
Contrary to popular belief, research efforts on parosmia have continued for over a century, with the first paper published on the topic being an 1895 case study investigating three patients with parosmia. The three patients described parosmic smells as “ammonia-like” and “foul.” Recognized as the paper that coined the term parosmia, Tilley’s report paved the way for future otorhinolaryngologists to investigate this qualitative smell disorder. In the report, the author even experimented with different methods to treat the condition, including intranasal stimulants [12].
Following this study, a 1966 article summarizing a series of twentieth-century papers by the Danish researcher Kaj Zilstorff acted as a position paper for parosmia, describing the understanding of its etiology at the time, as well as treatment methods that had been attempted. In his paper, Zilstorff recommends the intranasal administration of 10% cocaine hydrochloride, stating that it effectively cured almost all subjects with parosmia [13]. This finding was replicated by Leopold et al. in 1991, and was deemed an ineffective method for the long-term management of olfactory dysfunction [14, 15].
Etiology of Parosmia
When the etiology of parosmia is investigated, upper respiratory tract infections, traumatic brain injury, sinonasal diseases, neurological and psychiatric disorders, exposure to toxic chemicals, chemotherapy, and surgery come up as the most common causes of the disorder [16,17,18, 19•, 20,21,22, 23••, 24, 25]. Since it has many potential etiologies, it is important to be careful when ruling out all possible etiologies before a decision is made.
Parosmia and COVID-19
For many years following the initial definition of parosmia in 1895, researchers had shifted their focus toward quantitative smell disorders like anosmia, the term for total olfactory loss, putting qualitative smell dysfunctions like parosmia and phantosmia into the background. Following the onset of the COVID-19 pandemic and the ever-increasing number of cases of post-infectious olfactory dysfunction, the addition of the post-COVID manifestation of parosmia helped cause an accumulation of knowledge and new approaches. Although parosmia was already a condition with years of research but limited clinical interventions, the surge in olfactory dysfunction cases following the COVID-19 pandemic made it a well-known condition. The COVID-19 pandemic has caused breakthroughs in understanding smell disorders, including parosmia.
It has been documented that COVID-19 infections account for many changes in the nose and brain that may be responsible for the smell disorders caused by the disease. Recent studies investigating patients after a COVID-19 infection have detected changes in the brain structure and bilateral atrophy of the olfactory bulb which may account for the long-lasting disordered smell symptoms following the infection [26••, 27]. Interestingly, research conducted in Iraq argued that traditional treatment methods like olfactory training and steroids were rarely effective when treating post-COVID parosmia [28]. To solve this problem, a derived olfactory training method by the name “modified olfactory training” was proposed, demonstrating a statistically significant level of effectiveness in the recovery of post-COVID parosmia patients [29,30,31]. While worrying at first, the increased prevalence of parosmia cases with the COVID-19 pandemic gave way to many discoveries in the field of smell disorders, opening treatment opportunities for the wider body of olfactory disorder patients.
Molecular and Physiological Mechanisms Behind Parosmia
After defining and determining the etiology of parosmia, in addition to the clinical studies classifying parosmia as a result of healing from cases of hyposmia and anosmia, there is also an increase in the number of studies arguing that parosmia is a result of changes in the cortical regions of the brain [32,33,34]. Other studies argue that the distortion of olfactory signals is caused by the ephaptic firing of healing neurons that are not yet remyelinated or by the incorrect wiring of glomeruli [2, 35]. While some patients show improvement in the first 1–2 months of the onset of symptoms, the literature regarding parosmia also documents patients that have improved even after 40 years of symptoms [36]. The vastly varying durations in which parosmia patients have had symptoms account for why the qualitative smell disorders require multiple approaches and explanations for classification. This significant variation can also be interpreted as a sign for clinicians to avoid telling patients that “if symptoms do not improve in the first six months, there is little hope that it will improve later,” a piece of advice many patients hear from primary and secondary care providers. Not only is this advice incorrect, but it can also cause the patient to lose hope in the suggested treatment.
Now that parosmia is shown to be triggered by the presence of certain olfactory stimuli, researchers have shifted their focus toward determining which smells and circumstances trigger the symptoms. A study published by Bonfils et al. in 2005, many years before the COVID-19 pandemic, shows that the smells that trigger parosmia the most were the smells of gasoline, tobacco, perfumes, citrus, and chocolate [37]. The chemical basis of parosmia, however, is a post-COVID era phenomenon. Scientists that have worked in this field for years have taken advantage of their previous experiences and observed the post-COVID parosmia process in many people, finally changing the term “parosmia-triggering smells” to “parosmia-triggering chemicals” [38, 39].
At first, 2-furanmethanethiol, the chemical that gives coffee its intense smell, was identified as a parosmia-triggering chemical. Later, it was revealed through gas chromatography that the triggering factors of the disorder were much more than just one smell molecule [38, 39]. Primarily 2-furanmethanethiol, 2-ethyl-3,6-dimethylpyrazine, 3-methyl-2-butene-1-thiol, and 3-mercapto-3-methylbutyl formate were found to be the main factors triggering parosmia [38, 39]. The question as to why the response to these molecules is altered with the onset of parosmia can have many answers, and the question of whether this increase in the sensitivity of the olfactory system to bad smells, when it is typically evolutionarily adapted to prioritize hazardous smells over others, can be explained with the over-firing of receptors resulting from the overhealing of neurons or the damage to the olfactory bulb following alterations to cognitive functions remains unclear [2, 33, 34]. Furthermore, previous studies have shown that long-term and slow-healing anosmia caused by COVID-19 generally impacted patients’ olfactory bulbs, either through direct damage or through reactivity of the olfactory bulbs upstream from the site of the damage [27]. Olfactory bulb damage being present in some patients with post-COVID anosmia and not in others suggests that this might indicate whether the patient will develop parosmia. Similarly, the correlation between olfactory 4 width and the prevalence of smell disorders in post-viral and post-COVID patients may signal that smell disorders may be caused by receptor damage [40,41,42]. Most recently, studies have shown that certain loci in the human genome may affect the likelihood that one may develop post-COVID olfactory dysfunction [43].
Overall, it can be seen in the previous academic literature that anomalies and variations of many factors can lead to olfactory disorders, including anatomical, genetic, receptor-related, and cortical factors, and that this symptom cannot boil down to a single cause [2, 27, 30, 34, 42,43,44].
Evaluating Parosmia
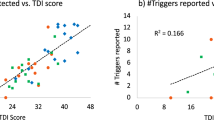
During the COVID-19 pandemic, centers for smell and taste disorders have also started focusing on novel testing methods and smell tests when evaluating anosmia and parosmia. While not all are used in current clinical practices, methods such as surveys, evaluation forms, neurocognitive tests, parosmia-specific odor identification tests, fMRI, MRI, PET/CT, and gas chromatography have all helped smell and taste specialists investigate the chemical basis of smell even more in-depth [38, 45,46,47,48,49,50,51]. The previously mentioned parosmia-specific surveys and tests make it easier for clinicians to keep track of patient progress, and for patients to stay on top of their treatment process. Parosmia-specific smell identification tests like SSParoT make it easier to interpret the change in the patient’s smell perception and relationship with food [48]. In SSParoT, pleasant and unpleasant smells are paired to provide hedonic range and direction values that turn subjective descriptions of parosmia into objective scores [48].
Changes in Quality of Life
As a symptom distorting patients’ olfactory perception, it is not too surprising to read in the academic literature that parosmia changes the quality of life for the worse [52]. Current literature investigating parosmia patients’ quality of life focuses mainly on the patients’ relationships with cooking and eating. Since the sense of smell is known to be a survival mechanism to determine whether a food is edible, the unpleasant distortion of this sense causes patients to view more foods as inedible or harmful [53]. The initial studies investigating the effects of smell disorders on nutrition found that 72% of patients reported a decline in their enjoyment of food [22, 54]. A recent publication also discovered that patients with parosmia experienced greater weight loss than those with other types of olfactory loss. The same study also investigated the effects of smell disorders in cooking and found that people with smell deficits said they “wanted to get through cooking ASAP” more often than people with an intact sense of smell [55]. Patients testifying how their disorder affected them emphasized the psychological effects of losing a sense, with one patient saying they are “grieving for [their] lost senses” [56]. Another study investigating this issue in the UK found that 52.4% of people with olfactory disorders had either depression and/or anxiety, while 62% of the population said that olfactory disorders had an impact on their enjoyment of their everyday lives [36, 57]. In all studies, parosmia patients reported negative impacts on psychological health, well-being, and nutrition [36, 39, 54,55,56,57,58].
Management and Treatment of Parosmia
Inspired by the long recovery periods of parosmic patients with olfactory training, a derived training method called “modified olfactory training” was proposed, where the traditional procedure is upgraded with the addition of new smells and the extension of the training period [29–31]. Compared to the classical method of olfactory training, this novel method resulted in an overall higher level of recovery, making it the new gold standard for the treatment of olfactory disorders [29]. Even with this method, some patients could take up to 6 months to recover, highlighting the importance of extended treatment duration [29, 30].
When the previously mentioned courses of treatment like corticosteroids and olfactory training fail to yield positive results, surgical techniques like “olfactory cleft blocking” may be used as a last resort. In this novel procedure, openings of the olfactory cleft are surgically closed off, completely preventing potentially triggering odorants from reaching the olfactory epithelium [59]. This technique, however, is reserved for managing the condition since it only provides symptomatic relief from parosmia without restoring normosmia.
As parosmia can seriously affect patients’ quality of life, the management strategies of parosmia must also focus on effectively communicating with the patient and making them feel understood. Therefore, establishing uninterrupted communication between the physician, the patient, and the patient’s relatives is of utmost importance when managing parosmia. This is because parosmia patients’ relatives cannot always detect when the patient is going through emotional distress due to their condition, making the situation even worse for the patients. It is also why it is important to evaluate parosmic patients along with a friend or relative. When a patient is asked to smell a pleasant coffee smell and says that it “smells like tar,” the contrasting reaction from their relative enjoying the smell forms the first step in building empathy between the two.
To support both the recovery and the well-being of the patients, the following course of treatment was developed and implemented by me:
-
1.
The patient is asked to fill out a form informing the clinician of their personal situation and the chemicals disturbing them. They are also asked to create a “blacklist” with parosmia-triggering smells and tastes.
-
2.
If the patient does not live alone, a close friend or relative is asked to accompany them to the smell test. They are then asked to smell the same stimuli, and the contrasting reactions help create an “empathy bridge.”
-
3.
The results of the smell evaluations are saved for use during the diagnosis, treatment, and follow-up processes. It is important that the clinician is familiar with the categories of the smell molecules and looks at the test smells as more than just smells but also chemical substances (“chemoparosmic process”).
-
4.
If the patient is found to have vitamin and mineral deficits, rapid weight loss, and malnutrition, vitamin and mineral supplements should be prescribed in addition to the treatment.
-
5.
Additional treatments should be prescribed to patients exhibiting decreased cognitive functions.
-
6.
The modified olfactory training procedure should be explained to the patient in detail with the durations, frequency, and order of training with the different smells.
-
7.
The patients are advised to make the following changes in their lifestyles:
-
(a)
Exercising outdoors: Since sweat may trigger parosmia, working indoors may be difficult for patients. Exercising outdoors will minimize detecting parosmia-triggering body odors and help the patient stay active.
-
(b)
To improve mood: Increased sunlight exposure is recommended to elevate mood [60].
-
(c)
To improve general quality of life: Patients are recommended to maintain a healthy sleep schedule, listen to music every day, and meditate.
Figure 1 illustrates the ideal methods to support the parosmic patient throughout the treatment.
The support algorithm above is utilized in my clinic to support the patient throughout the entire process, both mentally and physically. Not only does the course of treatment help with the symptoms of parosmia, but the other aspects of the process also help correct the neurotransmitter imbalances in the brain
Phantosmia
Phantosmia, another potential symptom of qualitative smell disorders, involves distorted smell detection in the absence of an olfactory stimulus [1]. The first documented case of phantosmia was reported in a 1988 paper where a patient experiencing olfactory hallucinations was cured through resection of the left olfactory nerve, which was hypothesized to be the origin of the hallucinations [61]. While phantosmia can result from other olfactory dysfunctions, the etiology is not clearly known for idiopathic phantosmia cases, and phantosmia and olfactory hallucinations are common symptoms in patients with schizophrenia and other neurological/psychiatric conditions [16, 62,63,64,65,66]. Such hallucinations have also been linked to traumatic brain injury, radiation therapy, viral infections, surgeries on the nose, and rhinosinusitis [67,68,69,70,71]. Interestingly, a 2013 case study documented a patient with Parkinson’s disease–related phantosmia that reported increased olfactory hallucinations before weather events like storms, leading him to believe that he could forecast the weather [62]. As the symptom cannot be linked to reactions to certain olfactory triggers, methods of evaluation are more limited compared to other smell disorders. These diagnostic methods include survey questions, scales, fMRI, and magnetic resonance spectroscopy [1, 47, 72, 73]. Most recently, the COVID-19 pandemic has caused a surge in the number of patients with phantosmia, most of whom have developed phantosmia symptoms upon recovering from post-COVID anosmia [44, 71, 74]. A 2022 case study on the course of symptoms of post-COVID phantosmia patients has found great variety in the number of days post-COVID that the patients started having phantosmia symptoms, with patients beginning to see symptoms from as little as 10 days and as long as 300 days after the infection [44].
Current management methods for the disorder are mainly medical [15, 75,76,77]. While it was initially proposed by Zilstorff’s 1966 paper to treat qualitative smell disorders with intranasal cocaine hydrochloride, the treatment method is not used at this time, and recent literature has shown that it is not an effective long-term treatment for phantosmia [13, 14]. Other case studies also demonstrated that medications like antipsychotics, anticonvulsants, and antidepressants could relieve the symptoms of patients with idiopathic phantosmia, suggesting that the disorder may be caused by alterations in cortical structures and activity levels in the brain [65, 76, 78, 79]. Since distorted olfaction in phantosmia does not result from any specific stimuli, the disorder is a field of research that is developing slower than other fields of olfactory research, meaning that future work is still needed to help create an effective method for treating it. Figure 2 is a flowchart summarizing the current diagnosis and treatment processes for patients presenting with olfactory hallucinations.
Conclusion
Parosmia and phantosmia are qualitative olfactory disorders that greatly affect patients’ quality of life. While parosmia causes unpleasant odors in response to triggering odorants like thiols and pyrazines, phantosmia can cause these odors even in the absence of odorant triggers. Although novel treatment methods have caused significant improvements in the treatment of these disorders, especially parosmia, the success rate still is not satisfactory. Future research should prioritize developing more reliable treatment regimens and focus on improving patients’ quality of life.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, Costanzo RM, et al. Position paper on olfactory dysfunction. Rhinology. 2017;54:1–30.
Hawkes C. Parosmia: Treatment, mechanism, and types. BMJ. 2020:m4739.
Landis BN, Frasnelli J, Hummel T. Euosmia: a rare form of parosmia. Acta Otolaryngol. 2006;126:101–3.
Brämerson A, Johansson L, Ek L, Nordin S, Bende M. Prevalence of olfactory dysfunction: the Skövde population-based study. Laryngoscope. 2004;114:733–7.
Murphy C. Prevalence of olfactory impairment in older adults. JAMA. 2002;288:2307.
Nordin S, Brämerson A, Bende M. Prevalence of parosmia: the Skövde population-based studies. Millqvist E, editor. Rhinology. 2007;45.
Olofsson J, Ekesten F, Nordin S. Smell distortions: prevalence, longevity and impact of Parosmia in a population-based, longitudinal study spanning 10 years. PsyArXiv. 2021. https://doi.org/10.31234/osf.io/nx8z9.
Sjölund S, Larsson M, Olofsson JK, Seubert J, Laukka EJ. Phantom smells: prevalence and correlates in a population-based sample of older adults. Chem Senses. 2017;42:309–18.
Ohla K, Veldhuizen MG, Green T, Hannum ME, Bakke AJ, Moein ST, et al. A follow-up on quantitative and qualitative olfactory dysfunction and other symptoms in patients recovering from COVID-19 smell loss. Rhinol J. 2022 Apr 10. https://doi.org/10.4193/Rhin21.415.
Lechien JR, Vaira LA, Saussez S. Prevalence and 24-month recovery of olfactory dysfunction in COVID‐19 patients: a multicenter prospective study. J Intern Med. 2022 Sep. https://doi.org/10.1111/joim.13564.
Pellegrino R, Mainland JD, Kelly CE, Parker JK, Hummel T. Prevalence and correlates of parosmia and phantosmia among smell disorders. Chem Senses. 2021;46.
Tilley H. Three cases of parosmia; causes, treatment, & c. The Lancet. 1895;146:907–8.
Parosmia ZK. J Laryngol Otol. 1966;80:1102–4.
Leopold DA, Hornung DE. Olfactory cocainization is not an effective long-term treatment for phantosmia. Chem Senses. 2013;38:803–6.
Leopold DA, Schwob JE, Youngentob SL, Hornung DE, Wright HN, Mozell MM. Successful treatment of phantosmia with preservation of olfaction. Arch Otolaryngol Head Neck Surg. 1991;117:1402–6.
Croy I, Yarina S, Hummel T. Research letter Enhanced parosmia and phantosmia in patients with severe depression. Psychol Med. 2013;43:2460–4.
Damm M, Temmel A, Welge-Lüssen A, Eckel HE, Kreft M-P, Klussmann JP, et al. Riechstörungen. HNO. 2004;52:112–20.
Reden J, Maroldt H, Fritz A, Zahnert T, Hummel T. A study on the prognostic significance of qualitative olfactory dysfunction. Eur Arch Otorhinolaryngol. 2006;264:139–44.
• Ciurleo R, De Salvo S, Bonanno L, Marino S, Bramanti P, Caminiti F. Parosmia and neurological disorders: a neglected association. Front Neurol. 2020;11. This study provides an important insight into the neurological disorders that may cause symptoms of parosmia.
Müller A, Landis BN, Platzbecker U, Holthoff V, Frasnelli J, Hummel T. Severe chemotherapy-induced parosmia. Am J Rhinol. 2006;20:485–6.
Emmett EA. Parosmia and hyposmia induced by solvent exposure. Occup Environ Med. 1976;33:196–8.
Croy I, Nordin S, Hummel T. Olfactory disorders and quality of life - an updated review. Chem Senses. 2014;39:185–94.
•• Lecuyer Giguere F, Jobin B, Robert J, Bastien L, Giguère J-F, De Beaumont L, et al. Early parosmia signs and affective states predict depression and anxiety symptoms 6 months after a mild traumatic brain injury. Chem Senses. 2020;45:483–90. This study showcases the negative effects qualitative olfactory disorders may have on patients’ mental health.
Jacek S, Stevenson RJ, Miller LA. Olfactory dysfunction in temporal lobe epilepsy: a case of ictus-related parosmia. Epilepsy Behav. 2007;11:466–70.
Lum C, Davidson MD. Parosmia after laparoscopic gastric bypass and gastric banding. J Am Osteopath Assoc. 2010;110:617–8.
•• Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-COV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604:697–707. This study summarizes very important findings on how COVID-19 infections affect the brain structure, potentially leading to qualitative olfactory disorders.
Moideen S, Innisai A, Uvais NA. Bilateral olfactory bulb atrophy in post–COVID-19 parosmia. Prim Care Companion CNS Disord. 2022;24.
Rashid RA, Alaqeedy AA, Al-Ani RM. Parosmia due to COVID-19 disease: a 268 case series. Indian J Otolaryngol Head Neck Surg. 2022 Oct;74(Suppl 2):2970-2977. https://doi.org/10.1007/s12070-021-02630-9.
Altundag A, Cayonu M, Kayabasoglu G, Salihoglu M, Tekeli H, Saglam O, et al. Modified olfactory training in patients with postinfectious olfactory loss. Laryngoscope. 2015;125:1763–6.
Altundag A, Yilmaz E, Kesimli MC. Modified olfactory training is an effective treatment method for COVID-19 induced parosmia. Laryngoscope. 2022;132:1433–8.
Liu DT, Sabha M, Damm M, Philpott C, Oleszkiewicz A, Hähner A, et al. Parosmia is associated with relevant olfactory recovery after olfactory training. Laryngoscope. 2020;131:618–23.
Duyan M, Ozturan IU, Altas M. Delayed parosmia following SARS-COV-2 infection: a rare late complication of COVID-19. SN Compr Clin Med. 2021;3:1200–2.
Bitter T, Siegert F, Gudziol H, Burmeister HP, Mentzel H-J, Hummel T, et al. Gray matter alterations in parosmia. Neuroscience. 2011;177:177–82.
Karimi-Galougahi M, Yousefi-Koma A, Bakhshayeshkaram M, Raad N, Haseli S. 18FDG pet/CT scan reveals hypoactive orbitofrontal cortex in anosmia of COVID-19. Acad Radiol. 2020;27:1042–3.
Shiga H, Okuda K, Taki J, Watanabe N, Tonami H, Kinuya S, et al. Nasal thallium-201 uptake in patients with parosmia with and without hyposmia after upper respiratory tract infection. Int Forum Allergy Rhinol. 2019;9:1252–6.
Philpott C, Dixon J, Boak D. Qualitative olfactory disorders: patient experiences and self-management. Allergy Rhinol. 2021;12:215265672110042.
Bonfils P, Avan P, Faulcon P, Malinvaud D. Distorted odorant perception. Archives of Otolaryngology-Head & Neck Surgery. 2005;131:107.
Parker JK, Kelly CE, Gane SB. Molecular mechanism of parosmia. MedRxiv. 2021. https://doi.org/10.1101/2021.02.05.21251085.
Parker JK, Methven L, Pellegrino R, Smith BC, Gane S, Kelly CE. Emerging pattern of post-COVID-19 parosmia and its effect on food perception. Foods. 2022;11:967.
Altundag A, Temirbekov D, Haci C, Yildirim D, Cayonu M. Olfactory cleft width and volume: possible risk factors for postinfectious olfactory dysfunction. Laryngoscope. 2020;131:5–9.
Altundag A, Yıldırım D, Tekcan Sanli DE, Cayonu M, Kandemirli SG, Sanli AN, et al. Olfactory cleft measurements and COVID-19–related anosmia. Otolaryngol-Head Neck Surg. 2020:019459982096592.
Tekcan Sanli DE, Altundag A, Yıldırım D, Kandemirli SG, Sanli AN. Comparison of olfactory cleft width and volumes in patients with COVID-19 anosmia and COVID-19 cases without anosmia. ORL. 2021;84:1–9.
Shelton JF, Shastri AJ, Fletez-Brant K, Auton A, Chubb A, Fitch A, et al. The UGT2A1/UGT2A2 locus is associated with COVID-19-related loss of smell or taste. Nat Genet. 2022;54:121–4.
Alrasheedi AN. Characterization, treatment modalities, and self-perceived improvement of post COVID-19 phantosmia: a case series of eleven patients. Rhinol Online. 2022;5:44–8.
Boscolo-Rizzo P, Hopkins C, Menini A, Dibattista M, Cancellieri E, Gardenal N, et al. Parosmia assessment with structured questions and its functional impact in patients with long-term COVID-19-related olfactory dysfunction. Int Forum Allergy Rhinol. 2022.
Iannilli E, Leopold DA, Hornung DE, Hummel T. Advances in understanding parosmia: an fMRI study. ORL. 2019;81:185–92.
Landis BN, Frasnelli J, Croy I, Hummel T. Evaluating the clinical usefulness of structured questions in parosmia assessment. Laryngoscope. 2010;120:1707–13.
Liu DT, Welge-Lüssen A, Besser G, Mueller CA, Renner B. Assessment of odor hedonic perception: the Sniffin’ Sticks Parosmia Test (SSParoT). Sci Rep. 2020;10.
Parker JK, Kelly CE, Gane SB. Insights into the molecular triggers of parosmia based on gas chromatography olfactometry. Commun Med. 2022;2.
Yildirim D, Kandemirli SG, Tekcan Sanli DE, Akinci O, Altundag A. A comparative olfactory MRI, DTI and fMRI study of COVID-19 related anosmia and post viral olfactory dysfunction. Acad Radiol. 2022;29:31–41.
Yousefi-Koma A, Haseli S, Bakhshayeshkaram M, Raad N, Karimi-Galougahi M. Multimodality imaging with PET/CT and MRI reveals hypometabolism in tertiary olfactory cortex in parosmia of COVID-19. Acad Radiol. 2021;28:749–51.
Philpott CM, Boardman J, Boak D. Patient experiences of postinfectious olfactory dysfunction. ORL. 2021;83:299–303.
Stevenson RJ. An initial evaluation of the functions of human olfaction. Chem Senses. 2009;35:3–20.
Ferris AM, Duffy VB. Effect of olfactory deficits on nutritional status: does age predict persons at risk? Ann N Y Acad Sci. 1989;561:113–23.
Fjaeldstad AW, Smith B. The effects of olfactory loss and parosmia on food and cooking habits, sensory awareness, and quality of life—a possible avenue for regaining enjoyment of food. Foods. 2022;11:1686.
Burges Watson DL, Campbell M, Hopkins C, Smith B, Kelly C, Deary V. Altered smell and taste: anosmia, parosmia and the impact of long COVID-19. Plos One. 2021;16.
Philpott CM, Boak D. The impact of olfactory disorders in the United Kingdom. Chem Senses. 2014;39:711–8.
Miwa T, Furukawa M, Tsukatani T, Costanzo RM, DiNardo LJ, Reiter ER. Impact of olfactory impairment on quality of life and disability. Arch Otolaryngol Head Neck Surg. 2001;127–497.
Liu J, Pinheiro-Neto CD, Zhao J, Chen Z, Wang Y. A novel surgical treatment for long lasting unilateral peripheral parosmia: olfactory cleft blocking technique. Auris Nasus Larynx. 2021;48:1209–13.
Maruani J, Geoffroy PA. Bright light as a personalized precision treatment of mood disorders. Front Psychiatry. 2019;10.
Kaufman MD, Lassiter KR, Vittal SB. Paroxysmal unilateral dysosmia: a cured patient. Ann Neurol. 1988;24:450–1.
Aiello SR, Hirsch AR. Phantosmia as a meteorological forecaster. Int J Biometeorol. 2013;57:813–5.
Corcoran C, Whitaker A, Coleman E, Fried J, Feldman J, Goudsmit N, et al. Olfactory deficits, cognition and negative symptoms in early onset psychosis. Schizophr Res. 2005;80:283–93.
Hirsch AR. Parkinsonism: the hyposmia and phantosmia connection. Arch Neurol. 2009;66:538.
Pause BM, Hellmann G, Göder R, Aldenhoff JB, Ferstl R. Increased processing speed for emotionally negative odors in schizophrenia. Int J Psychophysiol. 2008;70:16–22.
Turetsky BI, Hahn C-G, Borgmann-Winter K, Moberg PJ. Scents and nonsense: olfactory dysfunction in schizophrenia. Schizophr Bull. 2009;35:1117–31.
DiFabio R, Casali C, Giugni E, Pierelli F. Olfactory hallucinations as a manifestation of hidden rhinosinusitis. J Clin Neurosci. 2009;16:1353–5.
Kumar J, Murphy E, Gray S, Holbrook E, Curry W, Venteicher A. Phantosmia and dysgeusia following endoscopic transcribriform approaches to olfactory groove meningiomas. J Neurol Surg Part B: Skull Base. 2017;38:245–50.
Lötsch J, Ultsch A, Eckhardt M, Huart C, Rombaux P, Hummel T. Brain lesion-pattern analysis in patients with olfactory dysfunctions following head trauma. NeuroImage: Clin. 2016;11:99–105.
Yang JC, Khakoo Y, Lightner DD, Wolden SL. Phantosmia during radiation therapy. J Child Neurol. 2012;28:791–4.
İşlek A, Balcı MK. Phantosmia with COVID-19 related olfactory dysfunction: report of nine case. Indian J Otolaryngol Head Neck Surg. 2021:1–3.
Levy LM, Henkin RI. Brain gamma-aminobutyric acid levels are decreased in patients with phantageusia and phantosmia demonstrated by magnetic resonance spectroscopy. J Comput Assist Tomogr. 2004;28:721–7.
Levy LM, Henkin RI. Physiologically initiated and inhibited phantosmia: cyclic unirhinal, episodic, recurrent phantosmia revealed by brain fMRI. J Comput Assist Tomogr. 2000;24:501–20.
Ohla K, Veldhuizen MG, Green T, Hannum ME, Bakke AJ, Moein ST, et al. Increasing incidence of parosmia and phantosmia in patients recovering from COVID-19 smell loss. 2021.
Leopold DA, Loehrl TA, Schwob JE. Long-term follow-up of surgically treated phantosmia. Arch Otolaryngol Head Neck Surg. 2002;128:642.
Majumdar S, Jones NS, McKerrow WS, Scadding G. The management of idiopathic olfactory hallucinations: a study of two patients. Laryngoscope. 2003;113:879–81.
Morrissey DK, Pratap U, Brown C, Wormald P-J. The role of surgery in the management of phantosmia. Laryngoscope. 2015;126:575–8.
Landis BN, Croy I, Haehner A. Long lasting phantosmia treated with venlafaxine. Neurocase. 2012;18:112–4.
Muffatti R, Scarone S, Gambini O. An olfactory reference syndrome successfully treated by aripiprazole augmentation of antidepressant therapy. Cogn Behav Neurol. 2008;21:258–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on RHINOLOGY: Taste and Smell Disorders
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altundag, A. Parosmia and Phantosmia: Managing Quality Disorders. Curr Otorhinolaryngol Rep 11, 19–26 (2023). https://doi.org/10.1007/s40136-023-00441-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-023-00441-w