Abstract
Growing number of contact lens discomfort (CLD) and CL dropout incidence rate afflict the development of CL industry. This article analyzes literatures of past 5 years’ on studies of CLD. It reviews the epidemiology and mechanism of CLD, analyzes different characteristics of CLD resulting from CL material, contact lens care system, and wearers. It sketches the relationship between CLD and ocular surface microenvironment, pointing out that CLD is an incompatible status between CL and the ocular surface microenvironment. Literature analysis also reveals that while high-quality optical effect of rigid lens came at the price of unwelcome initial discomfort, soft lens wearing continuously changes the balance of ocular surface microenvironment, leading to time-dependent discomfort. Different components or formulas of contact lens care systems could be transited by CL into ocular surface and induce CLD. Personal features of wearers such as age, gender, race, and psychological state also could be considered as potential CLD risks.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Brennan NA, Efron N. Symptomatology of HEMA contact lens wear. Optom Vis Sci. 1989;66(12):834–8.
Guillon M, Maissa C. Dry eye symptomatology of soft contact lens wearers and nonwearers. Optom Vis Sci. 2005;82(9):829–34.
•• Young G, et al. Characterizing contact lens-related dryness symptoms in a cross-section of UK soft lens wearers. Contact Lens Anterior Eye. 2011;34(2):64–70. There were over 900 subjects invovled in the survey and the study used a new score, the Contact Lens Dry Eye Questionnaire (CLDEQ).
Rumpakis, J.: New data on contact lens dropouts: an international perspective. Rev Optom. http://www.revoptom.com/content/d/contact_lenses_and__solutions/c/18929/ (2010). Accessed 31 March 2013.
Asbell PA, Lemp MA. Dry eye disease. The clinicians guide to diagnosis and treatment. New York: Thieme Medical Publishers, Inc.; 2006.
Mathers WD. Why the eye becomes dry: a cornea and lacrimal gland feedback model. CLAO J. 2000;26(3):159–65.
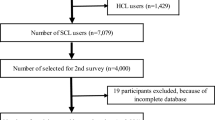
•• Dumbleton K, et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93–9. This article described a large study with over 4 thousand surveys, analyzing the impact of CLD on lens discontinuation.
Nichols KK, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS14–9.
• Mann A, Tighe B. Contact lens interactions with the tear film. Exp Eye Res. 2013;117:88–98. This article provides a comprhensive analysis about the interaction and impact of contact lens on tear physiology and biochemistry.
Doughty MJ. Contact lens wear and the goblet cells of the human conjunctiva—a review. Contact Lens Anterior Eye. 2011;34(4):157–63.
Fonn D, Peterson R, Woods C. Corneal staining as a response to contact lens wear. Eye Contact Lens. 2010;36(5):318–21.
Sindt CW, et al. Dendritic immune cell densities in the central cornea associated with soft contact lens types and lens care solution types: a pilot study. Clin Ophthalmol. 2012;6:511–9.
Villani E, et al. In vivo confocal microscopy of meibomian glands in contact lens wearers. Invest Ophthalmol Vis Sci. 2011;52(8):5215–9.
du Toit R, et al. The effects of six months of contact lens wear on the tear film, ocular surfaces, and symptoms of presbyopes. Optom Vis Sci. 2001;78(6):455–62.
Riley C, Young G, Chalmers R. Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: the effect of refitting with daily-wear silicone hydrogel lenses (senofilcon a). Eye Contact Lens. 2006;32(6):281–6.
• Chalmers RL, et al. Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8) and opinion of contact lens performance. Optom Vis Sci. 2012;89(10):1435–42. It reported the development and validation of a short form of the Contact Lens Dry Eye Questionnaire (the CLDEQ-8) as a outcome measure in soft contact lenses clinical trials.
The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75–92.
McCarty DJ, McCarty CA. Survey of dry eye symptoms in Australian pilots. Clin Exp Ophthalmol. 2000;28(3):169–71.
Begley CG, et al. Responses of contact lens wearers to a dry eye survey. Optom Vis Sci. 2000;77(1):40–6.
The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):93–107.
Dumbleton K, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the subcommittee on epidemiology. Invest Ophthalmol Vis Sci. 2013;54(11):20–36.
Efron N, Pearson RM. Centenary celebration of Fick’s Eine Contactbrille. Arch Ophthalmol. 1988;106(10):1370–7.
Pearson R. Contact lens trends in the United Kingdom in 1991. J Br Contact Lens Assoc. 1992;15:17–23.
•• Efron N, et al. International survey of rigid contact lens fitting. Optom Vis Sci. 2013;90(2):113–8. This report described analysis results of a very large survey with 40 paticipating countries and 12,230 rigid and 100,670 soft lens fits.
Morgan PB, Efron N. A decade of contact lens prescribing trends in the United Kingdom (1996–2005). Contact Lens Anterior Eye. 2006;29(2):59–68.
Efron N. Obituary-rigid contact lenses. Contact Lens Anterior Eye. 2010;33(5):245–52.
Stapleton F, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the subcommittee on neurobiology. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS71–97.
Chen J, Simpson TL. A role of corneal mechanical adaptation in contact lens-related dry eye symptoms. Invest Ophthalmol Vis Sci. 2011;52(3):1200–5.
Millodot M, Henson DB, O’Leary DJ. Measurement of corneal sensitivity and thickness with PMMA and gas-permeable contact lenses. Am J Optom Physiol Opt. 1979;56(10):628–32.
Truong TN, Graham AD, Lin MC. Factors in contact lens symptoms: evidence from a multistudy database. Optom Vis Sci. 2014;91(2):133–41.
Yanai R, et al. Disruption of zonula occludens-1 localization in the rabbit corneal epithelium by contact lens-induced hypoxia. Invest Ophthalmol Vis Sci. 2009;50(10):4605–10.
Ding H, et al. Changes in corneal biometry and the associated histology in rhesus monkeys wearing orthokeratology contact lenses. Cornea. 2012;31(8):926–33.
Carracedo G, Gonzalez-Meijome JM, Pintor J. Changes in diadenosine polyphosphates during alignment-fit and orthokeratology rigid gas permeable lens wear. Invest Ophthalmol Vis Sci. 2012;53(8):4426–32.
Bhatoa NS, Hau S, Ehrlich DP. A comparison of a topography-based rigid gas permeable contact lens design with a conventionally fitted lens in patients with keratoconus. Contact Lens Anterior Eye. 2010;33(3):128–35.
Morgan PB, Maldonado-Codina C, Efron N. Comfort response to rigid and soft hyper-transmissible contact lenses used for continuous wear. Eye Contact Lens. 2003;29(1 Suppl):S127–30 discussion S143–S144, S192–S194.
•• Efron N, et al. An international survey of daily disposable contact lens prescribing. Clin Exp Optom. 2013;96(1):58–64. This report described findings from a large international survey with 40 countries participated and data collected in relation to over 90,000 soft lens fits, of which 23,445 (24.1 per cent) were with daily disposable lenses and 73,170 (75.9 per cent) were with reusable lenses.
Lum E, et al. Corneal sensitivity with contact lenses of different mechanical properties. Optom Vis Sci. 2013;90(9):954–60.
Situ P, et al. Effects of silicone hydrogel contact lens wear on ocular surface sensitivity to tactile, pneumatic mechanical, and chemical stimulation. Invest Ophthalmol Vis Sci. 2010;51(12):6111–7.
Golebiowski B, Papas EB, Stapleton F. Corneal and conjunctival sensory function: the impact on ocular surface sensitivity of change from low to high oxygen transmissibility contact lenses. Invest Ophthalmol Vis Sci. 2012;53(3):1177–81.
Santodomingo-Rubido J, Barrado-Navascues E, Rubido-Crespo MJ. Ocular surface comfort during the day assessed by instant reporting in different types of contact and non-contact lens wearers. Eye Contact Lens. 2010;36(2):96–100.
Chen Q, et al. Tear menisci and ocular discomfort during daily contact lens wear in symptomatic wearers. Invest Ophthalmol Vis Sci. 2011;52(5):2175–80.
Arita R, et al. Contact lens wear is associated with decrease of meibomian glands. Ophthalmology. 2009;116(3):379–84.
Hong J, et al. Corneal epithelial thickness map in long-term soft contact lenses wearers. Optom Vis Sci. 2014;91(12):1455–61.
Jansen ME, et al. Effect of contact lens wear and a near task on tear film break-up. Optom Vis Sci. 2010;87(5):350–7.
Young G, et al. Soft contact lens-related dryness with and without clinical signs. Optom Vis Sci. 2012;89(8):1125–32.
Papas EB, et al. Consequences of wear interruption for discomfort with contact lenses. Optom Vis Sci. 2014;91(1):24–31.
Spyridon M, et al. Eye sensitivity in soft contact lens wearers. Optom Vis Sci. 2012;89(12):1682–90.
Sankaridurg P, Lazon de la Jara P, Holden B. The future of silicone hydrogels. Eye Contact Lens. 2013;39(1):125–9.
Szczesna-Iskander DH. Comparison of tear film surface quality measured in vivo on water gradient silicone hydrogel and hydrogel contact lenses. Eye Contact Lens. 2014;40(1):23–7.
Carney FP, Nash WL, Sentell KB. The adsorption of major tear film lipids in vitro to various silicone hydrogels over time. Invest Ophthalmol Vis Sci. 2008;49(1):120–4.
Maissa C, et al. Contact lens lipid spoliation of hydrogel and silicone hydrogel lenses. Optom Vis Sci. 2014;91(9):1071–83.
Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact lenses? Eye Contact Lens. 2013;39(1):86–92.
Dumbleton K, et al. Objective and subjective responses in patients refitted to daily-wear silicone hydrogel contact lenses. Optom Vis Sci. 2006;83(10):758–68.
Young G, et al. Hydrogel lens comfort in challenging environments and the effect of refitting with silicone hydrogel lenses. Optom Vis Sci. 2007;84(4):302–8.
Fonn D, Dumbleton K. Dryness and discomfort with silicone hydrogel contact lenses. Eye Contact Lens. 2003;29(1 Suppl):S101–4 discussion S115–S118, S192–S194.
Cheung SW, et al. A comparative study of biweekly disposable contact lenses: silicone hydrogel versus hydrogel. Clin Exp Optom. 2007;90(2):124–31.
Dalton K, et al. Physical properties of soft contact lens solutions. Optom Vis Sci. 2008;85(2):122–8.
Wilson LA, McNatt J, Reitschel R. Delayed hypersensitivity to thimerosal in soft contact lens wearers. Ophthalmology. 1981;88(8):804–9.
Wright P, Mackie I. Preservative-related problems in soft contact lens wearers. Trans Ophthalmol Soc U K. 1982;102(Pt 1):3–6.
Gorbet M, et al. Human corneal epithelial cell shedding and fluorescein staining in response to silicone hydrogel lenses and contact lens disinfecting solutions. Curr Eye Res. 2014;39(3):245–56.
Dutot M, et al. Multipurpose solutions and contact lens: modulation of cytotoxicity and apoptosis on the ocular surface. Cornea. 2010;29(5):541–9.
Teo L, et al. A survey of contact lens complications in Singapore. Eye Contact Lens. 2011;37(1):16–9.
Yang SN, et al. Comparative effect of lens care solutions on blink rate, ocular discomfort and visual performance. Ophthalmic Physiol Opt. 2012;32(5):412–20.
White CJ, Thomas CR, Byrne ME. Bringing comfort to the masses: a novel evaluation of comfort agent solution properties. Contact Lens Anterior Eye. 2014;37(2):81–91.
McMonnies CW. Hand hygiene prior to contact lens handling is problematical. Contact Lens Anterior Eye. 2012;35(2):65–70.
Thakur DV, Gaikwad UN. Microbial contamination of soft contact lenses & accessories in asymptomatic contact lens users. Indian J Med Res. 2014;140(2):307–9.
Morgan PB, et al. An international analysis of contact lens compliance. Contact Lens Anterior Eye. 2011;34(5):223–8.
Vijay AK, et al. Contact lens storage case hygiene practice and storage case contamination. Eye Contact Lens. 2015;41(2):91–7.
Murphy PJ, et al. Noninvasive assessment of corneal sensitivity in young and elderly diabetic and nondiabetic subjects. Invest Ophthalmol Vis Sci. 2004;45(6):1737–42.
Acosta MC, et al. Influence of age, gender and iris color on mechanical and chemical sensitivity of the cornea and conjunctiva. Exp Eye Res. 2006;83(4):932–8.
Chalmers RL, et al. Struggle with hydrogel CL wear increases with age in young adults. Contact Lens Anterior Eye. 2009;32(3):113–9.
Nichols JJ, Sinnott LT. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006;47(4):1319–28.
Richdale K, et al. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26(2):168–74.
Rahman MO, Liu J. Gender differences in functioning for older adults in rural Bangladesh. The impact of differential reporting? J Gerontol A Biol Sci Med Sci. 2000;55(1):M28–33.
McMonnies CW. Psychological and other mechanisms for end-of-day soft lens symptoms. Optom Vis Sci. 2013;90(6):e175–81.
McMonnies CW. How contact lens comfort may be influenced by psychiatric and psychological conditions and mechanisms. Clin Exp Optom. 2014;97(4):308–10.
Disclosure
The authors of this paper all declare they have no conflicts of interests.
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Contact Lens Discomfort.
Rights and permissions
About this article
Cite this article
Chen, J., Xiao, X. & Huang, JF. Contact Lens Discomfort and Dropout. What is it? Epidemiology. Curr Ophthalmol Rep 3, 98–105 (2015). https://doi.org/10.1007/s40135-015-0068-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40135-015-0068-6